Research Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2017) Volume 7, Issue 60
Laparoscopic Sleeve Gastrectomy, as an Ultimate Intervention for Fatness Treatment, Make Improved Physiological Changes in Obese Patients
Mustafa Erol and Nazim Gures*
Department of General Surgery, Ataturk State Hospital, Balikesir, Turkey
- *Corresponding Author:
- Nazim Gures
General Surgery Department, Turkey
Accepted date: January 15, 2017
Abstract
Background: Obesity and related comorbidities such as diabetes, coronary heart diseases and nonalcoholic fatty liver are both health and socioeconomically problem worldwide. Determining an appropriate treatment of morbid obesity is a multidisciplinary approach. In recent years, Laparoscopic Sleeve Gastrectomy (LSG) has become the first choice of surgical treatment for the morbid obesity patients resistant to the traditional diet methods, exercise and medications. Material and methods: We retrospectively analyzed the results of first 100 consecutive cases underwent LSG between January 2015 and January 2016 in our center. Patient demographics (age, gender) were recorded and Patient’s body mass indexes (BMI), fasting blood sugar (FBS), Lipid parameter (LDL, HDL) levels, Liver Enzyme (AST, ALT) levels, Blood Pressures and other comorbidities were compared between one week before and after six months of surgery. Surgical complications were also recorded. Results: BMIs, Levels of FBS, blood pressure, liver enzymes and lipid profile components significantly reduced (P<0.05). Comorbid conditions like hypertension, obstructive sleep apnea, mostly resolved or improved. A case of leakage resulted in pelvic abscess; laparotomy and drainage was performed. Another leakage gave rise to the gastrobronchial fistula which couldn’t be corrected by endoscopic methods. Patient finally underwent thoracotomy and lung segmentectomy. One patient had micro anastomotic leak and was observed nonoperatively. No mortality occurred. Conclusion: Although it may cause some major complications, LSG is effective operation to treat morbid obese patients. Comorbid conditions fastly resolve even within the months, synchronous with the weight loss.
Keywords
Sleeve, Obesity, Series, Laparoscopy, Gastrectomy
Introduction
Gluttony is one of the seven capital sins according to Christian theology. Obesity is now known to be complex result of psychological, endocrinological abnormalities and regarded as chronic, biological, preventable, and treatable disease [1,2]. Obesity decreases the quality of life and life expectancy [3] and bariatric/metabolic surgery has been shown to be the most effective and durable therapy for the treatment of morbid obese patients [4]. Laparoscopic Sleeve Gastrectomy, the current gold standard technique in bariatric surgery, is now a choice for the patients and surgeons worldwide by its superior excess weight loss, low complication rate, and excellent food tolerance, combined with a short hospital stay [5,6].
Herein, we reviewed the short term results of our initial experience with LSG. We also would like to emphasize the applicability of the procedure in a secondary medical center.
Material and Method
In one year period of time, from January 2015 to January 2016, 100 consecutive patients underwent LSG. Of the patients, 64 were female and 36 were male and their ages varied between 21 to 64. All the patients had over 35 BMI and have already been resistant to the diet methods, exercise and medications, were referred by same endocrinologist to the General Surgery Clinic. All the patients were carefully examinated by a specialist team consist of General Surgeon, endocrinologist, anaesthesiologist, pulmonologist, psychiatrist and cardiologist before the operation. They were screened preoperatively (Blood Pressure, blood count, routine biochemical tests including lipid profile, fasting blood sugar and chest x-ray). Operations were performed by the same team and the leading surgeon. Operational time was recorded.
