Research Article - Current Pediatric Research (2018) Volume 22, Issue 1
Individual and community level factors associated with defaulting of immunization among 12-59 months children in Ethiopia: Multilevel modeling analysis using 2011Ethiopia demographic and health survey.
Birhanu Jikamo Bago1*, Wondwossen Terefe2, Gebremeskel Mirutse21School of Public and Environmental Health, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia.
2Department of Public Health, College of Health Sciences, Mekelle University, Mekelle, Ethiopia.
- Corresponding Author:
- Birhanu Jikamo Bago
School of Public and Environmental Health
College of Medicine and Health Sciences
Hawassa University, Hawassa, Ethiopia
Tel: 251910440682
E-mail: bjikammo@gmail.com
Accepted date: March 27, 2018
Abstract
Introduction: Currently immunization prevents an estimated 2 to 3 million deaths every year. However; in 2012, 22.6 million children under one year of age who received first dose of diphtheria, pertussis, tetanus (DPT1) did not receive third dose of (DPT3) vaccine. Out of this 70% of children live in ten countries and Ethiopia is one of those countries. Objective: The aim of this study was to determine individual and community level factors associated with defaulting of immunization among 12-59 months children in EDHS, 2011. Methods: Source of data for this study was EDHS 2011. Sample from 592 clusters of 6,497 unweighted children and 6,666 weighted children among age group of 12-59 months. Multilevel regressions were used to identify predictors of defaulting of child immunization. Possible model diagnostic tests were addressed while building the model by stepwise forward. Four models were built to estimate both fixed effects of the individual and community-level factors and random effects between-cluster variation on defaulting of child immunization. Presence of confounders and interaction effects was investigated by computing relative changes on ß coefficients at a cutoff point 15%. A p<0.05 was used to identify significantly associated factors with defaulting of child immunization. Results: The current study found that more than three-fourth (78%) of children among age group of 12-59 months were missed one or more doses of recommended vaccine. Perceived problem of distance to reach a health facility (AOR=1.24; 95% CI: 1.01, 1.52) and nonexposure to media (AOR=1.53; 95% CI: 1.21, 1.93) had higher association with defaulting of child immunization. With regard to the community-level factors, communities living in Affar region (AOR=8.69, 95% CI: 4.33, 17.42) and communities living in Oromia region (AOR=3.82, 95% CI: 2.27, 6.44) had a positive influence on defaulting of child immunization. Conclusion and recommendation: In Ethiopia significant proportion of children was missed one or more doses of immunization. The current study found that, perceived problem of distance to reach a health facility, mother’s exposure to media, religion, child’s vaccination cards, birth order, mother’s empowerment in major decision on household issue and regions have association with defaulting of immunization. Thus, efforts to decrease the proportion of defaulter rate better to focus both on individuals and communities.
Keywords
Community-level factors, Individual-level factors, Two-level mixed effect, Clusters.
Introduction
Background
Vaccination is one of the important public health interventions and a cost effective strategy to decrease both the morbidity and mortality associated with communicable diseases [1]. Defaulting of immunization refers children who missed one or more doses of recommended vaccine based on Expanded Program on Immunization (EPI) [2].
World Health Organization (WHO) report, currently immunization prevents an estimated 2 to 3 million deaths every year from diphtheria, tetanus, pertussis and measles [3]. However; the benefits of vaccination have not yet reached many of those living in low and middle income countries, which carry the major burden of vaccinepreventable diseases [4].
Vaccination of children has continued to a significant reduction in morbidity and mortality from different vaccine preventable diseases [5]. Among those childhood deaths: nearly199 000 deaths caused by haemophilus influenza type b (hib), 195000 by pertussis, 118 000 by measles, 59000 by neonatal tetanus, 476 000 by pneumococcal disease, and 453 000 by rotavirus [3].
Summary of Global Immunization Coverage report in 2012 reported that, worldwide defaulter rate of children who received first doses of (DPT1), 6.7% of children did not receive third dose of (DPT3) and from those children who received (BCG) vaccine, 4.5% of children did not receive measles vaccine [6]. In the same report in Sub- Saharan Africa defaulter rate of children who received first dose of DPT1, 10% of children did not receive third dose of DPT3 and from those children who received BCG vaccine, 6.3% did not took measles vaccine [6]. In 2012, WHO, 22.6 million children under one year of age who received first dose of diphtheria, pertussis, tetanus (DPT1) did not receive third dose of diphtheria, pertussis, tetanus (DPT3) [3]. Out of this 70% of children live in ten countries and Ethiopia is one of those countries.
Defaulted children were at risk for morbidity, mortality and outbreaks of vaccine preventable diseases. According to 2016 Ethiopia Demographic and Health Survey (EDHS) report, four in ten children age 12-23 months (39%) received all basic vaccinations at some time and 22% received these vaccinations before their first birthday [7]. In Ethiopia, the vaccination coverage among children age 12-23 months is highest for the first dose of polio vaccine (81%) followed by first dose of DPT-HepB-Hib vaccine (73%). More than half (53%) of children in Ethiopia have received three doses of DPT-HepB-Hib vaccine and 54% received the measles vaccination [7]. There is a 20 percentage-point dropout rate at the national level from the first to the third dose of DPT-HepB-Hib vaccine and a 25 percentage-point dropout rate from the first to the third dose of polio vaccine [7].
