Research Article - Current Pediatric Research (2022) Volume 26, Issue 8
Junk food as cause of non-infectious sore throat in children.
Zafarullah Beigh1*, Faheem Khalid1, Suhail Ahmad Choh2
1Department of Otorhinolaryngology, Government Medical College Baramulla, Jammu and Kashmir India
2Department of Pediatrics, Government Medical College Baramulla, Jammu and Kashmir, India
- Corresponding Author:
- Zafarullah Beigh
Department of Otorhinolaryngology
Government Medical College Baramulla
Jammu and Kashmir
India
E-mail: Zafarullah@gmail.com
Received: 04 August, 2022, Manuscript No. AAJCP-22-69327; Editor assigned: 05 August, 2022, PreQC No. AAJCP-22-69327 (PQ); Reviewed: 08 August, 2022, QC No. AAJCP-22-69327; Revised: 15 August, 2022, Manuscript No. AAJCP-22-69327(R); Published: 22 August, 2022, DOI:10.35841/0971-9032.26.8.1555-1558.
Abstract
Introduction: Sore throat is one of the common reasons for outpatient and emergency visits among children. Sore throat is a symptom in which there is painful burning or scratching sensation in the back of throat. Various causative agents for sore throat are mentioned in literature. This study is about non-infectious sore throat in children due to commonly consumed spicy food “junk foods”. Material and Method: This study includes one hundred and seventy six Sore throat patients below 16 years of age, who gave history of eating junk food. Examination of all patients was done and advised to stop eating junk foods. Patient’s symptoms and signs were recorded and follow up was done after 2 days, 4 days and after 7 days. Results: We found that painful burning or scratching sensation in the back of the throat was relieved in 156 out of 176 patients after 2 days and pain on swallowing was relieved in 166 patients out of 176 patients after 2 days. This figure goes up 4 days after stopping eating junk food to 166 out of 176 and 170 out of176 respectively. Similarly, on examination of oropharynx we found that congestion on oropharyngeal structures was absent in 152 out of 176 patients after 2 days and figure goes up to 165 out of 176 patients after 4 days.
Keywords
Sore throat, Junk food, Laryngopharyngeal reflux.
Introduction
Sore throat is primary symptom of pharyngitis. The terms “sore throat” and “pharyngitis or pharyngotonsillitis” are often used interchangeably. Pharyngitis refers to objective evidence of inflammation of the pharynx, such as exudates, ulceration, or definite erythema.Sore throat is a symptom often caused by an inflammatory process in the oropharynx or nasopharynx. Most of these cases are of viral origin and occur as a part of the common cold. In addition to viral pathogens, bacterial pathogens may also cause pharyngeal infections.
Fear of complications, or a wish to relieve pain or to satisfy patients often lead physicians to use antibiotic treatment for sore throat.Sore throat is itself a symptom, and pain or discomfort in the pharynx is not always caused by an infectious agent. Conversely, infectious agents are often found in the pharyngeal area in asymptomatic patients. There is an apparent lack of studies on non-infective causes of sore throat like that caused by irritant foods.This study is about the role of commonly consumed junk food (uncle chips, lays, pringles, tedhemedhe, yummy toes, tangles, kurkure etc.) on sore throat.
Material and Method
This study was conducted in department of otorhinolaryngology and head neck surgery and department of pediatrics government medical college Baramulla from March 2020 to February 2021. One hundred and seventy sixsore throat patients under 16 years of age group, who gave history themselves or by their parents of eating junkfood before starting of sore throat were included in this study and proper written informed consent was taken from all patients and/or their parents. Routine physical examination and detailed ear, nose and throat examination of all patients was done. All patients were advised to stop eating junk foodparents of these patients were instructed to ensure the same.
All patients were put on placebo medication (multivitamin tablets/syrup) for 4 days and encouraged to take lot of plain water. Patient’s symptoms and signs were recorded and follow up was done after 2 days, 4 days and after 7 days.Placebo treatment was continued for 7 days in those patients whose signs and symptoms were found improved after 4 days, whereas systemic antibiotics, antihistaminic, proton pump inhibitors and analgesic either alone or in combination were started on those patients whose signs and symptoms persisted or aggravate after 4 days on placebo treatment.
Results
| Age in years | Number of patients n=176 | Percentage |
|---|---|---|
| <5 | 52 | 29.54 |
| 06-10 | 73 | 41.47 |
| 11-16 | 51 | 28.97 |
| Mean ± SD | 9 + 3.3 | |
Table 1. Age wise distribution of patients.
| Sex | Number of patients | Percentage |
|---|---|---|
| Male | 109 | 61.9 |
| Female | 67 | 38.09 |
| Total | 176 | 100 |
Table 2. Sex wise distribution of patients.
