Research Article - Current Pediatric Research (2016) Volume 20, Issue 1
Incidence and Etiology of Acute Kidney Injury in Children Admitted to PICU using PRIFLE Criteria
Srinivasa S1, Reshmavathi V2*
1Professor and HOD, Department of Pediatrics, Kempegowda Institute of Medical Sciences, Bangalore, India.
2Junior Resident, Department of Pediatrics, Kempegowda Institute of Medical Sciences, Bangalore, India.
- *Corresponding Author:
- Dr Reshmavathi V
37, 1st Main, RMV 2nd Stage
Amarjyothi Layout, Sanjaynagar, Bangalore 560094, India.
Tel: 9902645747
E-mail: dr.reshma.venkatram@gmail.com
| Date of Acceptance |
January 30, 2016 |
Abstract
Introduction: Acute Kidney Injury (AKI) is associated with severe morbidity and mortality. Lack of consensus definition has been major limitation in improving outcomes. Acute Dialysis Quality Initiative Group (ADQI) group proposed RIFLE (Risk, Injury, Failure, Loss of function, End stage renal disease) criteria, criteria for defining AKI, later modified in children as pRIFLE (pediatric RIFLE). This study tries to address the need of limited data on pediatric AKI.
Methodology: A prospective study conducted in between December 2013 to May 2015. Serum creatinine level was estimated on all patients on admission and alternate days till discharge from Pediatric Intensive Care Unit (PICU). Urine output was recorded. Estimated Creatinine- Clearance (eCrCL) was calculated using Schwartz formula. AKI diagnosis and staging was based on pRIFLE (pediatric RIFLE) criteria. Either eCrCl or urine output criteria were used to diagnose and stage AKI, using criterion that leads to higher stage. Maximal stage that the patient progressed during the stay in PICU was assigned the stage for that case. Data was compiled using SPSS software.
Results: Of total 697 cases, 680 cases met inclusion criteria. Incidence of AKI was 178 (26.1%). Stage ‘Risk (R)’, ‘Injury (I)’ and ‘Failure (F)’ constituted 60.7% (108), 28.6% (51) and 10.6% (19) respectively. Maximum AKI occurred in < 1 year (28.1%) (p=0.003). Urine output and creatinine criteria matching were there in 77%. Infections were commonest etiology. Amongst infections dengue (30%) was most common, followed by sepsis (21.9%) and then pneumonia (17.9%). Hypotension, nephrotoxic drugs, sepsis, need for mechanical ventilation were significant (p<0.001) risk factors for AKI. Prerenal causes constituted 68% and renal 32%.
Conclusion: Incidence of AKI is high among critically ill children. pRIFLE staging system that provides early identification and stratification of AKI. Infections are leading etiology of AKI in children.
Keywords
AKI, pRIFLE, PICU
Introduction
Acute Kidney Injury (AKI) has become a major global
health care challenge with an estimated 13.3 million cases
per year leading to an estimated mortality of 1.7 million
deaths per year globally. Increasing prevalence of AKI
is strongly associated with increased early and long term
patient morbidity and mortality [1]. According to recent
meta-analysis conducted by Paweena et al the pooled
incidence rate of AKI was 33.7% (95% CI, 26.9 to 41.3)
and AKI-associated mortality rates was 13.8% in children
(95% CI, 8.8 to 21.0) [2].
“0 by25” is an ambitious initiative of International Society
of Nephrology which aims to eliminate preventable deaths from Acute Kidney Injury worldwide by 2025. This
initiative emphasizes the magnitude of the problem, the
global concern about AKI and its endeavour to eliminate
mortality and morbidity due to AKI.
Acute kidney injury previously called acute renal failure
is characterized by a reversible increase in the blood
concentration of creatinine and nitrogenous waste products
and by the inability of the kidney to appropriately regulate
fluid and electrolyte homeostasis [3]. If left untreated, the
condition has a high risk of multiple organ failure and
potentially death. Patients who suffer from AKI may have
subsequent renal dysfunction after original injury. Children
are more susceptible for this dysfunction [4].