There were studies conducted on defaulting of child immunization at district levels in Ethiopia [8,9]. The weakness of those previous studies were the use of single level analytical techniques that did not take into account clustering and the hierarchical structure of data for individuals living in different households, cities and enumeration areas. Multilevel modeling can account for factors at individual and community level simultaneously and afford a more robust understanding of the factors associated with defaulting of child immunization [10].
On the other hand; when the correlation with the group level is ignored and a single level analytical method is used; it might lead to violation of the assumption of independency between observations in a group. In addition to that, ignoring group level effect generally lead to underestimation of the standard errors and produce false significant results and as a result to incorrect conclusions on effect sizes [10]. Efforts toward achieving healthy children are very critical to stakeholders on Maternal Neonatal and Child Health (MNCH). Therefore, the aim of this study was to determine individual and community level factors associated with defaulting of immunization among 12-59 months children in Ethiopia Demographic and Health Survey (EDHS), 2011.
Methods and Materials
Study Design
The 2011 Ethiopia Demography and Health Survey (EDHS) used a community-based cross-sectional study throughout the country and in this study no particular design was used rather data collected was supplementary analyzed to determine individual and community level factors associated with defaulting of immunization among 12-59 months children in Ethiopia (EDHS), 2011.
Study Setting
The study was conducted at the national level of the country Ethiopia. Ethiopia is a country at Horn of Africa with total area of around 1.1 million square kilometers [11,12]. In 2013 Ethiopian National Statistics Agency report, country’s total population was 86,613,986 and it is the second-most populous nation in Africa [13]. Children under the age of one and women of 15-49 years of age group were the targets for the EPI program according to Ethiopian immunization policy of 2007[5]. In 2011, estimated children under one year of age in Ethiopia was 1,924,910 [14]. The third round EDHS 2011 was collected over a five-month period from 27 December, 2010 to 3 June, 2011.
Source of Population
Source population for this study was women among age group of 15-49 years those who have children among age group of 12-59 months who were living in the selected enumeration areas.
Inclusion Criteria
Children among age group of 12-59 months who received at least one dose of recommended vaccine during their first year of age were included in this study.
The reason for choosing children who had celebrated their first year of life was due to their acceptance age for the recommended vaccines. Additionally; WHO and UNICEF guide line recommended complete vaccination of children until they celebrate their first year of life [11].
Exclusion Criteria
Children whose age was not correctly registered at the time of survey.
Study Population
The study population for this study was children who satisfied eligibility criteria were included.
Sample Size Determination and Sampling Procedure
In the 2011 EDHS, representative samples of 17,385 eligible women were identified for individual interview. Complete interviews were conducted for 16,515 women in their, yielding a response rate of 95%.
The sample size for this specific study was drawn from children among age group of 12-59 months who received at least one dose of recommended vaccine during their first year of age were included in this research. Therefore; this study focused on a sample of 6,497 unweighted children and 6,666 weighted children who received specific vaccine during their first year of age before the survey.
The 2011 EDHS used a stratified sampling procedure in two stages using the 2007 population and housing census (PHC) as a frame. Stratification was achieved by separating each region into urban and rural areas. In the first step clusters were selected from the list of census enumeration areas. The sample included 624 enumeration areas, 187 in urban and 437 in rural areas. In the second stage a complete list of households in each selected cluster was carried out and households were selected by systematic sampling. The EDHS sampling procedure was used for this study.
Data Collection Tool
The source of data for this specific research question was the 2011EDHS conducted throughout the country in September 2010. The 2011 EDHS tool has three components: the household questionnaire, the woman’s questionnaire and the man’s questionnaire. These questionnaires were adapted from model survey instruments developed for the MEASURE DHS project to reflect the population and health issues relevant to Ethiopia. The data for determining individual and community level factors was taken from woman’s questionnaire. The variables reviewed to be important for this specific research were collected from the Stata filled data received from http://www.measuredhs. com and these data were transferred and open into a Stata Software version 12.
Data Quality and Management
The quality of the data was maintained by checking its completeness, cleaning the missing values by running frequencies and some of the variables were re-coded into the same variable like age of the mother at birth and mothers education.
Study Variables
Dependent variable: Defaulting of child immunization is the dependent variable. It refers to children among age group of 12-59 months who missed one or more doses of recommended vaccine based on EPI program. It was dichotomized in to two as: Success=defaulter of immunization given value of “1” and Failure=nondefaulter of immunization given value of “0.” Nondefaulter of immunization refers children among age group of 12-59 months who received all recommended vaccines based on EPI program.
Independent variables: Individual and communitylevel factors for defaulting of child immunization were extracted from EDHS 2011.
Individual-Level Factors
Socio-economic factors
Mother’s and husband’s education: For both of these variables, the original category in the EDHS was adopted with no change as to categorize as: no education, primary education, secondary education and higher education. However, secondary and higher education were merged since their proportion was small and mothers who attended secondary school and higher education may not differ significantly with defaulting of child immunization.
Mother’s and husband’s occupation: These variables in the EDHS were collected data on mothers and husbands occupational status as: ‘no job’ or as a list of different jobs. The sorts of job collected for both mothers and husbands ranged from unskilled manual to professional. In the current study, the responses were categorized into two: ‘no job’ or ‘have job’ regardless of the type of job. The ‘no job’ category for mothers does not mean that mother’s did not perform any activities; rather, mother’s was limited to household activities.
