Research Article - Journal of Public Health Policy and Planning (2023) Volume 7, Issue 5
Knowledge, risk factors and perceived attitude towards cervical cancer among female tertiary students in the Tano-north municipality of the Ahafo region of Ghana.
Philip Narteh Gorleku1*, Jacob Setorglo2, Sebastian Ken Amoah3, Albert Piersson4, Wasiya Mutawakilu5
1Department of Medical Imaging, P.M.B. University of Cape Coast, Cape Coast, Ghana
2Department of Medical Biochemistry, P.M.B. University of Cape Coast, Cape Coast, Ghana
3Department of Obstetrics and Gynaecology, P.M.B. University of Cape Coast, Cape Coast, Ghana
4Department of Imaging Technology and Sonography, P.M.B. University of Cape Coast, Cape Coast, Ghana
5Department of Community Medicine, College of Health, Yamfo, Ghana
- Corresponding Author:
- Philip Narteh Gorleku
Department of Medical Imaging,
P.M.B. University of Cape Coast,
Cape Coast,
Ghana;
E-mail: madhab_jena@rediffmail.com
Received: 11-Sep-2019, Manuscript No. AAPHPP-23-2405; Editor assigned: 16-Sep-2019, PreQC No. AAPHPP-23-2405 (PQ); Reviewed: 30-Sep-2019, QC No. AAPHPP-23-2405; Revised: 13-Sep-2023, Manuscript No. AAPHPP-23-2405 (R); Published: 11-Oct-2023, DOI: 10.35841/aaphpp-7.5.195
Citation: Gorleku PN, Setorglo J, Amoah SK, et al. Knowledge, risk factors and perceived attitude towards cervical cancer among female tertiary students in the Tano-north municipality of the Ahafo region of Ghana. J Public Health Policy Plan. 2023;7(5):195
Abstract
Ghana is one of the countries with high incidence rate of cervical cancer in the world. Knowledge of the risk factors and the etiology of cancers, especially, cervical cancer leads to reduction in cancer incidence and prevalence. This study assesses the knowledge, risk factors and perceived preventive methods about cervical cancer of tertiary students in the Tano-north municipality of the newly created Ahafo region of Ghana. A structured questionnaire was used to collect data on socio-demographics, knowledge, risk factors and perceived preventive methods of 150 students who were randomly sampled. An in-depth interview was used to collect the information. Data were entered and analysed using SPSS v20. Proportions were presented for knowledge, risk factor and preventive factor variables. The age range was between 15 to 35 years with the 18-35-year bracket constituting 82.7% of respondents. A total of 59.3% of respondents were not aware that, early sexual intercourse is a risk factor and 78%, 64% and 90.7% of the respondents did not know that smoking cigarette, use of oral contraceptives and stress, respectively are risks of cervical cancer. Respondents also showed poor knowledge on preventive methods with only 32%, 25%, 24%, 57.3% and 34% acknowledged that delay in age of first sexual contact, regular exercise, non-smoking, HPV vaccine and pap smear respectively were preventive methods of cervical cancer. A total of 96.7% of the respondents were aware of cervical cancer disease with 87.6% stating that it is caused by HPV. Also, 66.9% knew pap smear was a screening test for cervical cancer but only 8.3% had ever done pap smear test. In conclusion it was observed that, respondents displayed poor knowledge about the risk factors and preventive methods of cervical cancer. The government should therefore develop and incorporate into the NHIS, a policy on free screening of young tertiary students for cervical cancer since willingness to screen was found to be high.
Keywords
Cervical cancer, Pap smear, Human papilloma virus, Risk factors, Preventive methods.
Introduction
Cervical cancer or carcinoma of the cervix uteri is a malignant neoplasm of the cervical area of the uterus caused by the Human Papilloma Virus (HPV) as the virus DNA is found in 99.7% of all cervical cancers.
