Case Report - Allied Journal of Clinical Pathology Research (2017) Allied Journal of Clinical Pathology Research (Special Issue 1-2017)
Infantile malignant osteopetrosis with interesting bone marrow biopsy findings.
Kesarwani D*, Kelkar K, Manchanda R and Godbole R
Department of Pathology, KEM Hospital, Pune, India
- *Corresponding Author:
- Deepika Kesarwani
Department of Pathology
KEM Hospital, Pune, India
E-mail id: ritu.mekesarwani@gmail.com
Accepted date: August 24, 2017
Citation: Kesarwani D, Kelkar K, et al. Infantile malignant osteopetrosis with interesting bone marrow biopsy findings. Allied J Clinicl Path. 2017;1(1):16-17.
Introduction
Osteopetrosis also known as Albers-Schonberg disease or marble bone disease is a rare genetic metabolic bone disorder characterized by a marked increase in bone density caused by a defect in bone remodeling due to failure of normal osteoclast function. It is classified into three forms: Infantile malignant autosomal recessive osteopetrosis, intermediate osteopetrosis and autosomal dominant (AD) osteopetrosis. Malignant infantile osteopetrosis is a rare severe fatal disorder with an average incidence of 1:200,000-1:300,000 [1]. The diagnosis is confirmed by radiology. Bone marrow aspiration in such cases is difficult and usually leads to dry tap. Trephine biopsy is essential in these cases to obtain bone marrow picture. Here we are reporting a case of infantile malignant osteopetrosis in a 6 months old female.
Case Report
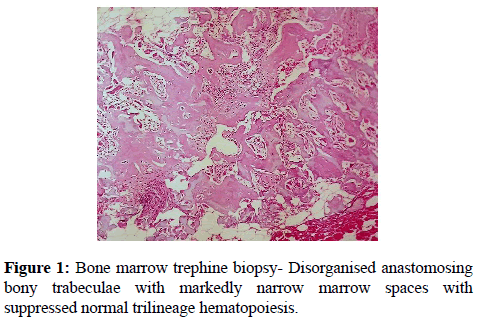
A 6 months old female infant presented to our centre with complaint of fever since 7 days. On clinical examination she was found to have pallor and hepatosplenomegaly. Her initial investigations revealed anemia (Hb-7.0 g/dl) and thrombocytopenia (Platelets: 38,000 /cumm). Peripheral smear findings revealed normocytic normochromic RBCs with anisopoikilocytosis, tear drop cells, nucleated red cells (25 nRBCs/100 WBCs) and leucoerythroblastic blood picture with peripheral smear showing shift to left upto blasts. Biochemistry workup revealed very high Lactate dehydrogenase (LDH) 2534 U/L (170-450 U/L), elevated Aspartate aminotransferase (AST) and Alanine aminotransferases (ALT) level. Based on peripheral smear finding, bone marrow aspiration and biopsy was advised and was obtained from posterior superior iliac spine. Bone marrow aspiration was dry tap. Bone marrow trephine biopsy revealed disorganized bony trabeculae, decreased bone marrow spaces with markedly suppressed trilineage hematopoiesis, focal areas of fibrosis and areas of new woven bone formation (Figure 1).
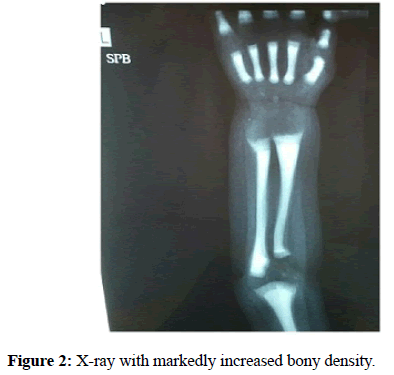
Plain radiograph of left Forearm and wrist revealed generalized increase in bone density and bone within bone appearance which is characteristic of infantile malignant osteopetrosis (Figure 2).
After the diagnosis was made, supportive treatment was given as blood transfusion for correction of anaemia, broad spectrum antibiotics to counteract infection along with calcitriol which helps to stimulate dormant osteoclast under the Paediatrics department of our center. Bone marrow transplantation was advised to the patient, but parents were non- affording. However, the condition of patient deteriorated and patient died eventually after 3 months.
