Research Article - Biomedical Research (2017) Volume 28, Issue 21
In vitro study on ultrasound-targeted and micro-bubble destruction-mediated ginsenoside rg1 in treating glaucomatous optic nerve damage
Yusheng Ma1#, Fengwei Ma1#, Guofeng Li2*1Department of Ophthalmology, Weifang Yidu Central Hospital, Weifang, Shandong, China
2Department of Ophthalmology, Weifang People’s Hospital, Weifang, Shandong, China
#These authors contributed equally to this work
Accepted date: November 03, 2017
Abstract
Objective: To investigate the therapeutic effect of ultrasound-targeted and micro-bubble destructionmediated ginsenoside Rg1 on glaucomatous optic nerve damage in rats.
Methods: 30 SD rats were selected as the study objects and randomly divided into the normal control group (n=10), the model group (n=10) and the treatment group (n=10). The model rats with glaucomatous optic nerve damage were treated with ultrasound-targeted and micro-bubble destructionmediated ginsenoside Rg1. The level of apoptotic genes (C-fos, p53, Smac), cytokines (BDNF, NRG-1, SDF-1), aquaporins and ion channels (AQP-1, CIC-3, CR) in the retina of each group was measured and compared.
Results: The contents of C-fos, p53 and Smac mRNA in the model group were obviously higher than those in the normal control group (p<0.05); The contents of BDNF, NRG-1 in the model group were significantly lower than those in the normal control group, while the level of SDF-1 was higher than that of control group. The levels of BDNF and NRG-1 in the treatment group were higher than those in model group, whereas the level of SDF-1 was greatly lower than that in the model group. When it comes to the model group, its AQP-1 was evidently lower than that of the normal control group, while its levels of CIC-3 and CR were higher than those in the normal control group. The AQP-1 mRNA level in the treatment group was obviously higher than that in the model group and the CIC-3 and CR mRNA contents were lower than those in the model group.
Conclusion: Ultrasound-targeted and micro-bubble destruction-mediated ginsenoside Rg1 can inhibit the apoptosis of retinal ganglion cells and the expression of such aquaporins and ion channels as AQP-1, CIC-3 and CB. Therefore, it is effective in treating glaucomatous optic nerve damage in rats.
Keywords
Ultrasound, Ginsenoside Rg1, Glaucoma, Optic nerve damage.
Introduction
Glaucoma, a kind of eye disease with relatively high incidence, is easy to induce the apoptosis of retinal ganglion cells under the condition of durative high intraocular pressure, which then causes optic nerve damage disease [1]. As such, the inhibition of retinal ganglion cell apoptosis and the effective protection of the function of retinal ganglion cell are the ideal target for the treatment of glaucomatous optic nerve damage [2]. In recent years, many drugs and treatment methods have been applied to the clinical treatment of ophthalmic diseases, but the outcomes brought by different options are not the same [3,4]. Ultrasound-targeted and micro-bubble destruction-mediated ginsenoside Rg1, a new treatment approach carried out in our hospital, has achieved satisfactory clinical results. However, there are few research reports about the mechanism of ultrasound-targeted and micro-bubble destruction-mediated ginsenoside. The aim of this study is to make an animal experimental study on glaucomatous optic nerve damage in rats and to explore the mechanism of ultrasound-targeted and micro-bubble destruction-mediated ginsenoside Rg1 on glaucomatous optic nerve damage in rats to provide theoretical reference for the better application of such therapy.
Materials and Methods
Materials
30 SD rats, weighing about 182-206 g and provided by the laboratory animal center of our hospital, were selected. Other materials included: ginsenoside Rg1 (Chengdu Desite Bio-tech Co., Ltd), % chloral hydrate (Nanjing Xinfan Bio-tech Co., Ltd), paraformaldehyde (Shanghai Gefan Bio-tech Co., Ltd), phosphate buffer ( Beijing Solarbio Technologies Co., Ltd ), htoxylin eosin (Shanghai Bogoo Biotechnology Co., Ltd.), xylene (Nanchang Ocean And Chemical Co., Ltd.), Trizol lysate (Shanghai Gefan Bio-tech Co., Ltd), PCR instrument (Xi'an Tianlong Technologies Co., Ltd.), and optical microscope (Shanghai Optical Factory).
Experimental grouping
In this study, the normal control group (n=10), the model group (n=10) and the treatment group (n=10) were established. The model rats with glaucomatous optic nerve damage were established as follows: according to the references [5], the rats were anesthetized by the injection of 5% chloral hydrate in the celiac and fixed on the operating table. The left eye was selected as the experimental object. Then surgery was performed to remove the lacrimal gland, kept the lateral rectus apart and exposed the optic nerve. Afterwards, the noninvasive vascular tweezers were used to clamp the eye for optic nerve damage. The rats that showed the symptoms of ischaemia and infection after the injury were washed out. On the second day after surgery, this eye was observed. If the pupil has been expanded and had no light reflex and the eyeball was not prominent obviously, then the model was established.
