Research Article - Current Pediatric Research (2021) Volume 25, Issue 9
Initial steps of delivery room resuscitation in depressed neonates-suctioning first or drying first!
Vijayakumar Biradar, Siddu Charki*, MM Patil, P Siri Chandna, P Mounica, SS Kalyanshettar, SV Patil
Department of Pediatrics, BLDE (DU) Shri BM Patil Medical College Hospital and Research Centre, Vijayapur, India
- Siddu Charki
Department of Pediatrics
BLDE (DU) Shri BM Patil Medical College Hospital and Research Centre
Vijayapur
India
E-mail: sidducharki@bldedu.ac.in/drsidducharki@gmail.com
Corresponding Author:
Accepted date: 25th September, 2021
Abstract
Background: Establishing adequate respiration at birth is necessary to start and maintain in extra uterine life; a phenomenon that proceeds smoothly in 90% of neonates but 10% of newborns fail to initiate effectual breathing. Most of these neonates start breathing after initial stimulation, about 3%-5% need basic resuscitation, but <1% requires advanced resuscitation. Objectives: To compare the effect of suctioning first or drying first on bradycardia outcomes during resuscitation and the need and duration of positive pressure ventilation, hypothermia at NICU admission or onset of respiratory distress at 6 hours of age, duration of NICU stay, and death. Methods: This study was conducted in the MCH unit of Shri BM Patil medical college hospital and research centre, Vijayapura. Design: Open-label, parallel grouped, randomized controlled trial. 200 depressed newborns requiring initial resuscitation steps at delivery were enrolled to receive either suctioning first or drying first during delivery room resuscitation. Results: Bradycardia during resuscitation and the need and duration of positive pressure ventilation was high in the suction first group (P-value=0.046). Incidence of hypothermia at NICU admission, onset of respiratory distress at 6 hours of age was also high in the suction first group. Duration of NICU stay was high in the suction first group (<0.001). Conclusion: At birth, in depressed newborns, the sequence of advocating initial resuscitation steps, drying first had a favorable effect compared to suctioning first on bradycardia outcomes during resuscitation and the need and duration of positive pressure ventilation and NICU stay.
Keywords
Suctioning, Drying, Initial steps, Bradycardia, Positive pressure ventilation.
Introduction
At birth, approximately 10% of newborns require assistance to initiate and sustain adequate respiration and perinatal asphyxia accounts for 23% of 40 lakhs of neonatal deaths each year globally. Timely and skillful delivery room resuscitation can prevent many of these neonatal morbidities and mortality [1,2]. All depressed newborns at birth requiring delivery room resuscitation should receive 'initial steps' of resuscitation before initiating positive pressure ventilation.
These essentially constitute temperature maintenance, positioning, suctioning, drying, and tactile stimulation. During the initial steps of resuscitation, suctioning is done to clear the airway, and drying is done to prevent heat loss. The sequence of suctioning first followed by drying has been approved as part of the initial steps in the Neonatal Resuscitation Program (NRP) of the American Academy of Pediatrics (AAP) based on expert opinion rather than evidence [3]. It is not established whether the same sequence of initial steps should be practiced in resource-limited settings, where the danger of hypothermia constitutes a more significant threat to neonates [4-6]. The first edition of Indian NRP recommended for drying sequence followed by suctioning as initial resuscitation steps [7].
In contrast, the neonatal resuscitation module of Facility-based newborn care has advocated the sequence of suctioning first, followed by drying. Varied recommendations have led to uncertainty among health professionals doing delivery room resuscitation. The present study's objective was to compare suctioning first versus drying first as a first initial step during delivery room resuscitation on bradycardia outcomes during resuscitation and the need and duration of positive pressure ventilation, hypothermia at NICU admission, or onset of respiratory distress at 6 hours of life [8].
Methods
This randomized controlled trial was conducted in the maternal and child health unit of Shri BM Patil medical college hospital and research centre, Vijayapura from January 2020 to December 2020. Written informed consent was collected. The institutional ethics committee approved the study protocol.
