- Biomedical Research (2014) Volume 25, Issue 1
Impact of ?Workshop? on the performances of first professional medical students in Physiology.
A. Bansal and S. Aggarwal*Department of Physiology, Rama Medical College, Hospital and Research Centre, Ramadelhi, NH-24, Ghaziabad (U.P.) –245304, India
Accepted date: November 21 2013
Citation: A. Bansal and S. Aggarwal. Impact of “Workshop” on the performances of first professional medical students in Physiology. Biomedical Research 2014; 25 (1): 127-131.
Abstract
Introducing interactive techniques of teaching in medical education can promote learner participation and, as a result, can lead to a higher level of learning. This article assesses the effectiveness of interactive learning technique. The present study was conducted on 300 first professional medical students of two consecutive batches, each of 150 students, with an aim to evaluate the impact of “Workshop” on their performances in Physiology. Students of both the batches were divided into three groups of 50 students each. All the groups were exposed to a workshop of two hours held once a week for ten weeks under the guidance of a facilitator. Their performance in Physiology was then assessed by subsequently held pre-professional theory examination. To evaluate the impact of workshop, their individual performances in terms of marks obtained as well as performance of the batch in terms of number of students passed in pre-professional examination were compared with that in the semester examination, held before conduction of the workshops. Outcome analysis of both the batches revealed that not only the performance of the batch but also the individual performances of the students were significantly higher in pre-professional examination than that in semester examination. This revealed the positive impact of workshop on the acquisition of knowledge by the students, their retention of the topic and their motivation towards self-directed learning.This study may help facilitators encourage more of student-centered learning activities in their curriculum to fulfill the goals of outcome based education focused towards students becoming lifelong learners.
Keywords
Interactive learning technique, Workshop Performance, Student-centered learning
Introduction
The quality of an educational system can be judged from at least three perspectives: the inputs to the system, what happens within the system and the outputs from the system. Those who are interested in inputs will focus their attention primarily on finances, resources, infrastructure, etc. Those interested in what happens within the system will focus their attention primarily on the processes used to organize, control and deliver education and training. Those interested in outcomes will focus their attention primarily on the products or results of education [1].
Medical education is a lifelong process embracing pre-medical experience, undergraduate education, general clinical training, specialist or vocational training, subspecialty training, and continuing medical education [2]. Medical schools need to prepare young doctors to practice in an increasingly complex healthcare scene with changing patient and public expectations, and increasing demands from employing authorities [3]. Educators across the world are charged with the responsibility of producing core learning outcomes for their medical curricula. These learning outcomes are often defined as the knowledge; skills and attitudes required by medical students at graduation [4].
In an attempt to recapture the education mission, one of the most important trends in health profession education in recent years has been the move to outcome based education. The emphasis is on the product-what sort of doctor will be produced-rather than on the educational process [5]. The core recommendation of the General Medical Council's education committee is the promotion of learner-centered and problem-oriented approaches to learning, which aim to produce doctors better equipped with the adult learning skills necessary for them to adapt to, and meet, the changing needs of the community they serve. The pedagogic shift from the traditional teachercentered approach, in which the emphasis is on teachers and what they teach, to a student- centered approach, in which the emphasis is on students and what they learn, requires a fundamental change in the role of the educator from that of a didactic teacher to that of a facilitator of learning. In reviewing and revising their undergraduate curriculums, many medical schools with large class sizes have chosen to introduce revised teaching and learning strategies that are more learner-centered but which attempt to combine the best of traditional modes with more innovative methods [2]. Thus, the primary emphasis of OBE in medical education lies on the importance of the process of learning and its outcome.
In the face of the above context, the Department of Physiology of Rama Medical College, Hospital and Research Centre planned to introduce an interactive learning technique, Workshop along with the conventional lecture method into their first year Physiology curriculum and evaluate its impact on the performances of first professional medical students in Physiology over a period of two years. The objective was to encourage the students for active participation in their own learning, facilitate them in the understanding of the curriculum and the learning outcomes, and motivate them towards self-directed and deep learning.
Material and Method
The present study was conducted in the Department of Physiology on 300 first professional medical students of two consecutive batches, 2011-12 and 2012-13 admitted at Rama Medical College, Hospital and Research Centre, Ghaziabad (U.P.).