Therapeutic methods
Rats in the treatment group were treated with ultrasoundtargeted and micro-bubble destruction-mediated ginsenoside Rg1: these rats were treated with ultrasound-guided drugcarrying micro-bubbles rupture by preparing ginsenoside Rg1 micro-bubbles. They were treated one time per day for seven days before conducting experiment. Rats in the model group were treated by injecting 0.05 ml saline one time per day for seven days before conducting experiment.
Approach of specimen collection
All rats in the normal control group, the model group and the treatment group were killed. The eyeballs taken out were immediately placed on ice and the retinal tissues extracted were preserved at -80°C liquid nitrogen until ready for use.
HE section staining method
The retinal of rats in the normal control group and the model group was prepared into frozen slices with the thickness of 6 μm and stained by htoxylin eosin to analyse whether the model was successful established or not. The method was described as follows: the slices were put into para-formaldehyde solution for 20 min and cleaned by phosphate buffer for three times, each lasting about 5 min. And then they were dried in normal temperature. Subsequently, 3 slices randomly selected for each specimen were dealt with as follows: the slices were soaked in distilled water for about 5 min; and then they were soaked in hematoxylin for 5 min so as to dye the cell nucleus and rinsed with running water; next, 1% HCl-Ethanol was used to separate color, which continued 30 s and 1% ammonia ethanol to bring back blue, lasting 10 s; again, they were soaked in distilled water for 2 min before being put into 1% eosin stain for 90 s and rinsed by flowing water; after that, they were dehydrated by using graded ethanol for about 10 min, hyalinized by methyl-benzene for some 15 min and mounted. At last, they were observed under optical microscope.
Methods for index detection
Put the specimen of retinal tissue into Trizol lysate, grind it and extract RNA. Then the apoptosis genes like C-fos, p-53 and Smac, such cytokines as BDNF, NRG-1 and SDF-1 and the water and ion channels, including AQP-1, CIC-3 and CR were amplified by PCR reaction. The relative expression of target gene was calculated by the following formula: ΔCt=Ct target gene-Ct β-actin, among which ΔCt was inversely proportional to the relative expression of target gene.
Statistical analysis
The data were analysed and calculated by SPSS 20.0. The comparison of measurement data between the three groups were examined by single factor variance and the comparison between two groups was tested by t-test. P<0.05 suggests that the difference is statistically significant.
Results
The result of HE staining
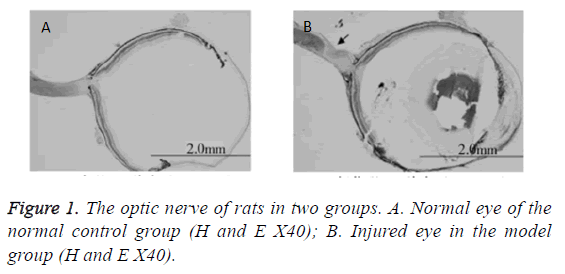
According to the analysis of H and E staining, compared with the rats in the normal control group, the optic nerve of rats in the model group was obviously damaged. Tissues in the damage area were palely stained and nerve fibers disorderly arranged (Figure 1). It suggested that the model was successfully established.
Comparison of the expression of apoptosis genes between the three groups
The contents of C-fos, p53 and Smac mRNA in the model group were obviously higher than those in the normal control group. The levels of C-fos, p53 and Smac mRNA in the treatment group were lower than those in the model group (Table 1).
| Groups | n | c-fos | p53 | Smac |
|---|---|---|---|---|
| The normal control group | 10 | 100.00 ± 12.48 | 100.00 ± 13.56 | 100.00 ± 14.77 |
| The model group | 10 | 303.56 ± 37.91 | 262.55 ± 48.15 | 288.44 ± 23.51 |
| The treatment group | 10 | 175.24 ± 17.82 | 154.76 ± 19.02 | 164.16 ± 15.63 |
| F | 12.09 | 10.36 | 14.11 | |
| p | 0.025 | 0.017 | 0.033 |
Table 1: Comparison of the content of mRNA in apoptosis genes among all groups.