Inclusion criteria
Inborn neonates who were depressed at birth requiring initial resuscitation steps were included in the study. Depression at birth was defined as the presence of apnea or gasping and limp or lack of muscle tone.
Exclusion criteria
Neonates with significant congenital anomalies and history of meconium-stained liquor were excluded. Maternal characteristics, including age, antenatal care visits, gravida, parity, h/o per vaginal leak, maternal fever, PIH, eclampsia, antepartum hemmoraghe, evidence of fetal distress, and mode of delivery were documented. Enrolled newborns were randomized into either suctioning first or drying first groups using random permuted blocks of 5 by an independent person. Serially numbered, opaque, and sealed envelopes were used to allocate newborns to the suctioning and drying groups. All deliveries were attended by pediatric resident who was trained in neonatal resuscitation program as per NRP guidelines.
If a newborn was born apneic or limp at birth, the umbilical cord was clamped immediately and the newborn was placed under a radiant warmer with the neck slightly extended. At this point in time, staff nurse opened the serially numbered sealed envelope, and the sequence of initial resuscitation steps was performed as per randomization. During resuscitation process, pulse oxymeter was connected to right hand and oxygen saturation and heart rate of newborn were recorded. Suctioning was done through wall-mounted suction apparatus with a pressure of 80-100 mm of Hg, and it was limited to 3 to 5 seconds, thereby avoiding deep suctioning. Drying was done using two pre-warmed linens to prevent further heat loss. Positive pressure ventilation was initiated if the baby had persistent apnea or bradycardia (heart rate<100/minute) even after initial resuscitation steps. Apgar score at 1 and 5 min in both groups was noted.
All depressed neonates were monitored and managed as per unit protocol based on Apgar score at 1 min and 5 min. Newborns were placed in thermo neutral environment under radiant warmer with a set temperature of 36.5°C. A predesigned structured proforma was used to document newborn characteristics, including heart rate, oxygen saturation at 1 min, 2 min, 5 min, and 10 min, the axillary temperature at admission, and signs of respiratory distress (hurried breathing, chest wall retractions, grunting, and bilateral air entry). Investigations included rapid sepsis screening tests including complete blood count, absolute neutrophil count, C-reactive protein and blood culture, arterial blood gas analysis, chest X-ray, echocardiography, and cranial ultrasonography if required. In newborns admitted in NICU, respiratory support was initiated via non-invasive ventilation like oxygen hood, humidified High Flow Nasal Cannula (HFNC), nasal Continuous Positive Airway Pressure (CPAP), or conventional ventilation as per the Silverman Anderson scoring system. Intravenous fluids and inotropes were started as per unit protocol.
Primary outcomes were bradycardia during resuscitation and the need and duration of positive pressure ventilation, chest compressions, and use of adrenaline during delivery room resuscitation. Secondary outcomes included oxygen saturation during the first 10 minutes of life, hypothermia at NICU admission or onset of respiratory distress at 6 hours of age, NICU stay duration, and death. Hypothermia was defined as axillary temperature < 36.50°C. Respiratory distress was defined as the presence of at least one of the following: hurried breathing with respiratory rate >60/minute, chest wall retractions, and grunting.
Sample size
Sample size of 178 was calculated using an expected incidence of 10% of the need for delivery room resuscitation, a precision (d) of 0.05 and level of confidence of 95%. Taking into consideration the 10% rate of attrition, the total sample size was 200 newborns, 100 in each group of drying first and suctioning first [3].
Statistical analyses
The statistical program SPSS version 23.0 was used for analysis. Independent samples t-test/Mann Whitney U-test and fisher exact test were used to compare non-parametric and parametric variables. Risk Ratios (RR) with 95% CI were calculated for outcome variables. A P value of <0.05 was considered statistically significant.
