Case Report - Gynecology and Reproductive Endocrinology (2023) Volume 7, Issue 3
Incidental finding of bicornuate uterus in a primigravida associated with preeclampsia with severe features: A case report.
Ilikannu SO1, Adigba EO1, Jombo SE1*, Agadagba E1, Odo BC1, Ochuba CO2
1Department of Obstetrics and Gynaecology, Federal Medical Centre, Asaba, Nigeria
2Department of Public Health and Family Welfare, University of Port Harcourt, Choba, Nigeria
- Corresponding Author:
- Jombo SE
Department of Obstetrics and Gynaecology,
Federal Medical Centre,
Asaba,
Nigeria,
E-mail: jombosunday@yahoo.com
Received: 14-Mar-2023, Manuscript No. AAGGS-23-96739; Editor assigned: 17-Mar-2023, PreQC No. AAGGS-23-96739 (PQ); Reviewed: 31-Mar-2023, QC No. AAGGS-23-96739; Revised: 26-Apr-2023, Manuscript No. AAGGS-23-96739 (R); Published: 24-May-2023, DOI:10.35841/2591-7994-7.3.142
Citation:Ilikannu SO, Adigba EO, Jombo SE, et al. Incidental finding of bicornuate uterus in a primigravida associated with preeclampsia with severe features: A case report. Gynecol Reprod Endocrinol. 2023;7(3):142
Abstract
Abnormal fusion of the mullerian duct during embryonic life results in a variety of congenital malformations of the uterus. A bicornuate uterus is a rare congenital anomaly of the uterus which results from the partial fusion of the mullerian ducts, leading to varying degrees of separation of the uterine horns. It poses several obstetric complications like recurrent miscarriages, mal-presentation, preterm labour, intrauterine growth restriction and hypertensive disorders of pregnancy including preeclampsia. We present a 29 year old unbooked primigravida with features of preeclampsia with severe features and an unfavourable cervix at 35 weeks gestation. She subsequently had an urgent caesarean section with the outcome of a live male neonate that weighed 2.2 kg with good Apgar scores and an incidental finding of a bicornuate uterus. Successful pregnancies have been reported with this rare condition, however detailed examination with ultrasound and other investigation modalities could help pick this anomaly early enough for proper management to avert the morbidity that can ensue from this rare entity.
Keywords
Mullerian duct, Bicornuate uterus, Primigravida, Preeclampsia, Case report.
Introduction
Uterine anomalies result from agenesis or a defect in fusion or canalization of the mullerian duct. Mullerian ducts also called the paramesonephric ducts are embryological structures important for the development of the urogenital system. A bicornuate uterus is a very rare congenital anomaly of the uterus in which the uterus is heart-shaped as against the pear shape a normal uterus takes [1]. According to the classification of mullerian duct anomalies given by the American society for reproductive medicine, it falls in the class 4 category with others being unicornuate uterus, didelphis uterus, septate uterus, arcuate uterus, hypoplasia/agenesis and DES-related anomaly. The incidence of uterine anomalies varies and determining factors could include the population studied and the diagnostic techniques applied. An incidence of 3%-5% has been recorded in the general population, 2%-8% in subfertile women, 3.2%-6.9% of women with a history of recurrent miscarriage. Bicornuate uterus on its own represents 10%-39% of mullerian duct anomalies [2].