The theory classes of Physiology of both the batches were held through out the academic session of one year by adopting single human body system teaching approach at one time to ensure better understanding of the subject matter. Each system was taught by only one faculty member by conventional lecture method to prevent bias. After completion of each human body system, a theoretical system completion test was conducted to assess the students. A semester examination was also conducted after the completion of the first semester. Then, two months prior to the pre-university examinations scheduled at the end of second semester, students of both the batches were exposed to the same type of curricula innovative tool.
Students of both the batches were divided into three groups of 50 students each, according to their enrollment numbers on the attendance register. Each group was allotted one faculty member who was its facilitator. Division and allotment of batches was randomly done to prevent bias.
The groups were further divided into ten subgroups of five students each, according to their enrollment numbers. Cumulative internal assessment of performances of the students of each subgroup in the system completion tests and terminal theory examination was prepared. The internal assessment was evaluated and amongst the students of each subgroup, students who failed to fulfill 33% internal assessment university eligibility criterion for appearing in university examinations, were identified. These students constituted the representatives of their subgroups.
A set of question papers from previous years’ university examinations was prepared and distributed amongst the students. Each subgroup was allotted two assignments in the form of two question papers from the entire set. The representatives of each subgroup were asked to find answers to the allotted assignment as well as discuss it with other members of their subgroup.
A workshop of two hours was then held once a week for ten weeks for all the groups of a batch under the guidance of each facilitator. All the students had been informed to bring their Physiology textbooks with them in the workshop. In each workshop, the representatives of two subgroups informed before were asked to present one of their assignments. The representatives not only presented their assignment but also helped other students of their group locate and mark the answers of question papers in their textbooks. The facilitator helped the representatives in their presentation. They also guided the students on the skills of framing and writing an answer. To encourage students for their effective participation in the workshop, students were given credits in the form of attendance. Credit of two marks to each member of subgroup was also given for each assignment attended or represented. The entire set was thus discussed in twenty workshops. The students of both the batches were then assessed by subsequently held theory pre-professional examination.
To evaluate the impact of Workshop, the performance of the students of both the batches in terms of number of students passed (obtaining 50% marks in theory was taken as the cut-off percentage for passing) as well as the individual performances of the students in terms of marks obtained in Physiology theory pre-professional examination held after conduction of the workshops were compared with that of the semester examination held before.
To compare the results, statistical analysis was done by applying students’ paired t- test and McNemar test with continuity correction. The level of significance was considered only when the p value is less than 0.05 (p < 0.05).
Results
Statistical analysis of the data revealed that the cumulative performance of the students in terms of the number of students passed as well as the individual performances of the students in terms of marks obtained in Physiology were higher in the pre-university examination than that in the terminal examination.
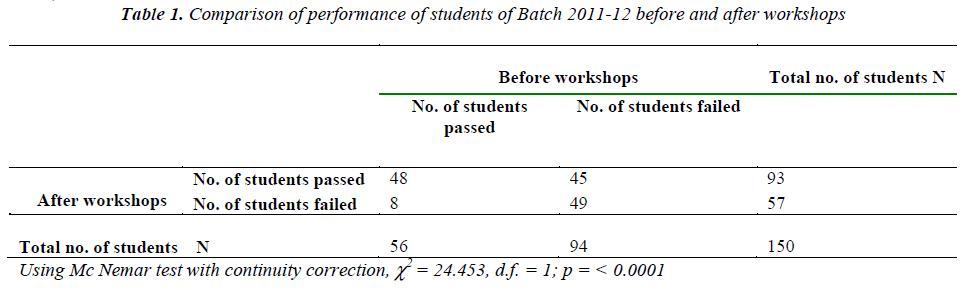
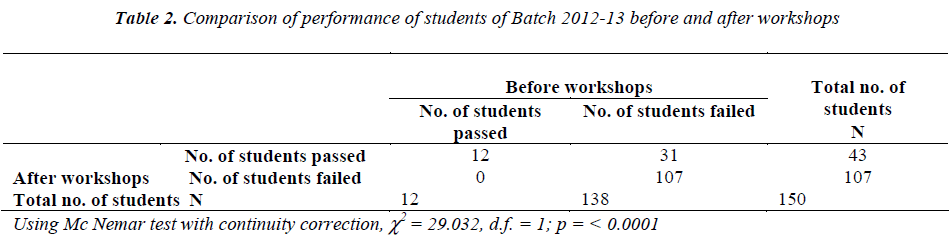
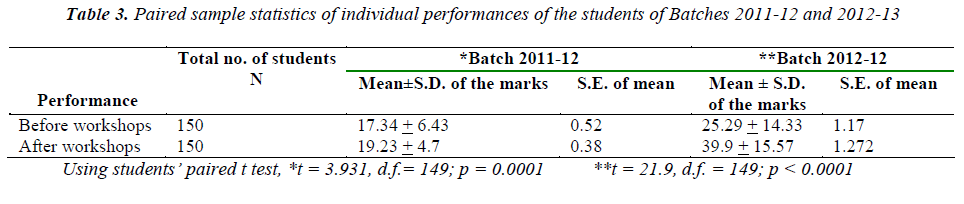