Results
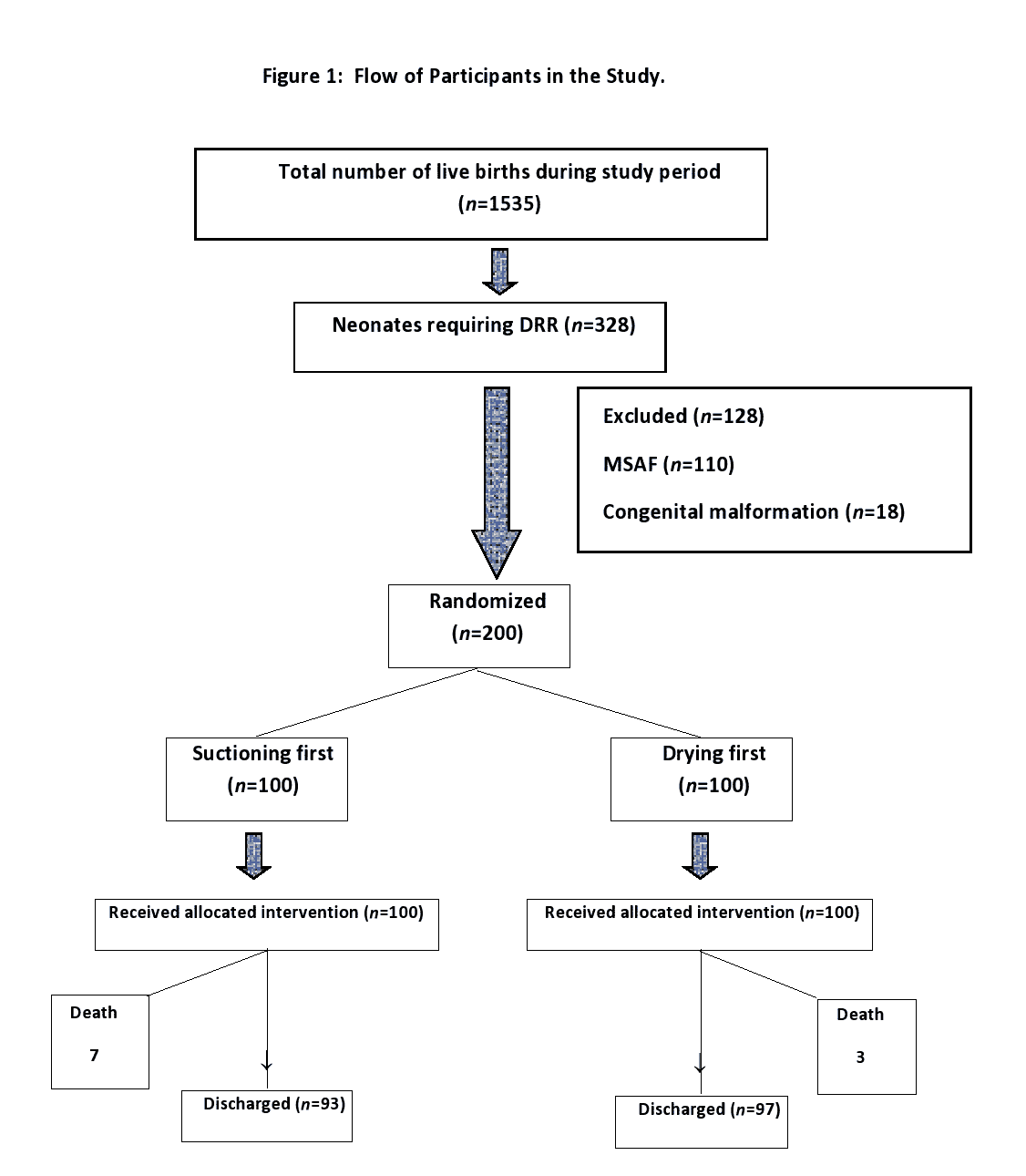
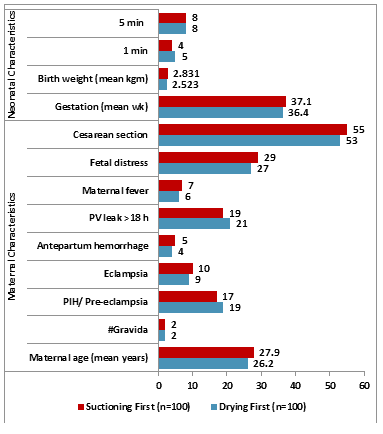
100 neonates were enrolled in both groups as per each allocated intervention (Figure 1). Maternal and neonatal baseline characteristics were comparable in both study groups (Figure 2 and Table I). Bradycardia during resuscitation and the need and duration of positive pressure ventilation was high in the suction first group in comparison to drying first group (46 (46%) vs. 32 (32%) (P-value=0.046)).