The bicornuate uterus is usually divided into bicornuate unicollis (one cervical canal) and bicornuate bicollis (two cervical canals) based on the partition of the cervix. This condition can be diagnosed before or during pregnancy. On many occasions, they may be asymptomatic and remain undiagnosed. Ultrasonography, Magnetic Resonance Imaging (MRI), Hysterosalpingogram (HSG), hysteroscopy and laparoscopy constitute modalities for making a diagnosis of this rare uterine anomaly. It is commonly associated with pregnancy complications such as recurrent pregnancy losses, preterm labour and rarely uterine rupture. Other complications that may arise include premature rupture of membranes and malpresentation. A higher incidence of intrauterine growth restriction and hypertensive disorders of pregnancy including severe preeclampsia have also been reported as complications that may arise from uterine anomalies such as in the bicornuate uterus [3]. Hence pregnancies in a bicornuate uterus are usually considered high-risk and require extra monitoring because of its association with poor reproductive outcomes. Menstrual complaints and primary infertility have also been associated with a bicornuate uterus. Women with a bicornuate uterus can experience successful pregnancies and can even go ahead to have uncomplicated vaginal deliveries. We, therefore, present a case of an incidental intraoperative finding of a bicornuate uterus that had a normal pregnancy that was terminated via caesarean section at 35 weeks gestation due to severe preeclampsia with good feto-maternal outcome [4].
Case Presentation
A 29 year old unbooked primigravida was referred from a secondary facility at 35 weeks gestation on account of severe preeclampsia following complaints of unremitting headache and epigastric pain of 5 days and 3 days respectively. On presentation, she was a young lady in no obvious distress, she was afebrile and not pale but had bilateral pitting pedal oedema up to the knees [5].
Her blood pressure was 180/110 mmHg while her pulse rate was 86 beats per minute. The abdomen was uniformly enlarged and moved with respiration with a symphysio-fundal height of 34 cm. The uterus harboured a singleton fetus in a longitudinal lie and cephalic presentation. There were no palpable contractions in ten minutes and the fetal heart was heard and regular. She had a normal vulva and vagina with a cervix that was 1 cm dilated, posterior, medium in consistency, 3 cm long with presenting part at station 0-3 giving her a bishop score of 2/13. An impression of preeclampsia with severe features and an unfavourable cervix was made [6]. She was counselled on the diagnosis and the need for an urgent caesarean section. She was subsequently stabilized and worked up for abdominal delivery. Blood pressure control was with the use of intravenous labetalol, seizure prophylaxis was via Pritchard’s regimen for Magnesium Sulphate (MgSO4) [7].
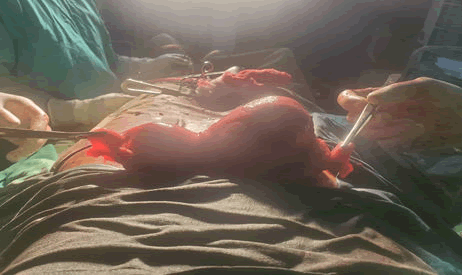
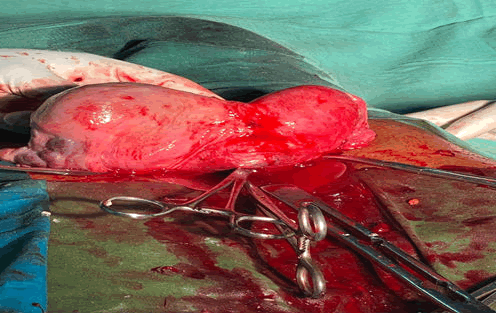
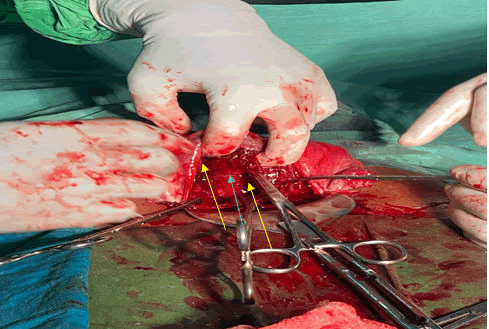
Her laboratory results showed a Packed Cell Volume (PCV) of 36%, a White Blood Cell (WBC) count of 6900 cells/mm3 and a platelet count of 220,000 cells/mm3. Urinalysis revealed proteinuria++, bedside clotting time was 8 minutes and her serum electrolytes, urea, creatinine and liver function tests were within normal limits. She had 2 units of O Rhesus D positive blood cross-matched for her. She had an urgent caesarean section with findings of a clean peritoneal cavity, not well-formed lower uterine segment, bicornuate uterus, clear and adequate liquor, live male neonate weighing 2.2 kg with apgar score of 6 and 8 in the first and fifth minute respectively [8]. There were grossly normal fallopian tubes and ovaries bilaterally on both horns of the uterus with an estimated blood loss of 600 mls. She had an uneventful post-operative recovery and was discharged after 5 days of admission to be followed up in the gynaecology clinic. She was satisfied with her treatment [9].