Comparison of the expression of cytokines between the three groups
The contents of BDNF, NRG-1 and mRNA in the model group were significantly lower than those in the normal control group, while its level of SDF-1 mRNA was higher than that of the normal control group. The contents of BDNF and NRG-1 mRNA in the treatment group were higher than those in the model group, whereas its level of SDF-1 mRNA was greatly lower than that in the model group (Table 2).
| Groups | n | BDNF | NRG-1 | SDF-1 |
|---|---|---|---|---|
| The normal control group | 10 | 100.00 ± 17.25 | 100.00 ± 14.06 | 100.00 ± 16.08 |
| The model group | 10 | 24.46 ± 5.42 | 29.04 ± 2.63 | 312.56 ± 37.68 |
| The treatment group | 10 | 73.21 ± 10.15 | 54.32 ± 6.75 | 158.33 ± 19.05 |
| F | 15.77 | 16.28 | 19.21 | |
| p | 0.021 | 0.019 | 0.011 |
Table 2: Comparison of the content of mRNA in cytokines among all groups.
Comparison of the expression of the water and ion channels between the three groups
The content of AQP-1 mRNA in the model group was evidently lower than that of the normal control group (p<0.05), while its levels of CIC-3 and CR mRNA were higher than those in the normal control group (p<0.05); the AQP-1 mRNA level in the treatment group was obviously higher than that in the model group (p<0.05) and the CIC-3 and CR mRNA contents were lower than those in the model group (Table 3).
| Groups | n | AQP-1 | CIC-3 | CR |
|---|---|---|---|---|
| The normal control group | 10 | 100.00 ± 13.05 | 100.00 ± 18.23 | 100.00 ± 17.02 |
| The model group | 10 | 32.78 ± 3.26 | 238.96 ± 31.22 | 305.31 ± 41.28 |
| The treatment group | 10 | 67.83 ± 7.63 | 176.85 ± 17.83 | 198.72 ± 19.41 |
| F | 18.07 | 17.13 | 18.52 | |
| p | 0.037 | 0.026 | 0.022 |
Table 3: Comparison of the content of mRNA in the water and ion channels among all groups.
Discussion
The occurrence of glaucoma is of great harm as it can easily induce vision loss and lead to optic nerve damage as well as to durative high intraocular pressure, so it has been paid more attention in recent years. Ultrasound-targeted micro-bubble destruction technology is a treatment technique that has emerged in recent years. It is worked by transmitting acoustic with different sound intensity site, which causes the rapture of micro-bubble under ultrasonic waves; meanwhile, the cavitation effect triggered by ultrasound has biological effect on the tissues around specific sites, improving vascular permeability that allows exogenous materials to better get through vascular endothelial barrier to reach the lesions quickly [6,7]. Ginsenoside Rg1 is one of the main effective components of ginsenoside [8]. Research shows that [9,10], ginsenoside Rg1 can enhance learning memory, improve immunity and defer organism aging. Scholars like Li [11], have found in trials that ginsenoside Rg1 can, to some extent, inhibit the apoptosis of nerve cells.
In this article, we established the rat model with glaucomatous optic nerve damage, which were treated with ultrasoundtargeted and micro-bubble destruction-mediated ginsenoside Rg1. Studies have confirmed that [12], hypertensive eye incurred by glaucoma can contribute to the excessive expression of many apoptotic factors in human body, which causes the apoptosis of retinal ganglion cells, damaging the optic nerve.
The increased expression of various pro-apoptotic genes like C-fos, p53 and Smac is involved in the apoptosis of retinal ganglion cells [13-15]. Under normal conditions, C-fos, p53 and Smac in body’s nervous system are in low-level expression; but when oppressed with ocular hypertension, C-fos, p53 and Smac will express excessively, promoting cell apoptosis. This study demonstrated that the contents of C-fos, p53 and Smac mRNA in the model group were obviously higher than those in the normal control group and that the levels of C-fos, p53 and Smac mRNA in the treatment group were lower than those in the model group. This means that ultrasound-targeted and micro-bubble destruction-mediated ginsenoside Rg1 can inhibit the apoptosis of retinal ganglion cells.
The apoptosis process of retinal ganglion cells is complex because many mechanisms are involved in it and it is closely related to the abnormal expression of various kinds of nerverelated cytokines. Neurotrophin BDNF and neuroprotective protein NRG-1 are of remarkable significance in maintaining the survival and function of neuron. If these cytokines are deprived, patients with glaucoma are prone to suffer from nerve injury. SDF-1, a kind of important cytokine in glial cells, can facilitate the appearance of glial scar. According to this study, the contents of BDNF, NRG-1 and mRNA in the model group were significantly lower than those in the normal control group, while its level of SDF-1 mRNA was higher than that of the normal control group. The contents of BDNF and NRG-1 mRNA in the treatment group were higher than those in the model group, whereas its level of SDF-1 mRNA was greatly lower than that in the model group. All these suggest that ultrasound-targeted and micro-bubble destruction-mediated ginsenoside Rg1 is conducive to regulating the expression of such cytokines as BDNF, NRG-1 and SDF-1 and to the repair and regeneration of retinal ganglion cells.