Wealth index: Is derived from the different assets of the households in order to assess the household’s cumulative living standard. There were five categories; the original category in the EDHS was adopted with no change as categorize to: poorest, poorer, middle, richer, and richest.
Exposure to mass media: Frequency of listening to radio and watching television were considered as exposure to mass media in the current study by excluding exposure to magazines and newspapers. For the reason that, proportion of mother’s in Ethiopia have lower literacy rates, poor distribution print media outside of the capital city and serve small portion of the population. There were three categories for this variable: not exposure to radio and television, exposed to either radio or television, exposure to both radio and television in one week course.
Child’s vaccination card: Vaccination cards were used to identify children who have vaccination cards and those children who have not cards at the time of survey.
Woman’s empowerment in major decisions on household issues: Focused on four attributes from the EDHS data to describe women who were: (i) usually decide on respondent's health care; (ii) usually decides on large household purchases; (iii) usually decides on visit to family or relatives; and (iv) usually decides what to do with money husband will earns. There were five categories for this variable based on the number of these decisions, in which women participate as: involved in four of the decisions, involved in three of the decisions, involved in two of the decisions, involved in one of the decisions, not involved in any of the decisions. Woman was considered to be empowered if she decides on all of above the items listed by the woman alone or together with her partner.
Socio-Demographic Factors
Age of mother: Measured in year which the age was categorized into three groups: 15-24years; age 25-34years; and age 35-49 years.
Religion: The dominant religion in the country was: Orthodox, Muslim, and Protestant with minorities was merged into one category and labeled as ‘other’.
Birth order: This variable indicates that the order of birth. Indirectly, it pointed out the parity of the mothers. There were four categories for this variable as: those first born child, second and third born child, 4th and 5th born child and 6th and above born child.
Marital status: There were two categories for this variable as: living with partner; not living with partner. The former included women formally married and women living with a partner as married, while the latter contained nevermarried women as well as those widowed, divorced or separated.
Health Care Utilization Factors
Place of delivery: The responses for place of delivery collected in the EDHS data were two categories as: home delivery, and different (governmental health facilities, different types of private health facilities and others).
Perception of provider availability: The survey question asked women if provider availability was a problem for them to get any medical help from health institutions, not limited to child immunization services. There were two categories for this variable as: ‘yes, big problem’: or, ‘not big problem’. Was used the same codes for this study.
Perception of distance to a health facility: The survey question asked women if distance was a problem for them to get any medical help from health institutions, not limited to child immunization services. There were two categories for this variable as: ‘yes, big problem’: or, not big problem.
Perception of drugs availability: The survey question asked women if drugs availability was a problem for them to get any medical help from health institutions, not limited to child immunization services. There were two categories for this variable as: ‘yes, big problem’: or, ‘not big problem’.
1. Community-level factors
2. Community-level socio-economic factors
3. Defining community aggregates
The EDHS did not collect data that can directly describe the characteristics of the clusters except place of residence and region. Therefore; other community level variables were generated by aggregating the individual characteristics with our interest in a cluster. The aggregates were computed using the proportion of a given variables’ subcategory we were concerned on in a given cluster. Since the aggregate value for all generated variable was not normally distributed. It was categorized into groups based on the national median values. Similar procedure was used for the following aggregate variables.
Community poverty status: It is defined as the proportion of poor or poorest mothers within the cluster. Within the cluster proportion of poor or poorest were aggregated and show over all poverty status within the cluster. There were two categories for this variable with reference to the national median value; higher proportion of poor/poorest mothers and lower proportion of poor or poorest mothers within the cluster.
Community unemployment rate: Defined as the proportion of mothers who had no job within the cluster. This aggregate show overall unemployment rate of women within the cluster. There were two categories for this variable with reference to national median value; lower proportion of mother’s unemployed and higher proportion of mother’s unemployed within the cluster.
Community women education: Was defined as the proportion of mother’s who attended primary/secondary/ higher education within the cluster. The aggregate of individual mother’s primary/secondary/higher educational attainment can show the overall educational status of women within the cluster. There were two categories for this variable with reference to the national median value: higher proportion of mother’s who attended primary/secondary/higher education and lower proportion of mother’s who attended primary/secondary/higher education within the cluster.
Community institutional delivery: It is defined as the proportion of mother’s who delivered their child in the health institution within the cluster. The aggregate of individual mothers who delivered their child in the health institution within the cluster can show the overall institutional delivery of the cluster. There were two categories with reference to the national median value; lower proportion of mother’s who delivered their child in the health institution, and higher proportion of mother’s who delivered their child in the health institution within the cluster.
Community media exposure: Was defined as the proportion of mother’s who were exposed at either radio or television or both radio and television within the cluster in the course of week. The aggregate of individual mothers who were exposed at either radio or television or both radio and television can show the overall media exposure of mother’s within the cluster. There were two categories for this variable: with reference to the national median value; lower proportion of mother’s who were exposed at either radio or television or both radio and television within the cluster, and higher proportion of mother’s who were exposed at either radio or television or both radio and television within the cluster.
Community ANC utilization: Was defined as the proportions of mother’s who visit antenatal care at least one visit within the cluster. The aggregate of individual mother who visit antenatal care at least one visit can show the overall antenatal care utilization of mother’s within the cluster. There were two categories for this variable: with reference to the national median value; lower proportion of mother’s who visit antenatal care at least one visit and higher proportion of mother’s who visit antenatal care at least one visit within the cluster.