Cervical cancer is preventable and in most cases, curable, if identified in its early stages mostly through screening programmes which have been instituted in some countries. Global Cancer (GLOBOCAN) report puts cervical cancer in both incidence and mortality, as the fourth most prevalent cancer among women with an estimated 570,000 of new cases diagnosed worldwide in 2018 which represents 6.6% of all female cancers. According to the World Health Organization (WHO), approximately 90% of deaths from cervical cancer occur in low and middle-income countries [1].
In West Africa, out of the 31,955 new cases of cervical cancer reported in 2018, Ghana alone accounted for 3,151 new cases out of which there were 2,119 mortalities. Cervical cancer is the leading cause of death among the gynaecological cancers in Ghana due to the higher rate of illiteracy, absence of national screening programme and most women are not financially endowed.
Even though the incidence of cervical cancer is high in Ghana accurate data of the disease is non-existent. The idea to collect, store and analyse data on people living with cancer is to provide accurate, complete and timely cancer report for interventional programmes. Such information would serve as a guide to monitor patient care, assist in the efficient and effective allocation of scarce health resources and act as a driving force for policy development which is needed for a comprehensive cancer control in Ghana. There are currently only two cancer registries in Ghana at the Korle-Bu and Komfo Anokye teaching hospitals which are located in the Ashanti and greater Accra regions of Ghana. This is because these are tertiary hospitals and referral centres for all cancer cases including cervical cancer in the country [2].
Currently in Ghana, there are only three health institutions where one can receive treatment for cancers, Sweden Ghana medical centre, Korle-Bu and Komfo Anokye teaching hospitals in Accra and Kumasi respectively. The cost of cervical cancer treatment in Ghana as at 2015, was about one thousand, five hundred Ghana cedis (GHS 1,500), equivalent to about two hundred and seventy-four United States Dollars, (USD 274) per week for radiotherapy and GHS 155 (USD 29) for chemotherapy. This means that with the exclusion of other auxiliary costs, a patient need about six thousand six hundred and thirty-five Ghana cedis GHS 6,635 (USD 1,212) monthly to get the needed treatment and this amount is far above the total monthly income of an average Ghanaian. This makes it difficult for individuals suffering from cancer to seek medical care. Low knowledge of cancer by patients together with their families and undefined referral patterns due to suspicion of cancer diagnosis leads to late presentation at the treatment centres. Unfortunately at the imaging department of the hospital we observe a lot of late stage of presentation which goes beyond educational levels and is compounded by cultural practices, beliefs and the widespread use of alternative medicine. People spend money and a lot of resources on radiotherapy and other forms of treatment, family members may tend to ignore people with cervical cancer making them a burden to the health facility and the community (where support is sometimes sought from community members to help in treating the patient). Although there is no formal cancer registry in Ghana, the International Agency for Research on Cancer has estimated that in 2018, there were 22,823 new cases of cancer with 15,089 deaths. As mentioned earlier, out of this figure, 3,151 Ghanaian women developed cervical cancer with more than 2,119 deaths as a result of the disease. Despite these staggering statistics, cervical cancer prevention is not commonly promoted in Ghana. The after effects of past investigations demonstrate that in Ghana, awareness on cervical cancer and HPV is to a large extent very low even among women with advanced education.
This study therefore seeks to assess the knowledge, risk factors and perceived preventive methods of cervical cancer among tertiary students in the Tano-north municipality of the newly created Ahafo region of Ghana [3].
Materials and Methods
This was a cross-sectional survey comprising 150 female students. They were sampled randomly from a tertiary institution in the Tano-north municipality in the Ahafo region of Ghana. A structured questionnaire was used for the study to capture information on demographics of respondents as well as their knowledge, perceived risk factors associated and perceived preventive methods about cervical cancer. Five variables: Age of respondents, religious affiliation, educational level, ethnicity and marital status were considered for sociodemographic characteristics. Regarding knowledge, causal knowledge (five questions), knowledge of diagnosis (six questions) and knowledge of treatment and prevention (eight questions). Factors considered in perceived risk of cervical cancer (eight statements to which respondents responded a ‘yes’ or ‘no’); perceived prevention method cervical cancer (six statements, responded ‘yes’ or ‘no’). The data obtained was entered and analyzed using the Statistical Package for Social Science (SPSS v.20). Proportions were presented for categorical variables [4].