| Characteristics | Drying first | Suctioning first | P value |
|---|---|---|---|
| (n=100) | (n =100) | ||
| Maternal characteristics | |||
| Maternal age, (years) | 26.2 ± 6.6 | 27.9 ± 5.6 | 0.051 |
| #Gravida | 2 (1-3) | 2 (1-3) | - |
| PIH/ Pre-eclampsia | 19 (19%) | 17 (17%) | 0.713 |
| Eclampsia | 09 (9%) | 10 (10%) | 0.809 |
| Antepartum hemorrhage | 4 (4%) | 5 (5%) | 0.733 |
| PV leak >18 hrs | 21 (21%) | 19 (19%) | 0.723 |
| Maternal fever | 6 (6%) | 7 (7%) | 0.774 |
| Fetal distress | 27 (27%) | 29 (29%) | 0.752 |
| Cesarean section | 53 (53%) | 55 (55%) | 0.776 |
| Neonatal characteristics | |||
| Gestation, wk | 36.4 ± 2.3 | 37.1 ± 2.8 | 0.054 |
| Birth weight, g | 2523 ± 1260.1 | 2831 ± 950.6 | 0.052 |
| 1 min | 5 (3-7) | 4 (3-6) | 0.733 |
| 5 min | 8 (6-9) | 8 (6-9) | - |
Table 1. Maternal and neonatal characteristics of study groups. Values in number (%) except; *: Mean (SD) or #: Median (IQR). *: Significant at 5% level of significance.
Bag and tube ventilation, Chest compressions, and Adrenaline usage were high in the suction first group compared to the drying first group, which was not statistically significant (P value>0.05). Oxygen saturation at 1 min, 2 min, 5 min, and 10 min was almost similar in both groups with a non-significant P-value. (>0.05) Incidence of hypothermia at NICU admission, onset of respiratory distress at 6 hours of age was also high in the suction first group with a non-significant P value (>0.05). Duration of NICU stay was high in the suction first group compared to drying first group with a significant P value <0.001. Death was observed in 3% neonates in the drying first group and 7% neonates in the suction first group, which was not statistically significant (P-value=0.097) (Table 2).
| Variable | Drying first (n=100) | Suctioning first (n=100) | Relative risk (95% CI) | P value |
| Bradycardia during resuscitation (HR<100) | 32 (32%) | 46 (46%) | 0.90 (0.81-1.14) | 0.046* |
| Bag and mask ventilation | 32 (32%) | 46 (46%) | 0.90 (0.81-1.14) | 0.046* |
| Duration, sa | 30 | 60 | <0.001* | |
| Bag and tube ventilation | 10 (10%) | 19 (19%) | 1.06 (0.79-1.35) | 0.071 |
| Duration, mina | 05-Aug | 06-Dec | - | |
| Chest compressions | 6 (6%) | 14 (14%) | 0.71 (0.51-1.23) | 0.059 |
| Adrenaline usage | 4 (4%) | 10 (11%) | 0.65 (0.35-2.15) | 0.096 |
| Oxygen saturation (%)a | ||||
| At 1 min | 60 (56-63) | 56 (54-63) | 0.566 | |
| At 2 min | 70 (66-72) | 66 (62-70) | 0.544 | |
| At 5 min | 86 (83-88) | 84 (80-88) | 0.692 | |
| At 10 min | 96 (92-98) | 95 (90-98) | 0.633 | |
| Hypothermia at admission | 38 (38%) | 45 (45%) | 0.81 (0.59-1.08) | 0.315 |
| Respiratory distress at 6 h | 27 (27%) | 33 (33%) | 0.84 (0.74-1.15) | 0.177 |
| Duration at NICU stay | 4 ± 2.75 | 6 ± 1.45 | <0.001* | |
| Death | 3 (3%) | 7 (7%) | 0.34 (0.18-1.31) | 0.097 |
Table 2. Outcome variables in depressed neonates in the study groups.All values in no (%) except , a: Median (IQR); RR: Relative Risk; *: Significant at 5% level of significance.