Surgical technique
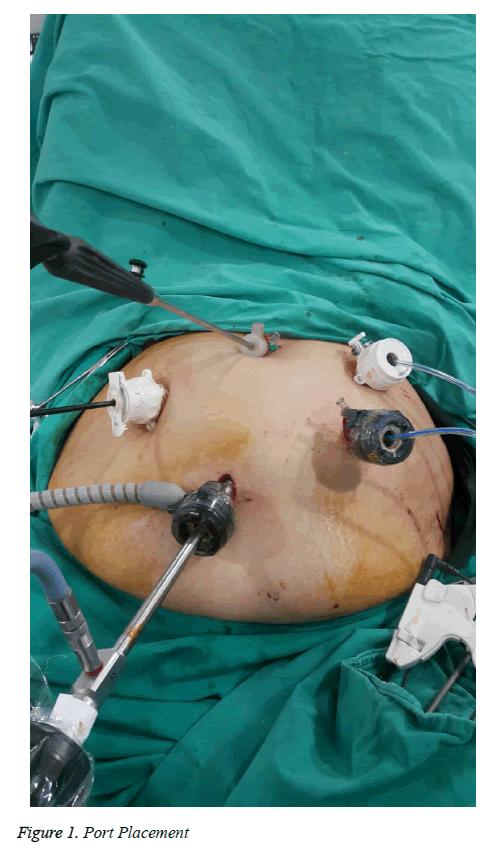
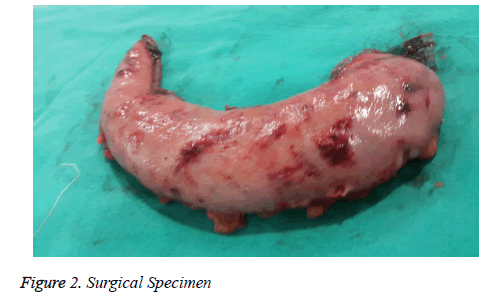
Under general anesthesia, five trocars were inserted: a supraumblical 12 mm optical, two 5/12 mm right and left superolateral to the umbilicus and two 5 mm epigastric (Figure 1). Liberalization of the greater curvature was carried out upwards, starting from the point of 4 cm superior to the pylorus up to the left crura. A 36 F tube was inserted from the mouth to mark the stapler line. Endo GIA (Gastrointestinal Anastomosis Stapler) was used for the longitudinal stapling of the greater curvature towards to Angle of His. Specimen was retracted from the abdomen through 12 mm trocar (Figure 2).
Postoperative follow-up
Patients were observed in the Intensive Care Unit on the day of Surgery. Oral liquids were started on postoperative day two. After the patients were able to tolerate soft foods they were discharged. They were called to our outpatient clinic for the follow-up program by the periods of 10 days, 1 month, 3 months and 6 months after surgery. Routine biochemical tests and patient’s actual weights were also registered during these visits. In this study, results of the 6 month’s tests and BMI’s were compared to the results prior to the surgery. The patients were also questionnaired for the severity of the obesity-related symptoms (joint pains, sleep apnea, etc) that they had before the surgery.
Statistical analysis
In order to compare means, paired-sample t-test, using the SPSS, Version 19 (Chicago, IL) was used.
Results
The mean age of the male patients was 36.1 ± 12 and female patients were 33.2 ± 11. Mean BMI of the males was higher than the females (Table 1, Demographic Data).
| Variable | Female | Male | p |
|---|---|---|---|
| Patient | 64 | 36 | |
| Age (mean+SD) | 36.1 ± 12 | 36.1 ± 12 | 0.657 |
| BMI (mean+SD) | 47.1 ± 4 | 47.1 ± 4 | 0.426 |
SD: Standard Deviation, BMI: Body Mass Index
Table 1: Patient’s Demographics
Serum levels of all the parameters ( FBS, LDL, HDL, AST and ALT levels) were measured in an automated system by using commercially available kits (Cobas system, Roche Diagnostics, Mannheim, Germany). All the biochemical values (FBS, LDL, HDL, TG, AST, ALT) reduced at the end of the six months when compared to baseline values (Table 2). Patients weights and BMI’s are also significantly lower than the baseline (P<0.05) (Table 3).
| Baseline | 6 months After Surgery | P | |
|---|---|---|---|
| FBS | 102.6 ± 12.3 | 86 ± 9.6 | 0.0001* |
| LDL | 132.2±24.2 | 108 ± 18.8 | 0.0001* |
| HDL | 40.3±7.2 | 45.6 ±6.4 | 0.001* |
| TG | 190.2 ±70.2 | 132.6 ± 47.7 | 0.0001* |
| ALT | 38.9 ±8.9 | 27.9 ± 5.7 | 0.0001* |
| AST | 28.6±8.3 | 21.1 ± 5.9 | 0.0001* |
FBS: Fasting Blood Sugar; LDL: Low Density Lipoprotein; HDL: High Density Lipoprotein; TG: Triglyceride; AST: Aspartate Transaminase ALT: Alanine Transaminase
Table 2: Biochemical Values (mean+SD)
| Baseline | 6 months | p | |
|---|---|---|---|
| BMI Alterations (mean + SD)45.6 ±4.5 | 45.6 ±4.5 | 30.4 ± 5.2 |
Table 3: BMI Alterations (mean + SD)
EWL (excess weight loss) of the patients at the end of the six months 65.3 ± 18.3% (mean ± SD)
Median operative time is 55 minutes (range 35 to 120 min)
Comorbid conditions mostly resolved, at least improved at the end of the six months (Table 4).