Results
Demographic characteristics
The demographic characteristics of the 150 female respondents were presented in Table 1. The sample comprised of only women since the study purposefully enrolled women aged 18 to 35 years. Majority (92.7%) of the respondents were Christians followed by Muslims who constituted 7.3% of the total sample for the study. Regarding ethnicity, 83.3% of the respondents are Akans followed by Ewes constituting 5.3%. For the respondent’s highest level of education, 75.3% had obtained tertiary level certificates, 17.3% had attained diploma. Regarding the marital status of respondents, it was established that, majority (90%) of respondents are single [5].
| Variables | Frequency | Percentage |
|---|---|---|
| Age (years) | ||
| 15-17 | 6 | 4 |
| 18-25 | 124 | 82.7 |
| 26-35 | 20 | 13.3 |
| Total | 150 | 100 |
| Religion | ||
| Christian | 139 | 92.7 |
| Muslim | 11 | 7.3 |
| Total | 150 | 100 |
| Ethinicity | ||
| Akan | 125 | 83.3 |
| Ewe | 8 | 5.3 |
| Ga-Adangbe | 3 | 2 |
| Dagbani | 5 | 3.3 |
| Gurma | 2 | 1.3 |
| Guan | 1 | 0.7 |
| Others | 6 | 4 |
| Total | 150 | 100 |
| Level of education | ||
| Degree | 10 | 6.7 |
| Diploma | 26 | 17.3 |
| Certificate | 113 | 75.3 |
| Other | 1 | 0.7 |
| Total | 150 | 100 |
| Marital status | ||
| Single | 135 | 90 |
| Married | 14 | 9.3 |
| Cohabiting | 1 | 0.7 |
| Total | 150 | 100 |
Table 1. Socio-demographic characteristic of respondents.
Knowledge about cervical cancer
Table 2 shows results of level of knowledge on the causes, diagnosis, prevention and treatment of cervical cancer. Majority (96.7%) of the respondents have heard about cervical cancer with 41.4% indicated to have got the information from a health worker. About, 67.7% agreed that been sexually active at an early age can cause cervical cancer and 88.2% knew cervical cancer is caused by a virus called Human Papilloma Virus (HPV). On the knowledge of diagnosis of cervical cancer, out of the 150 respondents, only 68.3% knew pap smear is a test to look for abnormal cancer cells and 8.5% reported that it is a test to see if one has chlamydia or gonorrhoea. About 37.0% reported that a pap smear test should be done at least twice in a year and 34.9% did not know the frequency at which the test should be done. For treatment and prevention, 80% of the respondents were aware of cervical cancer screening with 92.4% knowing that cervical cancer is preventable. Also 63.5% of the respondents were aware that there is a vaccine for the prevention of cervical cancer, 89.7% believed, only women above the age of 30 years should be screened for cervical cancer. It was also observed that, 16.6% of the respondents believed one does not need pap smear after cervical cancer vaccination while majority (95.2%) think that a woman can get cervical cancer through deep kissing. Furthermore, 88.3% of the respondents believed too much of exposure to sunlight can cause cervical cancer while only 38.6% think that cervical cancer is common only among women in their 20s [6].
