Research Article - Current Pediatric Research (2022) Volume 26, Issue 3
Impact of the SARS-CoV-2 pandemic on pediatric trauma injuries requiring surgery in Germany.
Mine-Lea Meyer-Yeginer, Michael Boettcher, Konrad Reinshagen, Kristofer Wintges*
Department of Pediatric Surgery, University Medical Center Hamburg-Eppendorf, Martinistrae, Hamburg, Germany
- Corresponding Author:
- Kristofer Wintges
Department of Pediatric Surgery, University Medical Center Hamburg-Eppendorf, Martinistrae, Hamburg, Germany
E-mail: k.wintges@uke.de
Received: 03 February, 2022, Manuscript No: AAJCP-22-53366; Editor assigned: 07 February, 2022, PreQC No: AAJCP-22-53366 (PQ); Reviewed: 15 March, 2022, QC No: AAJCP-22-53366; Revised: 20 March, 2022, Manuscript No: AAJCP-22-53366 (R); Published: 26 March, 2022. DOI:10.35841/0971-9032.26.3.1273-1278.
Abstract
Introduction: The lockdown caused by the SARS-CoV-2 coronavirus has prompted drastic public health measures by governmental organizations which impacted especially daily life for children around the world. The aim of this study was to investigate the effect of closure of schools and kindergarten as well as restriction of leisure activities on the epidemiology of pediatric trauma injuries. Methods: This is a retrospective cohort study comparing all pediatric trauma admissions and surgical intervention in two level one pediatric trauma centre in Germany during the first lockdown in 2020 with the same pre-pandemic period in 2019. Results: During lockdown emergency consultations decreased by almost 30%. The rate of domestic (63% vs. 29%) and traffic accidents (8% vs. 12%) increased while injuries caused by sports, on playgrounds and in school and kindergarten decreased. The patients mean age was reduced (5.78 yrs vs. 4.55 yrs) with an increase in injuries especially in toddlers. Soft tissue injuries were more frequent (25% vs. 30%) than in pre-pandemic time. The number of patients requiring surgical interventions rose (40 vs. 62) in time of lockdown; especially soft tissue interventions and injuries caused by home accidents increased. Conclusion: The SARS-CoV-2 lockdown has resulted in an increase in domestic accidents, especially in toddlers. Injuries requiring surgical interventions were more common, which can probably be explained by changes in parental supervision, leisure activities and as a result of a loss of fundamental movement skills due to a lack of physical activity in preschool.
Keywords
Pediatric, Traumatology, SARS-CoV-2, Lockdown, Epidemiology, Pandemic.
Introduction
Since the first case of the novel coronavirus SARS-CoV-2 was reported in China in December 2019, the viral infection has been declared as a global pandemic by the World Health Organization on March 16 2020 [1]. The relatively high morbidity (10% to 15%) and mortality (0.25% to 4%) of SARS-CoV-2 compared with seasonal influenza has prompted drastic public health measures by governmental organizations [2]. The increasing infection rates quickly led to a global containment policy through social distancing practices. Several countries have gone through periods of being under lockdown with restrictions for public and social life requiring the population to remain at home to “flatten the curve”.
Especially children´s live have been drastically affected by the lockdown. In addition to general activity limitations this included kindergarten and school closures and also enormous restrictions on afterschool activities as past experience with viral pandemics such as the 2009 H1N1-outbreak has shown this as a potential intervention in partial containment [3,4]. Several studies reported a significant decrease of traumatic injuries in children [5-13] as accidents in school, on playgrounds and other leisure activities most frequently lead to traumatic injuries in childhood [14]. This exceptional situation led to a change in the epidemiology of childhood trauma. As far as we are aware there is no valid data collection for Germany jet. Therefore, the aim of this study was to examine how the SARS-CoV-2 pandemic have impacted the incidence, severity and characteristics of pediatric trauma injuries presented to a single level one pediatric trauma centre in Germany compared with the same period during 2019.
Methods
We performed a retrospective, comparative, epidemiological analysis assessing all acute pediatric trauma admissions in the first 8 weeks of a nationwide lockdown in Germany. This study was submitted to the ethics committee of the Hamburg medical association (WF-049/20) and approved.