| Postoperative | ||||
|---|---|---|---|---|
| Preoperative | Resolved | Improved | Unchanged | |
| Hypertension | 40 | 32 | 8 | 0 |
| Type 2 Diabetes Mellitus/Insulin Dependent | 10/6 | 6/2 | 4/3 | 0/1 |
| Obstructive Sleep Apnea | 12 | 12 | 0 | 0 |
| Depression / Anxiety | 15 | 2 | 10 | 3 |
| Knee / Hip Pain | 22 | 6 | 16 | 0 |
Table 4: Comorbidities (number of patients)
Two major complications occurred. A pelvic abscess was seen after 35 days of surgery and laparotomy and drainage needed for this patient. Another case presented with a gastrobronchial fistula underwent lung segmentectomy after endobronchial stenting attempts failed. One patient had microanastomotic leak treated with antibiotics and cessation of oral intake and leak regressed nonoperatively (Table 5).
| Number of Patients | Result | |
|---|---|---|
| Pelvic Abscess | 1 | Laparotomy + Drenaige |
| Gastrobronchial Fistula | 1 | Lung Segmentectomy |
| Microanostomotic Leak | 1 | Nonoperative Treatment |
Table 5: Surgical Complications
Discussion
Today, Bariatric surgery is known the most effective and durable therapy for the treatment of morbid obese patients. Among the bariatric surgery procedures, LSG, is becoming the leading bariatric surgery procedure, because of its simplicity and efficacy [4,5].
While starting, we knew that the learning curve of 50-100 cases for gaining proficiency and reducing the complication rates for laparoscopic bariatric surgery was suggested in the literature [7]. We are agreeing that to be familiarized with the laparoscopic surgery is also essential before starting the procedure. Particularly, laparoscopic manipulation skills and experience is crucial to have good result in superobese patient group (BMI>60). Operational time significantly reduced from almost two hours for the first case to even 35 minutes for some cases by the time and experience.
Our six-months fallow-up results are compatible with the literature [3,4,6-9]; FBS, lipid disturbance, liver function tests were all improved. Lemanu et al. reported FBS and related HbA1c had been significantly reduced after 5 years-long term fallow-up. Studies support the decrease of the LDL and Total Cholestrol levels; but the effect seems limited by the long term [11,12]. Yildiz et al. urged the effects of LSG on the nonwestern population and they founded that LSG is highly efficient to ameliorate the hypertension, hyperlypidemia, and diabetes mellitus [13]. The fact that, there is a study from Iran made up of short outcomes of their LSG series which has very similar results with our patient group [14] may be raised from the close relationship, genetic pool and eating habits between neighboring two countries. Two-years follow-up study from Greece , another neighboring country of Turkey, exhibits that diabetes mellitus, hypertension, and hyperlipidemia were diminished gradually at 6 months postoperatively, as well [15].
Stress and depressive symptoms were also lessened almost all of the patients suffered [16,17]. They felt more reconciled with their body image. Losing weight leads to increasing activity of the patient that means more serotonin production [18].
Interestingly, all the patients with obstructive sleep apnea symptoms quit to use Continuous Positive Airway Pressure (CPAP) and described better sleep quality, even within 6 months harmonious with the weight loss [19]. LSG is also effective treatment to relieve joint pain which is prominent on the large joints as hip and knee [20].
Postoperative leakage ranges in the literature between 1.1 and 5.3% [21] but an Israeli study reported as low as 0.83% in their 3003 cases series [22]. They also reported only one case of intraabdominal abscess that is already one in our series. Staple line reinforcement (SLR) is reported superior to no enforcement [23]; hence, we preferred SLR for our patients. Endobronchial fistula is a quite rare complication of LSG and surgical intervention might be needed [24].
Conclusion
LSG seems very effective weight loss treatment even within the short period after the surgery. Besides improvement in biochemical parameters, resolution of comorbid conditions of the patients can be striking. Increasing self-confidence and social activity of the patients another point that can easily be realized while their routine out-patient clinic controls. We also concluded that LSG can be feasible surgical procedure for a secondary health care hospital’s general surgery clinic with careful preoperative and postoperative evaluation of the patients.
References
- Konttinen H, Peltonen M, Sjöström L, Carlsson L, Karlsson J. Psychological aspects of eating behavior as predictors of 10-y weight changes after Surgical and conventional treatment of severe obesity: results from the Swedish Obese Subjects intervention study. Am J Clin Nutr. 2015; 101:16-24.
- Gonzalez-Campoy JM, Richardson B, Richardson C, Gonzalez-Cameron D, Ebrahim A,Strobel P, Martinez T, Blaha B, Ransom M, Quinonez-Weislow J, Pierson A, Gonzalez Ahumada M. Bariatric endocrinology: principles of medical practice. Int J Endocrinol. 2014; 2014: 917813.
- Giordano S, Victorzon M. Bariatric Surg ery in elderly patients: a systematic review. Clin Interv Aging. 2015; 10: 1627-1635.
- Lee WJ, Almulaifi A. Recent advances in bariatric/metabolic Surg ery: appraisal of clinical evidence. J Biomed Res. 2015; 29: 98-104.