| Statements of casual knowledge | Frequency (n) | Percentage (%) |
|---|---|---|
| Have you ever heard about cancer of the cervix? | 145 | 96.7 |
| If yes, the source of information | ||
| Friend | 19 | 13.1 |
| Health worker | 60 | 41.4 |
| Television | 26 | 17.9 |
| Radio | 13 | 9 |
| Internet | 26 | 17.9 |
| Newspaper | 1 | 0.7 |
| Total | 145 | 100 |
| Sexually active at early age can cause cervix cancer | 100 | 69 |
| Cervical cancer is caused by a virus called Human Papilloma Virus (HPV) | 127 | 87.6 |
| Condom can’t prevent fully the transmission of HPV | 103 | 71 |
| Knowledge of diagnosis | ||
| Pap smear is a test to look for abnormal cancer cells/cancer of the cervix | 97 | 66.9 |
| I have never had a pap test taken | 123 | 84.8 |
| I have had pap tests, but not regularly | 12 | 8.3 |
| I have pap tests regularly (about every 2 years) | 7 | 4.8 |
| How often do you think you need to do pap test at least twice a year | 54 | 37.2 |
| Knowledge of treatment and prevention | ||
| Have you ever heard about screening tests for cervical cancer? | 116 | 80 |
| Is cancer of the cervix preventable? | 134 | 92.4 |
| Is there a vaccine available that prevents cervical cancer? | 92 | 63.5 |
| Do you think women above 30 years need to be screened for cervical cancer? | 130 | 89.7 |
| One will no longer need to have pap smears after the vaccine? | 24 | 16.6 |
| Can one get cervical cancer from deep kissing? | 138 | 95.2 |
| Can too much sun exposure lead to cervical cancer? | 128 | 88.3 |
| Cervical cancer is most common for women in their 20s? | 56 | 38.6 |
Table 2. Respondents’ knowledge about cervical cancer.
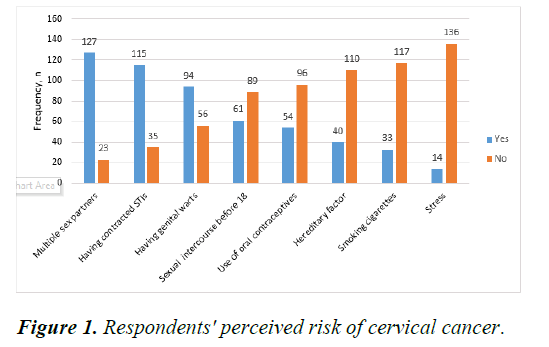
Perceived risks of cervical cancer
Figure 1 gives a summary of the perceived risks of cervical cancer among female tertiary students. It was observed that, 127 representing 84.7% of the respondents mentioned multiple sex partners as a risk factor associated with cervical cancer, while only 40.7% reported sexual intercourse before the age of 18 years was a risk. Also 76.7% said having contracted Sexually Transmitted Infections (STIs) poses a risk to a female to getting cervical cancer and 62.7% agreed having genital warts to be also an associating factor. The remaining respondents either indicated other factors such as use of contraceptives and stress as an associated factor or did not answer at all as shown in Figure 1.
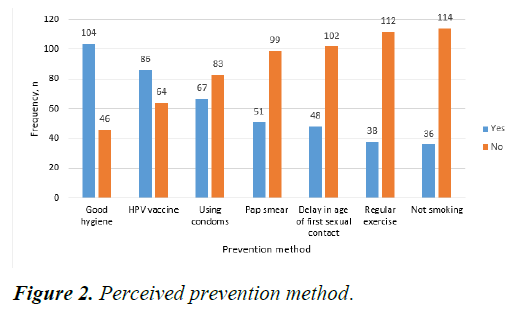
Perceived prevention method cervical cancer
Figure 2 presents a summary of preventive measures of cervical cancer. Majority (69.3%) of the respondents knew about HPV vaccination and 57.3% mentioned good personal hygiene especially of the genital area as ways of prevention. The remaining indicators received low frequencies as respondents did not know about them to be preventive measures. This has been graphically presented in Figure 2 [7].
Discussion
The World Health Organization (WHO) predicts that by the year 2025, 5,000 new cases of cervical cancer and 3,361 cervical cancer deaths will occur annually in Ghana, those who participated in the study were aged 15-38 years. This compares with a study among college students about cervical cancer screening. However, in a Nigerian study, majority were aged 26 years. The deviation in age category may be because this study sampled tertiary female students. The greater proportion of the females were single. This is because in Ghana, most females in their reproductive age complete tertiary education before they marry [8].