Results and Discussion
Uterine anomalies of which the bicornuate uterus is one of them are the result of mullerian or paramesonephric duct anomalies or disturbances at the time of fusion or development. An incidence of 3%-5% of uterine anomaly has been reported in the general population. Different classification schemes for female reproductive tract anomalies exist, but the most common classification was proposed by Buttram and Gibbons in 1979 and adopted by the American Society for Reproductive Medicine (ASRM) formerly the American fertility society in 1988. Within this system, the anomalies are grouped into mullerian hypoplasia/agenesis (group I), unicornuate uterus (group II), uterine didelphys (group III), bicornuate uterus (group IV), septate uterus (group V), arcuate uterus (group VI) and diethylstilbestrol related anomalies (group VII). Hence the index case fell into group IV of the ASRM classification. Bicornuate uterus (25%) and uterine didelphys (11%) have been reported as the most common of these anomalies [10].
Most cases of the bicornuate uterus are diagnosed during evaluation for gynaecologic or obstetric conditions but in the absence of symptoms, most anomalies remain undiagnosed until abdominal surgeries such as a hysterectomy or even a caesarean section. This was the case in our patient who had no menstrual problems prior to marriage, conceived within six months of marriage with no complication during pregnancy until 35 weeks gestation when she developed severe preeclampsia with the diagnosis of bicornuate uterus made intra-operatively. It is also important to note that the diagnosis was equally missed on two ultrasound scans done prior to the index admission [11].
Adverse pregnancy outcomes such as recurrent pregnancy loss, preterm birth, malpresentation, intrauterine growth restriction and fetal deformity have been associated with bicornuate uterus however, none of these were found in our patient. Some authors have also reported a higher incidence of hypertensive disorders of pregnancy including preeclampsia in patients with uterine anomalies compared to the general population [12]. Our patient had preeclampsia with severe features and an unfavourable cervix which was the indication for her caesarean section. Could a bicornuate uterus be the risk factor for her preeclampsia? Or was it her nulliparity?
Some workers have advocated for the routine use of cervical cerclage for pregnancies with a bicornuate uterus and other uterine anomalies due to preterm delivery that may ensue. However, cases of successful term singleton and twin pregnancies have been reported without cervical cerclage. Our patient did not have any cervical cerclage and carried her pregnancy to 35 weeks gestation before severe preeclampsia developed. There may be a need for further interventional studies to determine the effectiveness of routine cervical cerclage for pregnancies with a bicornuate uterus [13].
Hysterosalpingogram, a transvaginal ultrasound, magnetic resonance imaging, laparoscopy and hysteroscopy are investigative modalities for diagnosing a bicornuate uterus. The sensitivity of ultrasound in visualizing the rudimentary horn of a bicornuate uterus has been reported to be 23% which allows the diagnosis of only 14% of patients before the manifestation of clinical symptoms, this may have accounted for why the diagnosis was missed on ultrasound for our patient. Hence, machine resolution and the experience of the sonographer may contribute to the success of an ultrasound scan in making a diagnosis of a bicornuate uterus or other uterine anomalies. Radiologic differentiation of these uterine anomalies could be challenging occasionally. Widely diverging horns on HSG may suggest a bicornuate uterus; an intercornual angle greater than 105 degrees suggests a bicornuate uterus whereas less than 75 degrees indicates a septate uterus. Also with an MRI, an intrafundal downward cleft measuring ≥ 1 cm is indicative of a bicornuate uterus while <1 cm indicates a septate uterus. Laparoscopy and hysteroscopy have a role in both the definitive diagnosis and the treatment of uterine anomalies.