- Benaiges D, Más-Lorenzo A, Goday A, Ramon JM, Chillarón JJ, Pedro-BotetJ,Flores-Le Roux JA. Laparoscopic sleeve gastrectomy: More than a restrictive bariatric Surg ery procedure? World J Gastroenterol. 2015; 21:11804-14.
- Shabbir A, Dargan D. The success of sleeve gastrectomy in the management of metabolic syndrome and obesity. J Biomed Res. 2015; 29: 93-97.
- Dey A, Mittal T, Malik VK. Initial experience with laparoscopic sleeve gastrectomy by a novice bariatric team in an established bariatric center-a review of literature and initial results. Obes Surg. 2013; 23: 541-7.
- Catheline JM, Fysekidis M, Dbouk R, Boschetto A, Bihan H, et al. Weight loss after sleeve gastrectomy in super superobesity. J Obes. 2012; 2012: 959260.
- Svane MS, Madsbad S. Bariatric Surg ery - effects on obesity and related co-morbidities. Curr Diabetes Rev. 2014; 10: 208-214.
- Lemanu DP, Singh PP, Rahman H, Hill AG, Babor R, MacCormick AD. Five-year results after laparoscopic sleeve gastrectomy: a prospective study. Surg Obes Relat Dis. 2015; 11: 518-24.
- Strain GW, Saif T, Ebel F, Dakin GF, Gagner M, Costa R, Chiu YL, Pomp A. Lipid profile changes in the severely obese after laparoscopic sleeve gastrectomy(LSG), 1, 3, and 5 years after Surg ery. Obes Surg. 2015; 25: 285-289.
- Zhang F, Strain GW, Lei W, Dakin GF, Gagner M, Pomp A. Changes in lipid profiles in morbidly obese patients after laparoscopic sleeve gastrectomy (LSG). Obes Surg. 2011; 21: 305-9.
- Yildiz B, Katar K, Hamamci O. Efficacy of laparoscopic sleeve gastrectomy for the treatment of obesity in a non-Western society. Eat Weight Disord. 2016; 21: 695-699.
- Keleidari B, Mahmoudie M, Anaraki AG, Shahraki MS, Jamalouee SD. Six month-follow up of laparoscopic sleeve gastrectomy. Adv Biomed Res. 2016; 5: 49.
- Tsamis D, Plastiras A, Natoudi M, Oikonomou E, Zografos G, LeandrosE,Albanopoulos K. Impact of Laparoscopic Sleeve Gastrectomy on Weight Loss and Associated Comorbidities in Adolescents and Young Adults. J Laparoendosc Adv Surg Tech A. 2015; 25: 971-5.
- Mack I, Ölschläger S, Sauer H, von Feilitzsch M, Weimer K, Junne F, Peeraully R, Enck P, Zipfel S, Teufel M. Does Laparoscopic Sleeve Gastrectomy Improve Depression, Stress and Eating Behaviour? A 4-Year Follow-up Study. Obes Surg. 2016.
- Ayloo S, Thompson K, Choudhury N, Sheriffdeen R. Correlation between the Beck Depression Inventory and bariatric Surgical procedures. Surg Obes Relat Dis. 2015; 11: 637-642.
- Heijnen S, Hommel B, Kibele A, Colzato LS. Neuromodulation of Aerobic Exercise-A Review. Front Psychol. 2016; 6: 1890.
- Dilektasli E, Dilektasli AG. Laparoscopic Sleeve Gastrectomy Improves Excessive Daytime Sleepiness and Sleep Quality 6 Months Following Surg ery: A Prospective Cohort Study. Adv Ther. 2016; 33:774-785.
- Çak?r T, Oruç MT, Aslaner A, Duygun F, Yard?mc? EC, Mayir B, Bülbüller N. The effects of laparoscopic sleeve gastrectomy on head, neck, shoulder, low back and knee pain of female patients. Int J Clin Exp Med. 2015; 8: 2668-2673.
- Iossa A, Abdelgawad M, Watkins BM, Silecchia G. Leaks after laparoscopic sleeve gastrectomy: overview of pathogenesis and risk factors. Langenbecks Arch Surg. 2016.
- Sakran N, Raziel A, Goitein O. Laparoscopic Sleeve Gastrectomy for Morbid Obesity in 3003 Patients: Results at a High-Volume Bariatric Center. Obes Surg. 2016; 26: 2045-2050.
- Shikora SA, Mahoney CB. Clinical Benefit of Gastric Staple Line Reinforcement (SLR) in Gastrointestinal Surg ery: a Meta-analysis. Obes Surg. 2015; 25: 1133-1141.
- Silva LB, Moon RC, Teixeira AF, Jawad MA, Ferraz ÁA. Gastrobronchial Fistula in Sleeve Gastrectomy and Roux-en-Y Gastric Bypass--A Systematic Review. Obes Surg. 2015; 25: 1959-1965.