Community distance to a health facility: Was defined as the proportion of mother’s who report distance to reach a health facility was a big problem to get medical help within the cluster. The aggregate of individual mothers who report distance to a health facility was a big problem to get medical help within the cluster can show the overall mother’s distance was a big problem to get medical help. There were two categories for this variable with reference to the national median value; lower proportion of mother’s who report distance to a health facility was a big problem and higher proportion of mother’s who report distance to a health facility was a big problem to get medical help within the cluster.
Data Analysis
First data related with child immunization was extracted from children recode from the EDHS 2011 dataset. The data was cleaned, coded and analyzed by using Stata version 12. EDHS sample was not self-weighted and because of non-proportional allocation of different regions and urban-rural residences of the country that often be over-sampled in one region and under sampled in other region. Therefore, weighting of data has been computed to make sample representative of the entire population.
Descriptive statistics was performed with both weighted and unweighted data to explain background characteristics of the individual’s and community’s where the individual are nested in enumeration areas.
Multilevel Regression Model
Considering the different level or hierarchical structure of the EDHS 2011 data the individual level variables (level 1), were as nested within selected enumeration areas (level 2). The units of analysis were usually individuals (at a lower level) who were nested within community-level variables (at a higher level). The traditional logistic regression model assumes independency between observations. But data with hierarchical nature often have a dependency within the higher level of the hierarchy. Therefore; to take this effect into account; multilevel modeling is applied [15].
The Intercept only Multilevel Regression Model (Null Model)
The first model was run without any predictors to test the random effect between-cluster variation on defaulting of child immunization. The intercept-only model is useful because it gives us an estimate of the intra-class correlation coefficient (ICC) and used to decide if the data justified using a multilevel approach was possible or not.
Individual Level Factors Multilevel Regression Model (Model II)
The second model was used to examine contribution of each individual-level factors on defaulting of child immunization. In addition to this, ICC was estimated and compared with its value obtained in the null model. Proportional change in variance (PCV) was calculated with reference to null model to look at relative contribution to explain defaulting of child immunization.
Community Level Factors Multilevel Regression Model
The third model was used to analysis only community level factors. This model allows us to examine whether the community-level explanatory variables explain betweencluster variation on the defaulting of child immunization. Similarly; ICC was estimated and its change from the null model was assessed. PCV was calculated with reference to null model to look at relative contribution to explain defaulting of child immunization.
Individual and Community Level Factors Multilevel Regression Model or Mixed Model
The fourth model was derived by mixing both individual and community-level factors simultaneously. In the same way as above; ICC was estimated and its change from the null model was assessed. PCV was calculated with reference to null model to look at relative contribution to explain defaulting of child immunization.
Crude multilevel regression model was developed for each factor against the dependent variable without controlling the effect of other explanatory variables. That explanatory variable whose crude multilevel regression model has a p-value<0.25 was the candidate for the adjusted multilevel regression model [16]. This is due to the data was secondary and we used p<0.25 is important for giving more chance for the variables in the analysis.
Adjusted multilevel regression model were built with all the candidate predictors found in the crude association. Four models were built to estimate both fixed effects of the individual and community-level factors and random effects between-cluster variation on defaulting of child immunization. In this model measure of association was reported as Adjusted Odds Ratio (AOR) with 95% CIs, by controlling the effect of other predictors. A p-value<0.05 was used to identify factors significantly associated with defaulting of child immunization.
Model Building
All models were built by using stepwise forward method of model building technique. This method was chosen because of shorter computation time it takes while running the models [17]. In addition to this, it is useful for developing the best prediction equation from the smallest number of variables.
Model Diagnostics for Multilevel Model
Use of model diagnostic statistics is important to assess adequacy of the model. Existence of confounding or interaction effects among predictors was checked by using beta change for a given variable at a cutoff point greater than 15% [18].
If percentage of beta change in a given variable is greater than 15%, then the variable which brought this change have a confounding or interaction effect. To check the interaction effect of the variable, new variable was created by multiplying the two variables (a product term). If percentage of beta change in a given variable is greater than 15%, then the variable which brought this change have a confounding or interaction effect. To check the interaction effect of the variable, new variable was created by multiplying the two variables (a product term).
If the new variable become statistically significant at p-value<0.05, then this variable was considered to have an interaction and the product term was kept in the final model. But if the product term was not significant in the model, it was removed from the model and the variable, which brought the beta change, was considered as a confounder and was kept in the model. In the current study, two interaction effects were found. Perceptions of drugs availability no problem with perception of service provider were a problem were the first interacting variables. The second interaction was between perception of drugs availability was a problem and perception of service provider was a problem.
Multicolinearity effect has been checked; due to its presence can produces imprecise estimates of slope and even the sign of the coefficients might be misleading [19]. This was done by using mean of variation inflation factor (VIF) value. Less than 5 mean VIF value indicates absence of extreme colinearity problem among explanatory variables in the regression model.
Goodness of fit test was checked by computing the Hosmer and Lemeshow goodness-of-fit [20]. The statistically nonsignificant value of the Hosmer-Lemeshow statistics has been confirmed for the model fitting the data reasonably well. The predicting ability of the model (model accuracy) has been evaluated using the Area under the ROC (Receiver Operating Characteristic) [21].