For a long time there was lack of consensus on definition of
AKI. In 2005, the first consensus definition of AKI for the adult
population, based on the RIFLE (Risk, Injury, Failure, Loss
of function, End stage renal disease) criteria, was proposed
by the Acute Dialysis Quality Initiative Group (ADQI) [5].
The definition was later modified and evaluated in critically
ill pediatric patients and termed pRIFLE (Pediatric RIFLE)
criteria. The pRIFLE criteria differs from RIFLE criteria,
in that a) Only decrease in estimated creatinine clearance
(eCrCL), and not the change in glomerular filtration rate, is
used to determine grading b) The eCrCl is estimated using the
Schwartz formula, which incorporates the height and serum
creatinine level of the patient, and an age adjusted constant c)
pRIFLE incorporates a longer duration of urine output than in
adult RIFLE classification.
The spectrum and burden of AKI in developing countries
may be different from that of developed countries [6] The
patients from developing countries are younger, infection
associated AKI is more common and a significant
proportion may have already developed AKI at the time
of hospitalization. In addition, resource limitations in
managing children who require renal replacement therapy
add to the burden [7,8].
Most of the studies in AKI are based on adult population.
The incidence and clinico-etiological profile of AKI
varies from adults to children. Of the pediatric studies on
incidence of AKI, many are limited to developed countries
and often retrospective [9]. Hence limited data availability
on clinical profile of pediatric AKI from Indian children,
fallacies of retrospective studies, and regional variations in
the profile of AKI makes it compelling to study incidence
and outcome of AKI in pediatric patients and current study
tries to address this need.
Methodology
This was a Prospective and observational study conducted
at Kempegowda Institute of Medical Sciences, Bangalore.
All patients within the age group of 1 month to 18 years
admitted to Pediatric Intensive Care Unit (PICU) in
between December 2013 to May 2015 were included in
the study. Patients with known kidney disease and postoperative
cases were excluded from the study.
The study was approved by the Institute Ethics
Committee. Informed consent was taken from parents of
all participants. Detailed clinical history and examination
was done, co-morbidities were noted, and relevant data
regarding investigations was collected for all children
admitted to PICU.
Serum creatinine levels were estimated by modified Jaffe
method, which is quick, simple, reliable and inexpensive
method of creatinine estimation [10]. Serum creatinine
was estimated on all patients admitted to PICU on the
day of admission and on alternate days till discharge from
PICU. Serum creatinine may be repeated frequently in
children who develop shock, sepsis, need for ventilation, inotropes or diuretics. Creatinine estimation was done at
daily intervals in those patients with AKI.
Estimated creatinine clearance (eCrCL) was calculated
using Schwartz formula [11]. Age related creatinine
clearance was taken as the baseline CrCl.
Urine output measured and recorded as ml/kg/hour. Only
patients who were catheterized were considered for urine
output criteria.
Diagnosis and staging of AKI was based on Pediatric
RIFLE definition & classification. Either eCrCl or urine
output was used to diagnose and stage AKI, using a
criterion that leads to higher stage classification. Shock
was defined in presence of tachycardia, feeble pulses, cool
peripheries, hypotension (blood pressure <-2 Standard
deviation (SD) for age and sex) or capillary filling time > 3
seconds. Sepsis was the presence of systemic inflammatory
response syndrome with suspected or proven infection
[11]. The diagnosis of prerenal vs renal was decided based
on clinical diagnosis and supported by progressively
increasing serum creatinine values, even after 48 hours of
admission and appropriate fluid therapy (Table 1).
| |
Estimated Creatinine Clearance (eCrCl) |
Urine output |
| Risk |
 decrease by 25% |
<0.5 ml/kg/h for 8 h |
| Injury |
 decrease by 50% |
<0.5 ml/kg/h for 16 h |
| Failure |
decrease by 75% or eCrCl<35 ml/min/1.73 m2 |
<0.3 ml/kg/h for 24 h or anuric for 12 h |
| Loss |
Persistent failure >4 weeks |
|
| End stage |
End-stage renal disease (persistent failure >3 months) |
|
eCCl, estimated creatinine clearance; pRIFLE, pediatric risk, injury, failure, loss and end-stage renal disease.
Table 1: Classification/staging system for acute kidney injury.