| Symptoms | Number of patients at presentation (%) | Number of patients after 2 days (%) | Number of patients after 4 days (%) | Number of patients after 7 days (%) |
|---|---|---|---|---|
| Painful burning or scratching sensation in the back of the throat | 176 (100%) | 20 (11.36) | 10 (5.68) | 02 (1.13) |
| Pain when swallowing | 76 (100%) | 10(5.68) | 6 (3.40) | 02 (1.13) |
| Dry cough | 42 (23.86%) | 22 (12.5) | 13 (7.38) | 0 (0) |
| Foreign body sensation throat | 29 (16.47) | 17 (9.65) | 9 (5.11) | 2 (1.13) |
Table 3. Symptoms of patients at presentations and on follow up.
| Symptoms | Number of patients At presentation (%) | Number of patients after 2 days (%) | Number of patients after 4 days (%) | Number of patients after 7 days (%) |
|---|---|---|---|---|
| Painful burning or scratching sensation in the back of the throat | 176 (100%) | 20 (11.36) | 10 (5.68) | 02 (1.13) |
| Pain when swallowing | 76 (100%) | 10(5.68) | 6 (3.40) | 02 (1.13) |
| Dry cough | 42 (23.86%) | 22 (12.5) | 13 (7.38) | 0 (0) |
| Foreign body sensation throat | 29 (16.47) | 17 (9.65) | 9 (5.11) | 2 (1.13) |
Table 4. Signs of patients at presentation and on follow up.
| Signs | At Presentation (%) |
After 2 days (%) | After 4 days (%) | After 7 days (%) |
|---|---|---|---|---|
| Congestion on tonsilar pillars and soft palate | 148 (84.09) | 72 (40.90) | 13 (7.38) | 0 (0) |
| Congestion on tonsilar pillars, soft palate and posterior pharyngeal wall | 117 (66.47) | 69 (39.20) | 23 (13.06) | 02 (1.13) |
| Congestion on tonsilar pillars, soft palate and tonsils | 109 (61.93%) | 77 (43.75) | 25 (14.20) | 04 (2.27) |
| Congestion on tonsilar pillars and soft palate with Features of laryngopharyngeal reflux ( inter arytenoid congestion) | 79 ( 44.88) | 49 (27.84) | 33 (18.75) | 11 (6.25) |
Table 5. Signs of patients at presentation and on follow up.
Discussion
Soreness is generally described by the patient as pain in the throat without the effort of swallowing and also a painful swallow[1]. Sorethroat usually includes a painful burning or scratching sensation in the back of the throat, pain when swallowing, and sometimes tenderness in the neck. Other symptoms that may accompany a sore throat include coughing, sneezing, hoarseness or laryngitis, runny nose mild fever, general fatigue, swollen lymph nodes (glands) in the neck, bad breath (halitosis),and ear pain. A sore throat, depending on the cause, should last for no longer 5 to 7 days.
Treatment for a sore throat depends on the cause. Because viral illnesses are the most common cause of a sore throat, it is important not to use antibiotics to treat them. Antibiotics do not alter the course of viral infections. Unnecessary use of an antibiotic exposes patient to the risks of an allergic reaction and antibiotic side effects, such as nausea, vomiting, diarrhea, rashes, and yeast infections. Antibiotics also may kill beneficial bacteria and encourage the development of dangerous antibiotic-resistant bacteria.
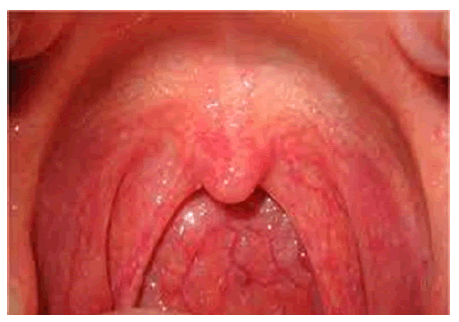
In our study we enrolled those patients of sore throat who gave history junk food intake, majority of patients were males (61.90%) in age group of 6-10 years (41.47 %). We found that painful burning or scratching sensation in the back of the throat and pain during swallowing was presenting complaint in all hundred and seventy six patients. On examination congestion of tonsillar pillars and soft palate was seen in almost all patients, whereas 109 patients out of 176 patients had inflamed tonsils as shown in Figure 1 ( most of these already diagnosed as chronic tonsillitis and dated for tonsillectomy), congested posterior pharyngeal wall and some patients had features of laryngopharyngeal reflux. None of these patients had cervical lymphadenopathy.
For sore throats caused by streptococcus, treatment with antibiotics may be needed. According to Tanzet al. [2], over 20% of asymptomatic school children may be carriers of group A streptococcal infection during the winter and spring. Complications of group A b-hemolytic streptococcal pharyngitis are generally rare in both children and adults [3–10]. In our study as all patients gave history of junk food intakeand also gave positive past history of similar illness as and when they eat junk food. Patients and their parents were counseled about such food being possible causative agent for sore throat and advised not to eat them further.
The trials on the effectiveness of zinc gluconate on sore throat provided conflicting results [11,12]. It is difficult to make firm recommendations about the dose, formulation and duration that should be used [13]. Further there are no reliable data on the efficacy of alternative Treatment (herbal treatment and acupuncture) on sore throat [14-20]. Based on these observations we prescribed only placebo medication (multivitamins) to sore throat patients.