Operational Definition
Fully vaccinated was children among age group of 12 to 59 months who received all recommended vaccines based on EPI program including one dose of BCG, three doses of DPT, three doses of polio and one dose of measles vaccine at the time of survey.
Immunization defaulters: If the children among age group of 12 to 59 months who missed one or more doses of recommended vaccine based on EPI program.
Vaccinated: Children among age group of 12 to 59 months who received at least one dose of the recommended vaccines based on EPI program.
Unvaccinated: Children among age group of 12 to 59 months who did not receive any dose of the recommended vaccines based on EPI program.
Coverage by card plus history: Coverage calculated with numerator based on card and mother’s report.
Combined model: Combined model was used interchangeably with mixed model that refers to a model with both individual and community-level factors.
Mixed model: Mixed model was used interchangeably with combined model that refers to a model with both individual and community-level factors.
Infectious disease: Diseases that damages or injures the host so as to impair host function and caused by the presence and activity of a pathogenic microbial agent (e.g. viruses, bacteria, etc.).
Communicable disease: An infectious disease caused by germs spread from one person to another (contagious).
Unweighted sample: This sample was used for regression analysis.
Weighted sample: This sample was used for description of background characteristics of study population.
Ethical Consideration
For this study ethical clearance was sought from the ethical review committee of Mekelle University College of Health Sciences (CHS) with approval and supporting letter. Then the EDHS 2011 data was obtained and used with the prior permission of the Central Statistical Agency of Ethiopia. This was done first we registered for dataset access and write title and significance of the study on the website after complete a short registration form. Downloading of datasets was done by using the accessed website at www.measuredhs.com on request with the help of ICF International. Downloading data was only used for purpose of this study. The dataset was not passed by on to other researchers without consent of DHS. All DHS data were treated as confidential and no need to identify any household or individual respondent interviewed in the survey.
Results
Description of the Study Population by their Individual Level Background Characteristics in the EDHS2011
This study focused on a sample of 6,497 unweighted children and 6,666 weighted children who received specific vaccine during their first year of age before the survey. In the current study, more than three-fourth (78%) of children were missed one or more doses of recommended vaccine.
More than two third (67%) of mothers and half (50%) of husbands had no formal education. Nearly half (45%) of mothers were unemployed. In contrast, almost all (99%) of their husbands had jobs ranging from unskilled manual labor to professional occupations. By media exposure, 41% of the mothers did not listen to radio or watch television, while the rest listened to radio or watched television or both, in the course of a week (Table 1).
| Individual characteristics | n (unweighted) | % (unweighted) | n (weighted) | % (weighted) |
|---|---|---|---|---|
| Mother’s education | ||||
| No formal education | 4,322 | 66.52 | 4,475 | 67.14 |
| Primary education | 1,779 | 27.38 | 1,904 | 28.5 |
| Secondary and higher education | 396 | 6.1 | 287 | 4.3 |
| Husband’s education* | ||||
| No formal education | 3,203 | 49.61 | 3,277 | 49.45 |
| Primary education | 2,466 | 38.2 | 2,763 | 41.71 |
| Secondary and higher education | 787 | 12.19 | 586 | 8.84 |
| Mother’s occupation | ||||
| No job | 3,221 | 49.58 | 2,963 | 44.45 |
| Have job | 3,276 | 50.42 | 3,703 | 55.55 |
| Husband’s occupation* | ||||