Estimated GFR for children is calculated using
SCHWARTZ formula
k = 0.45 for infants 1 to 52 weeks old
k = 0.55 for children 1 to 13 years old
k = 0.55 for adolescent females 13-18 years old
k = 0.7 for adolescent males 13-18 years old
The maximal stage that the patient progressed during the
stay in PICU was assigned the final stage for that case. The
patients were evaluated to ascertain the etiology of AKI
and its progression and were followed until discharge.
Statistical analysis
The incidence of AKI in children is approximately 5%
among non-critically ill and 30% in critically ill according
to Basu and Askenazi et al [4,12].
In order to estimate these incidence rates at 95% confidence,
and precision of 2.5% for the non-critically ill and 9% for
critically ill, the minimum required sample sizes were 304
and 104, respectively (Formula used is n=z21-α/2 P(1-P)/€2
where z= 95% power and 5% level of significance (1.96), P
is the incidence, €= Absolute precision).The admissions to
our PICU in previous year were well above the minimum
required sample. Hence all the cases in the study period
were considered.
Descriptive and inferential statistical analysis has been
carried out in the present study. Results on continuous
measurements are presented on Mean ± SD (Min-Max)
and results on categorical measurements are presented
in Number (%). Significance is assessed at 5% level of significance. Student t test (two tailed, independent) has
been used to find the significance of study parameters on
continuous scale between two groups (Inter group analysis)
on metric parameters. Chi-square/ Fisher Exact test has
been used to find the significance of study parameters on
categorical scale between two or more groups. Multivariate
Logistic regression analysis was done to assess the risk
factors for development of AKI.
Statistical software
The Statistical software namely SAS 9.2, SPSS 15.0,
Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment
ver.2.11.1 were used for the analysis of the data and
Microsoft word and Excel have been used to generate
graphs, tables etc.
Results
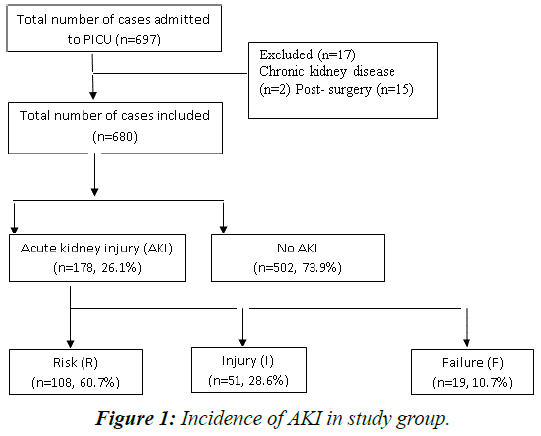
A total of 697 cases were admitted during the study period.
Of these 17 cases were excluded and 680 cases were
included in the study.
In this study, out of 680 included patients admitted to PICU
during the study period 178 had AKI making an incidence
of 26.1%. Stage ‘Risk’ comprised maximum cases with
60.7% (108 cases), followed by ‘Injury’ comprised 28.6%
(51 cases) and ‘Failure’ comprised 10.6% (19 cases).
Maximum AKI occurred in <1 year (28.1%) and incidence
was highest among younger age group (p=0.003) (Figure 1).
Figure 1: Incidence of AKI in study group.
Amongst the AKI cases creatinine criteria was used in all
cases while urine output criteria was applied for 190 cases.
RISK (R), INJURY (I) and FAILURE (F) cases were 108
(60.7%), 51(28.6%) and 19(10.7%) respectively by eCrCL
criteria. For urine output criteria, 74 cases of the 190 cases
had AKI. Among these 74 cases incidence of stage ‘R’ was
31%. ‘I’ was 46% and ‘F’ was 23% respectively (Table 2).
| Stage |
Creatinine Criteria |
Urine output Criteria |
| No AKI |
AKI |
Total |
No AKI |
AKI |
Total |
| No AKI |
502(100%) |
0(0%) |
502(73.8%) |
116(100%) |
0(0%) |
116(61.1%) |
| Risk |
0(0%) |
108(60.7%) |
108(15.9%) |
0(0%) |
23(31.1%) |
23(12.1%) |
| Injury |
0(0%) |
51(28.6%) |
51(7.5%) |
0(0%) |
34(45.9%) |
34(17.9%) |
| Failure |
0(0%) |
19(10.7%) |
19(2.8%) |
0(0%) |
17(23.0%) |
17(8.9%) |
| Total |
502(100%) |
178(100%) |
680(100%) |
116(100%) |
74(100%) |
190(100%) |
P<0.001**, Significant, Chi-Square test
Table 2: Creatinine and urine output criteria stage in relation to incidence of AKI.