A systematic review [21] found that non-steroidal anti-inflammatory drugs and paracetamol are more effective than placebo for reducing acute sore throat symptoms in adults. But in our patients pain was bearable and after proper assurance and explanations, all patients and their parents agreed for avoiding analgesics for minimum 4 days.
We found that painful burning or scratching sensation in the back of the throat was relieved in 156 out of 176 patients after 2 days and pain on swallowing was relieved in 66 patients out of 76 patients after 2 days. This figure goes up4 days after stopping eating junk foodto 166 out of 176 and 70 out of 76 respectively. Similarly, on examination of oropharynx we found that congestion on orpharyngeal structures was absent in 104 out of 176 patients after 2 days and figure goes up to 163 out of 176 patients after 4 days.
Those small percentage of patients whose symptoms and signs persist or aggravate after 4 days of stopping junk food were put on either alone or combination of proton pump inhibitors, oral antibiotics, antihistamines and/or analgesics. Persistence of symptoms in some patients can be due to Secondary infection oreating junk food against medical advice.
Conclusion
Sore throat is one of the common ailments in adolescentage group. Junk food is very much favorite to children. It is consumed in large amount in this part of world and children eat this food very often. Large randomized controlled trails are required to evaluate role of junk foods on sore throat but this study shows that junk foods are definite causative factor for sore throat and people especially children should not eat such foods in future.
References
- Linder JA, Bates DW, Lee GM, et al.Antibiotic treatment of children with sore throat. JAMA 2005; 294: 2315-22.
- Tanz RR, Shulman ST. Chronic pharyngeal carriage of group A streptococci.Pediatr Infect Dis J2007; 26: 175–176.
- Gerber MA, Baltimore RS, Eaton CB, et al.Prevention of rheumatic fever and diagnosis and treatment of acute streptococcal pharyngi-tis: A scientific statement from the American Heart Association rheumatic fever, endocarditis, and Kawasaki disease Committee of the Council on cardiovascular disease in the young, the Interdisci-plinary Council on functional genomics and translational biology,and the Interdisciplinary Council on quality of care and outcomesresearch: Endorsed by the American academy of pediatrics. Circulation 2009; 119: 1541–1551.
- Talmon Y, Gilbey P, Fridman N, et al. Acutemyopericarditis complicating acute tonsillitis: Beware the young male patient with tonsillitis complaining of chest pain. Ann Otol Rhinol Laryngol 2008; 117: 295–297.
- https://www.aafp.org/pubs/afp/issues/2008/0115/p199.html
- Abdel-Haq NM, Harahsheh A, Asmar BL. Retropharyngeal abscess in children: The emerging role of group A bhemolytic streptococcus. South Med J2006; 99: 927–931.
- Martin JM, Green M. Group A streptococcus. Semin Pediatr Infect Dis2006; 17: 140–148.
- Almroth G, Lindell A, Aselius H, et al. Acute glomerulonephritis associated with Streptococcus pyogenes with concomitant spread of Streptococcus constellatusin four rural families. Ups J Med Sci 2005; 110: 217–231.
- Gerber MA. Diagnosis and treatment of pharyngitis in children. Pediatr Clin North Am2005; 52: 729–747.
- Hanna BC, McMullan R, Gallagher G, et al. The epidemiology of peritonsillar abscess disease in Northern Ireland. J Infect2006; 52: 247–253.
- Mossad SB, Macknin ML, Medendorp SV, et al. Zinc gluconate lozenges for treating the common cold. A randomized, double-blind, placebo-controlled study. Ann Intern Med 1996; 125: 81–88.
- Macknin ML, Piedmonte M, Calendine C, et al. Zinc gluconate lozenges for treating the common cold in children: A ran-domized controlled trial. JAMA 1998; 279: 1962–1967.
- Singh M, Das RR. Zinc for the common cold. Cochrane Database Syst Rev 2011; (2): CD001364.
- Timmer A, Gunther J, Rucker G, et al.Pelargonium sidoides extract for acute respiratory tract infections. Cochrane Database Syst Rev2008; (3): CD006323.
- Shi Y, Gu R, Liu C, et al. Chinese medicinal herbs for sore throat. Cochrane Database Syst Rev2007; (3): CD004877.
- Brinckmann J, Sigwart H, van Houten TL. Safety and efficacy of a traditional herbal medicine (throat coat) in symptomatic temporary relief of pain in patients with acute pharyngitis: A multicenter, prospective, randomized, double-blinded, placebo-controlled study. J Altern Complement Med 2003; 9: 285–298.
- Gunsberger M. Acupuncture in the treatment of sore throat symp-tomatology. Am J Chin Med (GardCity NY)1973; 1: 337–340.
- https://daignet.de/site-content/die-daig/fachorgan/archiv/2006/ejomr-2006_1-pdfs/Hubbert%20Kopie.pdf
- Rau E. Treatment of acute tonsillitis with a fixed-combination herbal preparation. Adv Ther 2000; 17: 197–203.
- https://europepmc.org/article/med/10351119
- https://www.researchgate.net/publication/12202076_How_effective_are_treatments_other_than_antibiotics_for_acute_sore_throat