| No job | 192 | 2.97 | 93 | 1.4 |
| Have job | 6,264 | 97.03 | 6,533 | 98.6 |
| Wealth index | ||||
| Poorest | 1,642 | 25.27 | 1,398 | 20.97 |
| Poorer | 1,193 | 18.36 | 1,466 | 21.99 |
| Middle | 1,074 | 16.53 | 1,333 | 19.99 |
| Richer | 1,161 | 17.87 | 1,365 | 20.47 |
| Richest | 1,427 | 21.96 | 1,104 | 16.58 |
| Exposure to mass media | ||||
| No exposure to TV/radio | 2,878 | 44.3 | 2,733 | 41 |
| Exposure to either TV/radio | 2,017 | 31.05 | 2,168 | 32.53 |
| Exposure to both TV & radio | 1,602 | 24.66 | 1,765 | 26.47 |
| Age of mother | ||||
| 15-24 years | 1,432 | 22.04 | 1,455 | 21.82 |
| 25-34 years | 3,461 | 53.27 | 3,533 | 53.01 |
| 35-49 years | 1,604 | 24.69 | 1,678 | 25.17 |
| Religion | ||||
| Orthodox | 2,377 | 36.59 | 2,823 | 42.35 |
| Protestant | 1,208 | 18.59 | 1,486 | 22.29 |
| Muslim | 2,744 | 42.23 | 2,149 | 32.24 |
| Others (traditional, catholic) | 168 | 2.59 | 207 | 3.11 |
| Child’s vaccination cards | ||||
| No cards | 3,407 | 71.97 | 3,805 | 74.89 |
| Have cards | 1,327 | 28.03 | 1,276 | 25.11 |
| Mother’s empowerment by number of major household decision* | ||||
| Made no major decision | 562 | 9.52 | 538 | 8.77 |
| Made one major decision | 570 | 9.65 | 525 | 8.56 |
| Made two major decision | 749 | 12.69 | 857 | 14 |
| Made three major decision | 1,223 | 20.71 | 1,227 | 20.03 |
| Made four major decision | 2,800 | 47.43 | 2,979 | 48.63 |
| Birth order | ||||
| First born child | 1,343 | 20.67 | 1,333 | 20 |
| 2nd and 3rd born child | 2,119 | 32.62 | 2,079 | 31.18 |
| 4th and 5th born child | 1,482 | 22.81 | 1,538 | 23.07 |
| 6th and above born child | 1,553 | 23.9 | 1,716 | 25.75 |
| Marital status | ||||
| Not living with partners | 559 | 8.6 | 512 | 7.68 |
| Living with partners | 5,938 | 91.4 | 6,154 | 92.32 |
| Sex of children | ||||
| Male | 3,286 | 50.58 | 3,396 | 50.95 |
| Female | 3,211 | 49.42 | 3,270 | 49.05 |
| Place of delivery | ||||
| Home delivery | 5,457 | 83.99 | 5,937 | 89.06 |
| Health facility | 1,040 | 16.01 | 729 | 10.94 |
| Perception of drugs availability | ||||
| Not a big problem | 2,172 | 33.43 | 2,593 | 38.9 |
| Big problem | 4,325 | 66.57 | 4,073 | 61.1 |
| Perception of provider availability | ||||
| Not a big problem | 2,328 | 35.83 | 2,751 | 41.26 |
| Big problem | 4,169 | 64.17 | 3,915 | 58.74 |
| Perception of distance to a health facility | ||||
| Not a big problem | 1,895 | 29.17 | 1,793 | 26.9 |
| Big problem | 4,602 | 70.83 | 4,873 | 73.1 |
*41, observation missing for husband education,
*41 missing from husband occupation
*593, observation missing for woman empowerment
*1,763, observation missing from child’s vaccination card.
Table 1: Background characteristics of individuals among age group of 12-59 months of children who received specific vaccine during their first year age before the survey in EDHS 2011, Ethiopia. #n(unweighted)=6,497 and #n(weighted)=6,666
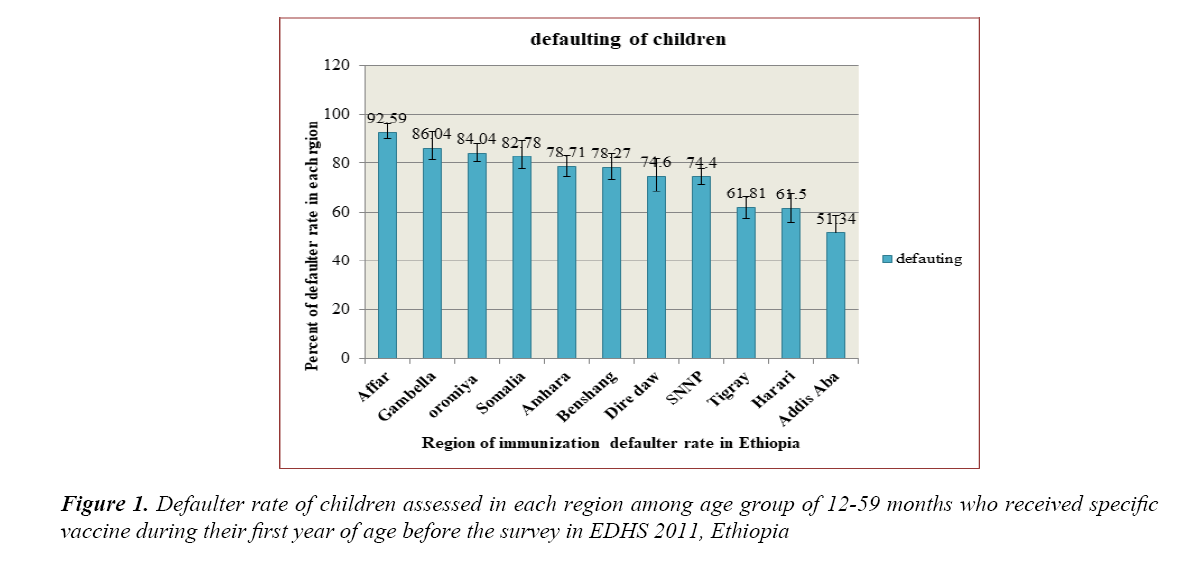
The proportion of defaulter rate in Ethiopia was higher in Affar region (92.59%) as compared with lowest in Addis Ababa (51.34%) (Figure 1).
Description of the Study Population by their Community level Background Characteristics in the EDHS2011
In the current study, 592 clusters were included in which all the children among age group of 12-59 months had lived. More than three-fourth (85.50%) of the clusters were in rural areas. The current study attempted to form community level factors by aggregating values of different individual characteristics. Accordingly, more than half (57%) of clusters were higher proportion of poverty status. Nearly two-third (66%) of clusters was lower proportion of unemployed. Nearly half (46%) of clusters were lower proportion of educated. Nearly half (45.5%) of the clusters were lower proportion of female educational attainment and 40.93% of clusters were lower proportion of media exposure to radio or television or both in the course of week (Table 2).