For the batches 2011-12 and 2012-13, only 37% and 8% students had passed in the terminal exam whereas in the pre-university exam, this pass percentage had risen to 62% and 28.6% respectively. Mc Nemar test with continuity correction was applied to calculate the significance of this difference and it was found to be highly significant for both the batches (p<0.0001).
The individual performances of each student of both the batches in both the examinations were also compared using students’ paired t-test. Students of both the batches performed considerably better in the pre-university examination held after conduction of the workshops compared to the semester examination held before and the difference in their pre and post workshops’ performances was highly significant (p< 0.0001).
Discussion
Medical curricula can be delivered in many ways. The lecture still remains the most widely used method of teaching in medical education. Although effective lecturing has been described in the literature, many question whether problem-solving skills or attitudes can be transmitted using the traditional lecture. Introducing interactive techniques can promote learner participation and, as a result, can lead to a higher level of learning [6]. In recent times, traditional teaching methods characterized by lectures and large groups demonstrations are quickly being replaced by modern innovative teaching/ learning methods. The main emphasis of the innovative teaching method is to place the student at the centre of teaching/learning process and to place the burden and responsibility for learning on the learner [7]. The other major emphasis is to avoid rote-learning and to develop problem-solving and life-long learning skills in the learner that is teaching the student how to learn.
The educational research has shown that students who are actively involved in the learning activity will learn more than students who are passive recipients of knowledge [8,9]. Interactive learning techniques can promote active involvement of the students with the material or the content, with the teacher, or with classmates/peers [10]. Indeed, even students who do not talk in class are often stimulated by questions or problem solving exercises as they think about what they would answer in a particular situation. Studies by Canon R and Michaelsen et al have revealed that interactive methods promote critical thinking and appear to be a superior method of attaining higher-level intellectual learning [7,11].
Rao and DiCarlo in their study on active learning of respiratory physiology have demonstrated that interactions allow two-way communication, reduce the monotony of passive learning, and enhance the students’ level of understanding and their ability to synthesize and integrate material [12]. Furthermore, such type of teaching interrupted by discussion increases the attention and memory of the students [10,13]. It also encourages the students to ask queries and think beyond the box thus keeping both students and teachers awake and learning alive [14]. It also allows teachers to receive instant feedback at a number of levels: on student needs (at the beginning, middle or end of a lecture), on how the information has been assimilated, and on future learning directions. Students, on the other hand, can get feedback on their own knowledge or performance [10].
It has been recognized that increased student involvement leads to change in attitude and learning outcomes [15]. Better learning outcomes and increase in student satisfaction with increased interactivity have been demonstrated by studies of Rees, McJimm [16,17]. Interactive lecturing is thus a way to capitalize on the strengths of small group learning in a large group format [8].
However still, till the present times, conventional lectures remain the primary tool for teaching and learning in most Indian medical colleges. Interactive sessions in the form of tutorials, seminars or workshops are often avoided in Indian medical colleges because of time constraints and fear of losing control over students. Other reasons for not adopting them in the medical curriculum include anxiety about not knowing the answer to a question posed by the students and large student to teacher ratio [10].