The study reports uneven knowledge of cervical cancer among the tertiary female students. That is, while more than half of the respondents in the study were aware and had good causal knowledge about cervical cancer, more than half also had poor knowledge on the risk and preventive methods to cervical cancer. This is consistent with similar low awareness about cervical cancer found in another study. Other studies in Ghana also reported that majority of the participants indicated that they had never heard of cervical cancer. Also in a related study that examined the knowledge and beliefs on cervical cancer and practices on cervical cancer screening among women aged 20 to 50 years in Ouagadougou revealed that, while 64.2% of participants have heard about cervical cancer, only 8.5% have heard about human papilloma virus and this confirms the uneven and inadequate information women have about cervical cancer. It was encouraging to learn that a greater proportion (41.4%) of the respondents received cervical cancer information from health workers. This is at variance with a study that had radio has been the main source of information. In another study, it was elicited that, information from friends was the main source of awareness about cervical cancer. This respondent in our study are tertiary students and they have regular contact with health workers and this probably explains why the source of information is different [9].
Conversely, lack of recommendation by health care providers hindered women in screening for cervical cancer. In addition, preventive counselling to reduce the risk of cervical cancer is viewed as been less important by health professionals in other settings. This confirms findings that despite the high prevalence of cervical cancer in developing countries, screening programs for the disease is very low.
Some respondents attributed cervical cancer to poor hygiene. This is not surprising since in a study on risk, it was reported that respondents disagree that heredity is a risk factor. This shows that there is a knowledge gap in terms of the causal factors of cervical cancer among the female students which needs public health attention targeted at increasing their knowledge on the causes of cervical cancer. Additionally, it was found from the study that, the respondents’ knowledge on the diagnosis of cervical cancer was relatively good. This is generally not a good sign as the age range of the respondents is within the recommended age for cervical cancer screening and must therefore be more aware of the preventive measures. Furthermore, about 16.6% did not know that one still needs to go for pap smear after taking the HPV vaccine which is due the fact that the vaccine does not kill 100% of all the viruses and therefore a repeated dose is imperative for good immunity. This trend is consistent with the study on assessing the knowledge and attitude towards cervical cancer screening among female students and staff in a tertiary institution in the Niger Delta. It was obvious among those unwilling to seek screening for cervical cancer that, the dominant reason was fear of the outcome and cost. This finding was also reported by Arulogun and Alubunmi, that fear of the results was among the reasons cited by the study participants who had never gone for the screening [10].
It was interesting to note the poor knowledge of the respondents on the risks associated with cervical cancer with about 64% and 78% not knowing that, the continual use of oral contraceptive and smoking of cigarette are risks of cervical cancer. In a study about the awareness of cervical cancer among female students of premier colleges in Kolkata, India reported similar outcome where out of all the student respondents, only 13%, 15%, 29% respectively could identify early onset of sexual intercourse, parity and cigarette smoking as risk factors of cervical cancer. It was also observed that, most of the respondents thought having multiple sexual partners could put an individual at risk of developing cervical cancer. The respondents also thought that having unprotected sex and early sex could predispose women to developing cervical cancer. These results were similar to studies which revealed that although lower number of the respondents recognized risk factors of cervical cancer and risk perception was low, the most commonly identified risk factors were having sex at an early age, many different sexual partners and sexually transmitted disease. The results suggest that the respondents in our study were aware of some risk factors but also misidentified some factors as risk factors which require serious targeted health education. The danger of not knowing the risk factors is that chances of prevention in terms of behavioural risk factors are almost non-existent. This then results in a higher number of women being at risk of cervical cancer [11].
The same premise may apply about ignorance on whether cervical cancer can be prevented or not. This study also showed that even though 92.4% of the respondents know that cervical cancer is preventable, they lack knowledge on cervical cancer prevention methods. This is consistent with previous studies in Ghana. There was better awareness of sexual experience and cervical cancer, including the influence of the number of previous partners similar to findings in the study by Abotchie and Shokar. This is evident in the lower percentages of the perceived preventive methods such as the use of condoms, HPV vaccine, not smoking, regular exercise and delay in age of first sexual contact among the respondents [12].