| Community Characteristics | n (unweighted) | % (unweighted) | n (weighted) | % (weighted) |
|---|---|---|---|---|
| Place of residence | ||||
| Urban | 1,277 | 19.66 | 967 | 14.5 |
| Rural | 5,220 | 80.34 | 5,699 | 85.5 |
| Region | ||||
| Tigray | 872 | 13.42 | 545 | 8.18 |
| Affar | 390 | 6 | 46 | 0.7 |
| Amhara | 833 | 12.82 | 1,699 | 25.49 |
| Oromia | 875 | 13.47 | 2,468 | 37.03 |
| Somalia | 380 | 5.85 | 133 | 1.99 |
| Benshangul-gumuz | 599 | 9.22 | 81 | 1.21 |
| SNNP | 943 | 14.51 | 1,469 | 22.04 |
| Gambella | 431 | 6.63 | 23 | 0.35 |
| Harari | 425 | 6.54 | 19 | 0.28 |
| Addis Ababa | 289 | 4.45 | 157 | 2.36 |
| Dire dawa | 460 | 7.08 | 26 | 0.39 |
| Community Unemployment | ||||
| Lower proportion of unemployed | 3,608 | 55.53 | 4,395 | 65.94 |
| Higher proportion of unemployed | 2,889 | 44.47 | 2,271 | 34.06 |
| Community Poverty Status | ||||
| Lower proportion of poor/poorest | 3,622 | 55.75 | 3,770 | 56.55 |
| Higher proportion of poor/poorest | 2,875 | 44.25 | 2,896 | 43.45 |
| Community Media Exposure | ||||
| Lower proportion of exposed | 3,149 | 48.47 | 2,729 | 40.93 |
| Higher proportion of exposed | 3,348 | 51.53 | 3,937 | 59.07 |
| Community Women Education | ||||
| Lower proportion of educated | 2,919 | 44.93 | 3,033 | 45.5 |
| Higher proportion of educated | 3,578 | 55.07 | 3,633 | 54.5 |
| Community ANC Utilization | ||||
| Lower proportion of utilized | 2,746 | 42.27 | 2,834 | 42.51 |
| Higher proportion of utilized | 3,751 | 57.73 | 3,832 | 57.49 |
| Community Institutional Delivery | ||||
| Lower proportion of delivered | 2,924 | 45.01 | 3,510 | 52.66 |
| Higher proportion of delivered | 3,573 | 54.99 | 3,156 | 47.34 |
| Community Distance to Health Facility | ||||
| Lower proportion of big problem | 3,620 | 55.72 | 3,437 | 51.56 |
| Higher proportion of big problem | 2,877 | 44.28 | 3,229 | 48.44 |
Table 2: Background characteristics of community’s among age group of 12-59 months of children who received specific vaccine during their first year of age before the survey in EDHS 2011, Ethiopia #n (unweighted)=6,497 and #n (weighted)=6,666
Interpretation of adjusted Multilevel Regression Result (Mixed Model Result)
Perception of distance problem to reach health facility had 24 % (AOR=1.24 95% CI 1.01, 1.52) higher odds of defaulting for immunization as compared with those mothers no problem related with distance, by controlling other predictors. Mothers who had no exposure to media had 53% (AOR=1.53; 95% CI 1.21, 1.93) higher odds of defaulting for immunization as compared with those mothers who exposed to media while holding all other predictors constant. Children who have no vaccination cards had 3.7 times (AOR=3.68; 95% CI 3.07, 4.41) higher likelihood of defaulting for immunization as compared with children who had vaccination cards while adjusting for all other predictors. Mothers who were not participate in major household decisions had 48% (AOR=1.48; 95% CI 1.06, 2.05) higher odds of defaulting for immunization as compared with mother’s who participate in four major household decision, by holding all other predictors constant (Table 3).
| Individual and Community Characteristics | Null Model | Model II AOR (95% CI) | Model III | Model IV AOR (95% CI) |
|---|---|---|---|---|
| AOR (95% CI) | ||||
| Mother’s Education | ||||
| No formal education | - | 0.93 (0.59, 1.45) | - | 1.23 (0.75, 2.01) |
| Primary education | 1.13 (0.72, 1.78) | 1.44 (0.90, 2.32) | ||
| Secondary and higher education | 1 | 1 | ||
| Husband’s Education | ||||
| No formal education | - | 0.78 (0.56, 1.09) | - | 0.81 (0.55, 1.19) |
| Primary education | 0.79 (0.57, 1.10) | 0.84 (0.58, 1.20) | ||
| Secondary and higher education | 1 | 1 | ||
| Mother’s Occupation | ||||
| No job | - | 1.15 (0.96, 1.38) | - | 1.05 (0.87, 1.27) |
| Have job | 1 | 1 | ||
| Wealth index | ||||
| Poorest | - | 1.30 (0.90, 1.88) | - | 1.25 (0.82, 1.89) |
| Poorer | 1.29 (0.89, 1.85) | 1.28 (0.85, 1.93) | ||
| Middle | 0.93 (0.65, 1.34) | 0.97 (0.65, 1.45) | ||
| Richer | 1.06 (0.75, 1.49) | 1.10 (0.75, 1.60) | ||
| Richest | 1 | 1 | ||
| Exposure to mass media | ||||