Urine output criteria was applied for 74 of all AKI
cases and there was matching between urine output and
creatinine criteria in 57 cases (77%). There was 39.1%
matching in stage ‘RISK’, 91.2% in stage ‘INJURY’ and
100% in stage ‘FAILURE’ (Table 3).
| Final Rifle stage |
Urine output stage (U) |
Total |
| RU |
IU |
FU |
| Risk |
9(39.1%) |
1(2.9%) |
0(0%) |
10(13.5%) |
| Injury |
14(60.9%) |
31(91.2%) |
0(0%) |
45(60.8%) |
| Failure |
0(0%) |
2(5.9%) |
17(100%) |
19(25.7%) |
| Total |
23(100%) |
34(100%) |
17(100%) |
74(100%) |
Table 3: Matching between creatinine criteria staging and urine output staging.
In this study maximum AKI occurred in <1 year and
incidence was highest among younger age group (p=0.003)
(Table 4).
| Age in years |
Final Rifle Stage |
Total |
| No AKI |
AKI |
| <1 yr |
110(21.9%) |
50(28.1%) |
160(23.5%) |
| 1-2 yrs |
96(19.1%) |
35(19.7%) |
131(19.3%) |
| 2-5 yrs |
86(17.1%) |
43(24.2%) |
129(19%) |
| 5-10 yrs |
71(14.1%) |
27(15.2%) |
98(14.4%) |
| 10-15 yrs |
97(19.3%) |
18(10.1%) |
115(16.9%) |
| >15 yrs |
42(8.4%) |
5(2.8%) |
47(6.9%) |
| Total |
502(100%) |
178(100%) |
680(100%) |
P=0.003**, Significant, Chi-Square test
Table 4: Association of Age in years in relation to incidence of AKI.
Infections were the leading cause of AKI. Amongst infections dengue (30%) was the most common etiology
associated with AKI, followed by sepsis (21.9%) and then
pneumonia (17.9%) (Table 5).
| AKI etiology |
AKI cases |
| Number |
Percentage |
| Dengue |
54 |
30.0 |
| Pneumonia |
32 |
17.9 |
| Sepsis |
39 |
21.9 |
| Acute GE |
9 |
5.05 |
| HUS |
4 |
2.24 |
| ALS |
10 |
5.61 |
| Poisoning |
15 |
8.42 |
| Status epilepticus |
7 |
3.9 |
| Malignancy |
2 |
1.12 |
| Snake bite |
2 |
1.12 |
| Cardiac Failure |
4 |
2.24 |
Table 5: Etiology of AKI.
On univariate analysis, hypotension, nephrotoxic drugs,
sepsis, need for mechanical ventilation were significant
risk factors for AKI. 56.9% of patients with AKI were
boys. (p=0.818). There was no significant difference of
AKI between males and females Hypotension was found
in 75.3% of patients with AKI (p<0.001). Nephrotoxic
drugs were associated with 42.1% of AKI cases (p<0.001).
Sepsis was present in 21.9% of AKI cases (p<0.001).
Need for mechanical ventilation was there in 20.2% cases
(p<0.001) (Table 6).
| Variables |
Final Rifle stage |
Total (n=680) |
P value |
| No AKI (n=502) |
AKI (n=178) |
| Gender |
|
|
• Male
|
287(57.2%) |
100(56.2%) |
387(56.9%) |
0.818 |
|
• Female
|
215(42.8%) |
78(43.8%) |
293(43.1%) |
| Hypotension |
|
|
• Yes
|
154(30.7%) |
134(75.3%) |
288(42.4%) |
<0.001 |
|
• No
|
348(69.3%) |
44(24.7%) |
392(57.6%) |
| Nephrotoxic drugs |
|
|
• Yes
|
291(58%) |
75(42.1%) |
366(53.8%) |
<0.001 |
|
• No
|
211(42%) |
103(57.9%) |
314(46.2%) |
| Sepsis |
|
|
• Yes
|
52(10.4%) |
39(21.9%) |
91(13.4%) |
<0.001 |
|
• No
|
450(89.6%) |
139(78.1%) |
589(86.6%) |
| Ventilator |
|
|
• Yes
|
34(6.8%) |
36(20.2%) |
70(10.3%) |
<0.001 |
|
• No
|
468(93.2%) |
142(79.8%) |
610(89.7%) |
Table 6: Correlation of clinical variables in relation to incidence of AKI.