Discussion
The term osteopetrosis is derived from the Greek ‘osteo’ meaning bone and ‘petros’, for stone. Osteopetrosis was first described by a German radiologist Albers-Schonberg in 1904 [2], so it is also known as Albers-Schonberg disease. Osteopetrosis is a rare genetic disorder resulting in generalized sclerosis of bones with a reduction of marrow spaces subsequent to defective osteoclast function and decreased bone turnover [3,4]. Osteopetrosis is categorized chiefly into three types: Infantile malignant autosomal recessive form, intermediate autosomal recessive form, and the benign autosomal dominant form or tarda [3-6]. The first two types are associated with a poor prognosis, have an onset at or shortly after birth and are usually fatal [3-7]. The benign autosomal dominant form manifests in later childhood and is incidentally discovered on a radiographic examination. The diagnosis of Osteopetrosis is usually made by radiological investigations. Radiographic features include increase in bone density of the entire skeleton with defective metaphyseal remodeling [3,4]. Long bones exhibit decreased marrow spaces with cortical thickening and become club-shaped [3]. A “bone within bone” or “endobone” appearance reflecting the dense shadow of the abnormal new bone within the outline of the normal bone is archetypal of osteopetrosis [3]. Bones may be uniformly sclerotic, but alternating sclerotic and lucent bands may be noted in iliac wings and near the ends of long bones (Rugger- Jersey Sign) [8]. Computerized tomography scan can be used for diagnosis and to determine the effect of the treatment. It is also used to assess auditory and optic canal which can also get affected in this disease. The abnormal bone formation and expansion interferes with medullary hematopoiesis which results in life threatening anemia, thrombocytopenia and increased susceptibility to infections which is also present in our case. This also leads to extra medullary hematopoiesis which is the reason for leucoerythroblastic blood picture and hepatosplenomegaly. Leucoerythroblastic blood picture, cytopenias and extra medullary hematopoiesis are consistently seen with these cases. So it can be a pointer towards this disease. Based on peripheral smear findings, bone marrow pathology including leukaemia, metastasis or infiltrative bone marrow disease (storage disease) were considered in differential diagnosis. Bone marrow trephine biopsy usually in such cases shows narrowing of bone marrow spaces with marked hypocellularity, markedly suppressed erythropoiesis, granulopoiesis and megakaryocytes. There is abnormal bone formation with thickened multiple disorganized bony trabeculae with areas of patchy reticulin fibrosis and several interrupted pieces of ossified cartilage. The disease has poor outcome and is fatal in most cases.
However the treatment options can be divided into medical and surgical. Medical management comprises of Calcitriol which help by stimulating dormant osteoclasts, thus stimulating bone resorption [9]. Large doses of calcitriol, along with restricted calcium intake, sometimes improve osteopetrosis dramatically. However, calcitriol usually produces only modest clinical improvement, which is not sustained after therapy is discontinued. Recombinant human interferon ϒ-treatment with ϒ-interferon has produced long-term benefits. It improves white blood cell function, greatly decreasing the incidence of new infections. With treatment, trabecular bone volume substantially decreases and bone marrow volume increases. This is seen to produce increases in hemoglobin, platelet counts, and survival rates [10].
Bone marrow transplantation-Bone marrow transplantation markedly improves some cases of infantile osteopetrosis [1]. It can cure bone marrow failure and metabolic abnormalities in patients whose disease arises from an intrinsic defect of the osteoclast lineage. It is the only curative treatment for this disease. However, it may be limited to a subset of patients whose defects are extrinsic to the osteoclast lineage and whose condition is unlikely to respond. Patients with crowded bone marrow are less likely than others to respond to a transplant. Surgical management has a very limited role in such patients. It is necessary in cases of fractures as these patients are more prone for fractures.
Conclusion
Osteopetrosis is rare disease but one can consider this disease in the infant with leucoerythroblastic blood picture with cytopenias and hepatosplenomegaly and complete radiological investigations should be done to confirm the diagnosis. Histomorphometric studies of bone may be useful to predict the likelihood that bone marrow transplantation will succeed.
References
- Mazzolari E, Forino C, Razza A, et al. A single-center experience in 20 patients with infantile malignant osteopetrosis. Am J Hematol. 2009;84:473–9.
- Albers-Schönberg HE. Röntgenbilder einer seltenen Knockenerkrankung. Munch Med Wochenschr. 1904;5:365–8.
- Albuquerque MA, Melo ES, Jorge WA, et al. Osteomyelitis of the mandible associated with autosomal dominant osteopetrosis: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:94-8.
- Bakeman RJ, Abdelsayed RA, Sutley SH, et al. Osteopetrosis: A review of the literature and report of a case complicated by osteomyelitis of the mandible. J Oral Maxillofac Surg. 1998;56:1209-13.
- Pinto RG, John I, Qabazard Z. Osteopetrosis associated with hyperkalaemia: A case report. Kuwait Med J. 2003;35:216-8.
- Kaya D, Tüzün E, Dinçer A, et al. A rare case of multiple sclerosis and cerebral hemorrhage associated with osteopetrosis. Diagn Interv Radiol. 2010;16:16-9.
- Nakayama J, Fujioka H, Kurosaka M, et al. Surgery for clavicular and humeral fractures in an osteopetrotic patient: A case report. J Orthop Surg. 2007;15:251-4.
- Loria-Cortes R, Quesada-Calvo E, Cordero-Chaverri C. Osteopetrosis in children: A report of 26 cases. J Pediatr. 1977;91:43-7.
- Key L, Carnes D, Cole S, et al. Treatment of congenital osteopetrosis with high-dose calcitriol. N Engl J Med. 1984;310:409-15.
- Key LL Jr, Rodriguiz RM, Willi SM, et al. Long-term treatment of osteopetrosis with recombinant human interferon gamma. N Engl J Med. 1995;332:1594-9.