Water channel and ion channel are involved in adjusting body’s intraocular pressure. The unusual expression of water channel and ion channel can raise the level of eye pressure, causing damage to retinal ganglion cells. AQP-1 is a kind of important aquaporin that plays crucial role in balancing intracellular and extracellular moisture. CIC-3 is an important component of chloride channel and CR is involved in regulating calcium ion and magnesium ion. CIC-3 and CR play a key role in adjusting cell volume and maintaining the balance of charge inside and outside vesicle. This study demonstrated that the content of AQP-1 mRNA in the model group was evidently lower than that of the normal control group, while its levels of CIC-3 and CR mRNA were higher than those in the normal control group; and that the AQP-1 mRNA level in the treatment group was obviously higher than that in the model group and the CIC-3 and CR mRNA contents were lower than those in the model group. This hints that ultrasound-targeted and micro-bubble destruction-mediated ginsenoside Rg1 can regulate the expression of water channel and ion channel in retina, making body’s eye pressure remain at a normal level.
Conclusion
In conclusion, ultrasound-targeted and micro-bubble destruction-mediated ginsenoside Rg1 can inhibit the apoptosis of retinal ganglion cells and regulate the production of such cytokines as BDNF, NRG-1 and SDF-1 and the expression of water and ion channels like AQP-1, CIC-3 and CB. Therefore, it is effective in treating rats with glaucomatous optic nerve injury.
References
- Ke F, Yu J, Tan K. Study on the protective effect of ligustrazine on retinal ganglion cells of rats with chronic ocular hypertension. Mod J Integr Trad Chinese West Med 2017; 26: 935-938.
- Shao Y, Yu Y, Zhou Q. Inhibition of miR-134 protects against hydrogen peroxide-induced apoptosis in retinal ganglion cells. J Mol Neurosci 2015; 56: 461-471.
- Silva GRD, Fialho SL, Siqueira RC. Implants as drug delivery devices for the treatment of eye diseases. Braz J Pharm Sci 2010; 46: 585-595.
- Rakoczy PE, Shen W, Lai M. Development of gene therapy‐based strategies for the treatment of eye diseases. Drug Develop Res 2015; 46: 277-285.
- Elsaied HE, Hamdy MD, Elsherbini AI. Investigation of proniosomes gel as a promising carrier for transdermal delivery of glimepiride. Univ J Pharm Res 2016; 1: 1-5.
- Wang S, Li Y. The progress in ultrasound-mediated and microbubble-targeted therapy. Med Philos 2017; 38: 57-60.
- Suzuki R, Oda Y, Utoguchi N. Progress in the development of ultrasound-mediated gene delivery systems utilizing nano- and microbubbles. J Off J Control Rel Soc 2011; 149: 36-41.
- Xu YL, Gao YZ, Tan KB. Myocardium-targeted transplantation of mesenchymal stem cells by diagnostic ultrasound-mediated microbubble destruction improves cardiac function in myocardial infarction of New Zealand rabbits. Int J Cardiol 2010; 138: 182-195.
- Lin Y, Lin Y, Yu G. The regulatory effect of ginsenoside Rg1 on the expression and signal transduction pathways in titanium particles co-cultured into osteocyte integrin. Chinese J Trad Med Traumatol Orthop 2017; 16: 3005-3007.
- Peng C, Li J, Tian X. Myocardium fibrosis of ginsenoside Rg1 after the inhibition of the acute myocardial infarction of rats. Prog Mod Biomed 2017; 16: 3005-3007.
- Li J, zhang X. Study on the mechanism of ginsenoside Rg1 on inhibiting neuron apoptosis. Acta Pharmaceutica Sinica 1997; 406-410.
- Anshu A, Price MO, Richardson MR. Alterations in the aqueous humor proteome in patients with a glaucoma shunt device. Mol Vis 2011; 17: 1891-1900.
- Lo PK, Huang SZ, Chen HC. The prosurvival activity of p53 protects cells from UV-induced apoptosis by inhibiting c-Jun NH2-terminal kinase activity and mitochondrial death signaling. Cancer Res 2004; 64: 8736-8745.
- Hsiao WT, Tsai MD, Jow GM. Involvement of Smac, p53, and caspase pathways in induction of apoptosis by gossypol in human retinoblastoma cells. Mol Vis 2012; 18: 2033-2042.
- Tan W, Zhao C, Li G. Study on the protection mechanism of brain-derived neurothrophic factor on neuron cultured in non-serum. Shanghai Med J 2011; 34: 375-378.