Surgical intervention through strassman metroplasty significantly reduces fetal loss (8%-12%) compared to patients without surgical treatment (70%-96%). It is usually reserved for women with recurrent pregnancy loss without any other identifiable risk factor. Laparoscopic and hysteroscopic metroplasty where available is a preferred alternative to the conventional open abdominal metroplasty with all the advantages of a minimally invasive procedure. However, the requisite skills and equipment are lacking in low and middleincome countries (Figures 1-3).
Conclusion
Although women with bicornuate uterus might have a successful pregnancy, they are still at risk of certain obstetric complications. Hence, a high index of suspicion, prompt diagnosis and a multidisciplinary approach to management may help to reduce the morbidity that may arise from this rare clinical entity.
Ethical Approval
Ethical approval was obtained from the ethics committee of the Federal medical centre, Asaba.
Competing Interests
The authors declare no competing interests.
Acknowledgment
The patient whose story is told in this case report gave her express approval with written consent for the publication of this report and accompanying images as her own way of contributing to the body of knowledge.
References
- Agarwal I, Tayade S, Sharma S, et al. A case report of a normal pregnancy in a bicornuate uterus through in vitro fertilization. Cureus. 2022;14(9):e29152.
[Crossref] [Google Scholar] [PubMed]
- Borgohain D, Srivastava S. Pregnancy in bicornuate uterus. Intern J Reprod Contrac Obst Gynecol. 2018;7(1):346-9.
- Adeyemi AS, Atanda OO, Adekunle AD. Successful pregnancy in one horn of a bicornuate uterus. Ann Afr Med. 2013;12(4):252.
[Crossref] [Google Scholar] [PubMed]
- Sugiura-Ogasawara M, Ozaki Y, Katano K, et al. Uterine anomaly and recurrent pregnancy loss. Semin Reprod Med. 2011;29(6):514-21.
[Crossref] [Google Scholar] [PubMed]
- Sasikala Mootha UB. Successful pregnancy in a case of bicornuate uterus with pre eclampsia and IUGR-a case report. Intern J Sci Res. 2013;4(1):316-17.
- Panagiotopoulos M, Tseke P, Michala L. Obstetric complications in women with congenital uterine anomalies according to the 2013 European society of human reproduction and embryology and the european society for gynaecological endoscopy classification: A systematic review and meta-analysis. Obstet Gynecol. 2022;39(1):138-48.
[Crossref] [Google Scholar] [PubMed]
- Gomez FG, Ruiloba FJ, Arellano FV, et al. Uterine anomalies associated with intrauterine growth restriction and hypertensive disorders during pregnancy [40K]. Obstet Gynecol. 2020;135:124S.
- Kurtz J, Stempel L. Uterine anomalies and hypertensive disorders of pregnancy: A retrospective study [1B]. Obstet Gynecol. 2017;129(5):20S.
- Gulavi E, Kyende Mutiso S, Mariara Muriuki C, et al. Successful pregnancy outcome after open strassman metroplasty for bicornuate uterus. Case Rep Obstet Gynecol. 2018;2018:4579736.
[Crossref] [Google Scholar] [PubMed]
- Goncalves E, Prata JP, Ferreira S, et al. An unexpected near term pregnancy in a rudimentary uterine horn. Case Rep Obstet Gynecol. 2013;2013:307828.
[Crossref] [Google Scholar] [PubMed]
- Crowley CM, Botros K, Hegazy IF, et al. Uterine didelphys: Diagnosis, management and pregnancy outcome. BMJ Case Rep. 2021;14(3):e242233.
[Crossref] [Google Scholar] [PubMed]
- Siwatch S, Mehra R, Pandher DK, et al. Rudimentary horn pregnancy: A 10-year experience and review of literature. Arch Gynecol Obstet. 2013;287(4):687-95.
[Crossref] [Google Scholar] [PubMed]
- Yasmeen S, Romano PS, Schembri ME, et al. Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol. 2006;194(4):992-1001.
[Crossref] [Google Scholar] [PubMed]