Conclusion
The study shows uneven display of knowledge of cervical cancer among the female students. While the respondents were aware of the cervical cancer and its causes, they had low knowledge of the risk factors associated with cervical cancer as well as the preventive methods to protect themselves. Therefore, there is urgent need for tertiary institutions to incorporate cancer-based education into their curriculum and into the existing medical services to boost uptake of screening programmes offered to increase the impact in reduction of cervical cancer incidence. The government should develop and incorporate into the national health insurance scheme, a policy on free screening for cervical cancer since willingness to screen was found to be high among study participants. This will enable young female adults to go to screen for the disease without being deterred by the cost of screening. Healthcare facilities should undertake regular outreach programs within the surrounding communities to create awareness about the disease and educate them on the need for regular screening.
Ethical Consideration
Ethical clearance and permission to carry the research was sought from both institutions. An introductory letter was obtained from the college of health Yamfo, Ghana and was sent to the institutions. Also, an informed consent was sought from the respondents. Factors such as social, religious, cultural and emotional values were highly respected. Respondents were assured of confidentiality as names and other personal information were not included in the study. There were no risks to the study. Participants were also told about their rights to withdraw from the study at any stage as participation in the study was voluntary.
Conflict of Interest
The authors have no competing interests.
Acknowledgement
The authors wish to express their sincere gratitude to the authorities of college of health Yamfo, Ghana for their support and all the students who took part in this exercise during the data gathering process.
References
- Lewis MJ. A situational analysis of cervical cancer in Latin America and the Caribbean. Pan Am Health Org. 2004.
- Gebreegziabher M, Asefa NG, Berhe S. Factors affecting the practices of cervical cancer screening among female nurses at public health institutions in Mekelle town, Northern Ethiopia, 2014: A cross-sectional study. J Cancer Res. 2016;2016:1-7.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68(6):394-24.
[Crossref] [Google Scholar] [PubMed]
- Yarney J, Donkor A, Opoku SY, et al. Characteristics of users and implications for the use of complementary and alternative medicine in Ghanaian cancer patients undergoing radiotherapy and chemotherapy: A cross-sectional study. BMC Complement Altern Med. 2013;13(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Lingwood RJ, Boyle P, Milburn A, et al. The challenge of cancer control in Africa. Nat Rev Cancer. 2008;8(5):398-403.
[Crossref] [Google Scholar] [PubMed]
- William M, Kuffour G, Ekuadzi E, et al. Assessment of psychological barriers to cervical cancer screening among women in Kumasi, Ghana using a mixed methods approach. Afr Health Sci. 2013;13(4):1054-61.
[Crossref] [Google Scholar] [PubMed]
- Abotchie PN, Shokar NK. Cervical cancer screening among college students in Ghana: Knowledge and health beliefs. Int J Gynecol Cancer. 2009;19(3):412-6.
[Crossref] [Google Scholar] [PubMed]
- Makwe CC, Anorlu RI, Odeyemi KA. Human Papillomavirus (HPV) infection and vaccines: Knowledge, attitude and perception among female students at the university of Lagos, Lagos, Nigeria. J Epidemiol Glob Health. 2012;2(4):199-06.
[Crossref] [Google Scholar] [PubMed]
- Abudukadeer A, Azam S, Mutailipu AZ, et al. Knowledge and attitude of Uyghur women in Xinjiang province of China related to the prevention and early detection of cervical cancer. World J Surg Oncol. 2015;13(1):1-7.
[Crossref] [Google Scholar] [PubMed]
- Williams MS, Amoateng P. Knowledge and beliefs about cervical cancer screening among men in Kumasi, Ghana. Ghana Med J. 2012;46(3):147.
[Google Scholar] [PubMed]
- Opoku CA, Browne EN, Spangenberg K, et al. Perception and risk factors for cervical cancer among women in northern Ghana. Ghana Med J. 2016;50(2):84-9.
[Crossref] [Google Scholar] [PubMed]
- Sawadogo B, Gitta SN, Rutebemberwa E, et al. Knowledge and beliefs on cervical cancer and practices on cervical cancer screening among women aged 20 to 50 years in Ouagadougou, Burkina Faso, 2012: A cross-sectional study. Pan Afr Med J. 2014;18:175.
[Crossref] [Google Scholar] [PubMed]