In this study, of all the AKI cases 68% were due to Prerenal
cause and 32% was renal cause (Table 7).
| Cause of AKI |
No. of patients |
% |
| Pre Renal |
121 |
68.0 |
| Renal |
57 |
32.0 |
| Total |
178 |
100.0 |
Table 7: Cause of AKI in relation to incidence of AKI in patients studied.
A Backward Wald logistic regression was performed to
ascertain the effects of hypotension, Sepsis, Ventilation and
nephrotoxic drugs usage on the likelihood that participants
have acute kidney injury. The logistic regression model
was statistically significant P<0.001 drawing an inference
that each of these risk factors were individually associated
with occurrence of AKI (Table 8).
| Variables |
Logistic regression results to predict the development of AKI |
95%CI |
| Logit co-efficient |
SE |
Wald |
P value |
Adj OR |
Lower |
Upper |
| Hypotension |
1.78 |
0.21 |
70.95 |
<0.001 |
5.95 |
3.93 |
9.01 |
| Nephrotoxic drugs |
-0.79 |
0.20 |
15.28 |
<0.001 |
0.45 |
0.31 |
0.67 |
| Sepsis |
0.91 |
0.27 |
11.81 |
0.001 |
2.50 |
1.48 |
4.20 |
| ventilation |
0.62 |
0.29 |
4.51 |
0.034 |
1.85 |
1.05 |
3.28 |
Table 8: Multivariate Logistic regression analysis to assess the risk factors for development of AKI
Discussion
In the present study, the incidence of AKI in PICU was
26.1%. This was comparable to Krishnamurthy et al
where incidence was 25.1% [13]. It was high compared
to other studies conducted in developed countries such
as Schneider et al where incidence was 10% which used
only serum creatinine to define AKI and not change in
eCCl [14]. However it was lower than reported figure of
82% according to Akan-Arican et al, in which all patients
had respiratory failure and were in receipt of mechanical ventilation [15]. This difference can be explained by
heterogeneity of patient population, regional differences
and sample size can explain this difference.
AKI stratum R, I, F was diagnosed in 60.7%, 28.6% and
10.7% OF AKI cases. The results are comparable to Mehta
et al. Maximum number of AKI patients were in Stratum
R. Altogether there was progression in grades in 76 cases,
maximum progression was from 'No AKI' to stage R.
Amongst the three pRIFLE stages maximum progression
was seen in stage R to stage I. This was similar to results
of both Hoste et al and Hui et al which also showed
maximum progression to stage I from stage R [16,17] Pediatric RIFLE criteria use both eCrCl and urine output
criteria for classification of AKI stages. In this study urine
output criteria was applied only to those patients who were
catherized for accurate measurement of urine output. Of
the cases for whom urine output criteria was applied there
was matching in 77% between urine output and eCrCl
criteria. Akcan-Arikan et al and Krishnamurthy et al
observed matching of 35% and 37% between urine output
and serum creatinine criteria comparable to the present
study [13,15]. It was observed that there is an increasing
trend in matching between the urine output and eCrCl with
progression of stage.
The maximum number, 28% of AKI patients were below
1 year in our study which was comparable to Mehta et
al. This shows that patients with AKI were younger than
those without AKI.
The etiology of AKI varies from developed and
developing countries. While sepsis, glomerulonephritis,
HUS and ATN predominate in developing countries,
these are replaced by major surgery, haemato-oncological
complications, nephrotoxic drugs and pulmonary failure
as cause of AKI. In this study too infections contributed to
majority of AKI cases. Amongst infections dengue (30%)
was the most common etiology associated with AKI,
followed by sepsis (21.9%) and then pneumonia (17.9%).