| No exposure to TV & radio | 1.52*** (1.21, 1.91) | 1.53*** (1.21, 1.93) | ||
| Exposure to either TV/radio | 1.15 (0.91, 1.44) | 1.13 (0.90, 1.43) | ||
| Exposure to both TV & radio | 1 | 1 | ||
| Religion | ||||
| Orthodox | - | 1 | - | 1 |
| Protestant | 1.51** (1.11, 2.05) | 1.22 (0.84, 1.79) | ||
| Muslim | 1.56** (1.21, 2.01) | 1.09 (0.80, 1.47) | ||
| Others (catholic, traditional) | 2.98** (1.50, 5.92) | 2.51* (1.24, 5.08) | ||
| Birth order | ||||
| First born child | - | 1 | - | 1 |
| 2nd and 3rd born child | 0.84 (0.65, 1.08) | 0.85 (0.66, 1.10) | ||
| 4th and 5th born child | 0.62** (0.48, 0.81) | 0.64** (0.49, 0.83) | ||
| 6th and above born child | 0.71* (0.54, 0.92) | 0.73* (0.55, 0.95) | ||
| Mother’s empowerment by number of major household decision | ||||
| Made no major decision | - | 1.62** (1.15, 2.25) | - | 1.48* (1.06, 2.05) |
| Made one major decision | 0.97 (0.72, 1.31) | 0.96 (0.71, 1.29) | ||
| Made two major decision | 1.21 (0.92, 1.58) | 1.18 (0.90, 1.54) | ||
| Made three major decision | 0.95 (0.76, 1.19) | 0.95 (0.76, 1.19) | ||
| Made four major decision | 1 | 1 | ||
| Child’s vaccination card | ||||
| No cards | - | 3.92*** (3.27, 4.70) | - | 3.68*** (3.07, 4.41) |
| Have cards | 1 | 1 | ||
| Sex of children | ||||
| Male | - | 1 | - | 1 |
| Female | 1.10 (0.93, 1.30) | 1.11 (0.94, 1.31) | ||
| Place of Delivery | ||||
| Home delivery | - | 0.76 (0.54, 1.07) | - | 0.77 (0.56, 1.06) |
| Health facility | 1 | 1 | ||
| Perception of drugs availability | ||||
| Not a big problem | 1 | 1 | ||
| Big problem | 0.98 (0.73, 1.32) | 0.99 (0.74, 1.33) | ||
| Perception of Provider Availability | ||||
| Not a big problem | - | 1 | - | 1 |
| Big problem | 1.28* (1.06, 1.55) | 1.25 (0.69, 1.51) | ||
| Perception of Distance to Health Facility | ||||
| Not a big problem | - | 1 | - | 1 |
| Big problem | 1.24* (1.01, 1.53) | 1.24* (1.01, 1.52) | ||
| Region | ||||
| Tigray | - | - | 1.45 (0.97, 2.16) | 0.64 (0.36, 1.13) |
| Affar | 12.30*** (6.76, 22.16) | 8.69*** (4.33, 17.42) | ||
| Amhara | 3.19*** (2.09, 4.86) | 2.21** (1.28, 3.80) | ||
| Oromia | 4.72*** (3.12, 7.14) | 3.82*** (2.27, 6.44) | ||
| Somalia | 3.65*** (2.15, 6.20) | 3.16*** (1.72, 5.78) | ||
| Benshangul-gumuz | 2.73*** (1.73, 4.30) | 2.17** (1.27, 3.69) | ||
| SNNP | 2.36*** (1.57, 3.54) | 1.53 (0.88, 2.67) | ||
| Gambella | 6.41*** (3.84, 10.68) | 2.86** (1.49, 5.48) | ||
| Harari | 1.24 (0.79, 1.79) | 1.09 (0.62, 1.92) | ||
| Addis Ababa | 1 | 1 | ||
| Dire Dawa | 2.68*** (1.69,4, 26) | 1.99 (0.91, 4.35) | ||
| Place of residence | ||||
| Urban | - | - | 1 | 1 |
| Rural | 0.94 (0.70, 1.24) | 0.75 (0.51, 1.11) | ||
| Community unemployment rate | ||||
| Lower proportion of unemployed | - | - | 1 | 1 |
| Higher proportion of unemployed | 1.05 (0.86, 1.29) | 1.01 (0.76, 1.31) | ||
| Community media exposure | ||||
| Lower proportion of exposed | - | - | 1.33*** (1.08, 1.65) | 1.10 (0.85, 1.44) |
| Higher proportion of exposed | 1 | 1 | ||
| Community mother’s education | ||||
| Lower proportion of educated | - | - | 1.06 (0.85, 1.32) | 1.10 (0.84, 1.43) |
| Higher proportion of educated | 1 | 1 | ||
| Community poverty status | ||||
| Higher proportion of poorer/poorest | - | - | 0.88 (0.71, 1.09) | 0.99 (0.75, 1.32) |
| Lower proportion of poorer/poorest | 1 | 1 | ||
| Community institutional delivery | ||||
| Lower proportion of delivered | - | - | 1.04 (0.84, 1.30) | 1.17 (0.92, 1.50) |
| Higher proportion of delivered | 1 | 1 | ||
| Community ANC utilization | ||||
| Lower proportion of utilized | - | - | 1.51*** (1.22, 1.87) | 1.24 (0.98, 1.57) |
| Higher proportion of utilized | 1 | 1 | ||
| Community distance from health facility | ||||
| Lower proportion of big problem | - | - | 1 | 1 |
| Higher proportion of big problem | 1.20 (0.98, 1.48) | 1.02 (0.79, 1.33) | ||
| Interaction between perception of drugs availability & perception of service provider availability | ||||
| Both drugs & service provider is not a big problem | - | - | NA | 1 |
| Drugs is not a big problem with service provider is a big problem | NA | 2.16** (1.25, 3.73) | ||