The present study had adopted one of the interactive learning tools, Workshop in its first professional Physiology curriculum despite the time constraints and large student to teacher ratio indicating that activelearning strategies can be easily incorporated into large classrooms. Outcome analysis of the study clearly revealed that the acquisition of knowledge by the students and their retention of the topic greatly improved after conduction of the workshops, so their performance in theory pre-university examination significantly improved by this method.
The workshops were able to arouse interest of the students in the subject and increase their receptivity, selfefficacy and motivation for self study. By organization of such workshops, learning became more active, interesting and self-directed. Students were encouraged to ask questions, communicate what they know and don’t know, challenge their assumptions, decide what information is needed to answer a question, determine how to frame an answer, think about how to apply what they had already learnt. This workshop on the one hand, helped the students clear their doubts, and on the other hand, provided the facilitators a feedback regarding poorly understood areas of the subject matter. It also helped in strengthening the communication skills of the students The representing students inspired their batch mates to interact and think creatively, increasing their self-efficacy which is linked to their academic performance.
It is also recognized that different learning systems suit different students so diversity in delivering medical curricula is supported. However, irrespective of the approach a significant amount of learning should be active. There must be sufficient time for self-directed learning and reflection to encourage students to develop the habits of lifelong learning [16]. Innovative education unlike the traditional education helps the student to develop skills and convert into independent learners [7].
At the end, it can be concluded that providing a variety of appropriate learning activities help students get the most from their medical education. Interactive learning techniques should be adopted in medical curricula to achieve the goals of outcome based education. The present study showed that student-centered learning activities like workshops motivate students to take responsibility for their own learning, improves their performance and help develop communication skills and attitudes such as teamwork and co-operation.
References
- Killen R. Outcomes-based education: Principles and possibilities. Unpublished manuscript. University of Newcastle, Australia, Faculty of Education 2000.
- Spencer JA, Jordan RK.. Learner centered approaches in medical education. BMJ 1999; 318 (7193):1280-1283
- Harden RM, Cosby JR, Davis MH. AMEE Guide No. 14: Outcome-based education: Part 1 – An introduction to outcome-based education. Medical Teacher 1999; 21(1): 7-14.
- Cannon R. Lecturing, Kensington (NSW). Higher Education Research and Development Society of Australia 1988.
- Davis M H. Outcome-based education. Journal of Veterinary Medical Education 2003; 30(3): 258-263.
- Nasmith L, Steinert Y. The evaluation of a workshop to promote interactive lecturing. Teach Learn Med. 2001; 13(1): 43-48.
- Nafukho FM, Kangethe S, Mutema AM. Innovative techniques in the training of health professionals: The case of Moi University, Faculty of Heath Sciences, Kenya. Presented at the Academy of Human Resource Development International Research Conference February 2000.
- Butler JA. Use of teaching methods within the lecture format. Medical Teacher 1992; 14: 11-25.
- Feden PD. About instruction: Powerful new strategies worth knowing. Educational Horizons 1994; 73:18-24.
- Steinert Y, Snell LS. Interactive lecturing: strategies for increasing participation in large group presentations. Medical Teacher 1999; 21(1): 37-42.10]
- Michaelsen LK, WatsonW, Cragin JP, Fink LD. Team learning: a potential solution to the problems of large classes. Exchange: The organizational behaviour teaching journal 1982; 7: 13- 21
- Rao SP, DiCarlo SE. Active learning of respiratory physiology improves performance on respiratory physiology examinations. Adv Physiol Educ 2001; 25: 55-61.
- Chilwant K.S. Comparison of two teaching methods, structured interactive lectures and conventional lectures. Biomedical Research 2012; 23 (3): 363-366.
- Mannison M, Patton W, Lemon G. Interactive teaching goes to university: keeping students awake and learning alive. Higher Education Research and Development 1994; 13: 35-47.
- Berg CA, Bergendahl VC, Lundberg BK. Benefiting from open-ended experiment? A comparison of attitudes to, and outcomes of, an expository versus an open-inquiry version of the same experiment. International Journal of Science Education 2003; 25(3): 351-372.
- Rees CE. The problem with outcomes‐based curricula in medical education: insights from educational theory. Medical education 2004; 38(6): 593-598.
- McKimm J. Current trends in undergraduate medical education: teaching, learning and assessment. Samoa Medical Journal 2010; 2 (2): 38-44.