Tropical febrile illnesses have been associated with AKI.
Dengue is a tropical febrile illness that is common in
this part of country. Dengue constituted the majority of
cases. The next common etiology was sepsis. According
to both Krishnamurthy et al and Mehta et al sepsis was
the most common etiology associated with AKI. There
is geographical variation in the etiology. There were no
post renal etiologies detected in this study. This could be
probably attributed to the post renal causes run a chronic
course with progressive deterioration of renal function and also that their detection is more frequent in pediatrics
wards than in PICU.
Prerenal causes account for majority of the AKI (68%) as
renal diseases were excluded from the study. In our study
risk factors for AKI were hypotension, nephrotoxic drugs,
sepsis and Need for Ventilation. Hypotension was found
in 75.3% of patients with AKI (p<0.001). Nephrotoxic
drugs were associated with 42.1% of AKI cases (p<0.001).
Sepsis was present in 21.9% of AKI cases (p<0.001).
Need for mechanical ventilation was there in 20.2%
cases (p<0.001). This is comparable with Mehta et al and
Mendonca et al [18].
The potential limitation of this study is the use of an
assumed baseline eCrCl. Furthermore urine output criteria
could not be applied to all patients as only patients who
were catheterized were included for urine output criteria.
Conclusion
AKI incidence in high in children admitted to PICU.
AKI commonly associated with severe dengue, sepsis
and pneumonia. It is amenable to treatment provided
early diagnosis and prompt treatment. Early identification
requires uniform definition and staging system to guide
intervention. This study supports use of the pRIFLE score
as an easy and simple tool for identification and classifying
AKI.
References
- Ravindra Mehta, J Cerda. International Society of Nephrology’s 0by25 Initative for acute kidney injury: a human rights case for nephrology. The Lancet 2015.
- PaweenaSusantitaphong, Dinna N. Cruz, Cerda J, Maher Abulfaraj, Fahad A, et al.,, For the Acute Kidney Injury Advisory Group of the American Society of Nephrology. ‘World Incidence of AKI: A Meta-Analysis. ‘Clin J Am SocNephrol 2013; 8: 1482-1493.
- Andreoli SP. Acute kidney injury in children, PediatrNephrol. 2009;24:253-263.
- Askenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL. 3-5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int. 2006;69:184-189.
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure: Definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204-12.
- Lameire N, Van Biesen W, Vanholder R. The changing epidemiology of acute renal failure. Nat Clin PractNephrol 2; 2006:364-377.
- Cerdá J, Bagga A, Kher V, Chakravarthi RM. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat Clin PractNephrol. 2008;4:138-153.
- Cerda J, Lameire N, Pannu N, Uchino S, Wang H, et al. Epidemiology of acute kidney inury. Clin J AM SocNephrol. 2008;3:881-886
- Mehta P, Sinha A, Sami A, Hari P. Incidence of Acute Kidney Injury in Hospitalized Children.
- Bowers LS, Wong ET. Kinetic serum creatinine assay II. A critical analysis and review. Clin Chem. 1980;26:555-561.
- Goldstein B, Giroir B, Randolph A.International Pediatric Sepsis Consensus Conference: Definitions for sepsis and organ dysfunction in Pediatrics. PediatrCrit Care Med. 2005;6:2-8.
- Basu RK, Prasad DP, Wong H, Wheeler DS. An update and review of acute kidney injury in pediatrics. PediatrCrit Care Med. 2011;12:339-347.
- Krishnamurthy S, Mondal N, Narayanan P, Biswal N, Srinivasan S, et al., Incidence and etiology of acute kidney injury in southern india. Indian J Pediatr. 2013;80:183-189.
- Schneider J, Khemani R, Grushkin C et al., Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med 2010; 38:933-939.
- Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, et al., Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71:1028-1035.
- Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, et al., RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: A cohort analysis. Crit Care. 2006;10:R73-82.
- WF Hui, Chan W, Miu TY et al. acute kidney injury in the pediatric intensive care unit: identification by modified RIFLE criteria. Hong Kong Med J.2013; 19:13-19.
- De Mendonça, Arnaldo, et al. "Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score." Intensive care medicine 2000;915-921.