Discussion
The literature review showed limited evidence on studies investigating the comparative efficacy of drying versus suctioning first in depressed neonates as initial steps during delivery room resuscitation. The present study showed that sequence of drying first or the suctioning first during initial resuscitation steps of delivery room in depressed neonates had significant outcomes, including increased bradycardia incidence during resuscitation and the need and duration of positive pressure ventilation were high in suctioning the first group with significant P-value, which could be attributed to apnea due to vagal stimulation in suctioning first group resulting in bradycardia and increased need of positive pressure ventilation. Hypothermia outcomes at NICU admission or onset of respiratory distress at 6 hours of age were comparable in depressed newborns in both groups with no statistical significance.
The incidence of hypothermia was relatively high in both groups of neonates. Neonates developing hypothermia during the process of resuscitation could be a possibility. It is well established that hypothermia at admission in neonates is associated with adverse outcomes [4-6]. Level and duration of resuscitative interventions such as bag and tube ventilation, chest compressions, medications like adrenaline usage between the two groups showed no difference. Oxygen saturation at 1 min, 2 min, 5 min, and 10 min was comparable between the two groups. Duration of NICU stay was high in suctioning the first group than drying the first group, which could be due to delayed perinatal adaptation at birth. The mortality rates were also similar in the two groups. [9-11].
Conclusion
During delivery room resuscitation in depressed neonates, initial resuscitation steps such as suctioning first or drying first had significant differences in outcomes in terms of incidence of bradycardia, need and duration of positive pressure ventilation and NICU stay duration. The sequence of advocating initial resuscitation steps, drying first had a favorable effect compared to suctioning first on outcomes of bradycardia during resuscitation and the need and duration of positive pressure ventilation and NICU stay. Hence it would be better to adopt drying first during resuscitation as advocated by the Indian NRP (first edition) in the Indian scenario. We should follow a standardized approach in implementing NRP guidelines to bring uniformity and consistency among health care professionals.
References
- Barber CA, Wyckoff MH. Use and efficacy of endotracheal versus intravenous epinephrine during neonatal cardio-pulmonary resuscitation in the delivery room. Pediatrics 2006; 118: 1028-34.
- Black RE, Cousens S, Johnson HL, et al. Child health epidemiology reference group of WHO and UNICEF. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet 2010; 375: 1969-87.
- Wyckoff MH, Aziz K, Escobedo MB, et al. Part 13: Neonatal resuscitation: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132: S543-60.
- Sodemann M, Nielsen J, Veirum J, et al. Hypothermia of newborns is associated with excess mortality in the first 2 months of life in Guinea-Bissau, West Africa. Trop Med Int Health 2008; 13: 980-6.
- Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: Distribution, risk factors and outcomes. J Perinatol 2011; 31: S49-56.
- Mullany LC, Katz J, Khatry SK, et al. Risk of mortality associated with neonatal hypothermia in southern Nepal. Arch Pediatr Adolesc Med 2010; 164: 650-6.
- http://www.nnfi.org/assests/pdf/nnf-mf.pdf
- Neonatal Resuscitation Module. Facility based newborn care: Ministry of health and family welfare, government of India, New Delhi. 2014; pp: 9-16.
- Kumar R, Aggarwal AK. Body temperatures of home delivered newborns in north India. Trop Doct 1998; 28: 134-6
- Kaushik SL, Grover N, Parmar VR, et al. Hypothermia in newborns at Shimla. Indian Pediatr 1998; 35: 652-6.
- Bang AT, Reddy HM, Deshmukh MD, et al. Neonatal and infant mortality in the ten years (1993 to 2003) of the Gadchiroli field trial: Effect of home-based neonatal care. J Perinatol 2005; 25(Suppl 1): S92-107.