All acute pediatric admissions for trauma to the level one pediatric trauma department of the university hospital of Hamburg and altonaer children’s hospital in Hamburg, Germany were analysed between March 16, 2020 and May 10, 2020. These results were then compared with the pre-pandemic period during 2019. All patients aged 0 to 16 who suffered from an accident were included; exceptions were patients with a severe major poly trauma or admissions only for wound and plaster control. The data sets were collected from electronic health record documentation in the emergency department and operating theatre. Demographic variables collected included patient age at injury and sex. Age categories were then created on the basis of the centres for disease control child development grouping [15]. Hospital-specific data included injury locations, location and type of injury. Injuries were differentiated into fractures, contusions and strains as well as soft tissue injuries. The classification of the individual injuries was based on the international statistical classification of diseases and related health problems (10th revision German modification (ICD-10-GM) version 2020). Injuries were grouped by body region using the ICD-10-Code (Table 1). Injuries that underwent surgical interventions were documented.
| Comparison period 2019 | Lockdown 2020 | p-value | |
|---|---|---|---|
| Total of patients | 1326 | 1044 | - |
| Daily incidence of presentation: | 15.54 (± 5.06) | 8.93 (± 3.65) | <0.001 |
| Average (SD) | |||
| Age (years): Average, (SD) | 5.78 (± 4.37) | 4.55 (± 3.99) | <0.001 |
| Age group: 0 to 5 years | 693 (52.26) | 602 (57.66) | <0.05 |
| Age group: 6 to 12 years | 441 (33.26) | 300 (28.74) | <0.05 |
| Age group: 13 to 16 years | 192 (14.48) | 142 (13.60) | 0.54 |
| Manchester triage: average (SD) | 3.64 (± 0.80) | 3.11 (± 1.54) | <0.001 |
| Sex (%) | |||
| Male | 766 (57.77) | 592 (56.70) | 0.6 |
| Female | 560 (42.23) | 452 (43.30) | |
| Type of injury (%) | |||
| Fractures | 203 (15.31) | 166 (15.90) | 0.69 |
| Contusions and strains | 784 (59.12) | 570 (54.59) | 0.08 |
| Soft tissue injuries | 339 (25.56) | 308 (29.50) | <0.05 |
Table 1. Demographic variables in pre-pandemic and pandemic period.
Continuous data were tabulated and analysed. Data were presented as absolute numbers, proportion (%), average, and standard deviation. 2019 and 2020 data were compared and statistically tested using the independent-samples students test for normally distributed data. Categorical data was compared using chi squared test. All comparative tests were two-tailed with a significance threshold of p<0.05. Statistical analyses were conducted utilizing IBM SPSS statistics for Macintosh, version 26.0 (IBM Corp., Armonk, NY).
Results
The study in total included 2370 patients with acute pediatric trauma consultations. During lockdown there was a significant decrease of 27% of presentations in the emergency room compared to the same period in 2019 (Table 2). This was particularly evident in the 6 to 12 year old age group (441 vs. 300; p<0.05), whereas there were more injuries in the 0 to 5 year old age group (693 vs. 602; p<0.05). The average age of injured children was significantly lower during the lockdown (5.78 ± 4.37 vs. 4.55 ± 3.99; p<0.001). The daily incidence of presentations during the pandemic of all patients was also significantly reduced (15.54 ± 5.06 vs. 8.93 ± 3.65; p<0.001) with a significant reduction in Manchester triage, which is an indication of serious overall injuries (3.64 ± 0.80 vs. 3.11 ± 1.54; p<0.001). There were no gender differences between the cohorts (p=0.60).
| Comparison period 2019 | Lockdown 2020 | p-value | |
|---|---|---|---|
| Operations (% of all injuries) | |||
| Total | 40 (3.00) | 62 (6.00) | <0.001 |
| Fractures (%) | 27 (67.5) | 30 (48.29) | 0.20 |
| Soft tissue injuries (%) | 13 (32.5) | 32 (51.61) | <0.001 |
| Operations per age group (%) | |||
| Age group: 0 to 5 | 14 (35.00) | 32 (51.61) | 0.01 |
| Age group: 6 to 12 | 16 (40.0) | 21 (33.87) | 0.52 |
| Age group: 13 to 16 | 10 (25.00) | 9 (14.52) | 0.18 |
| Mean Age (SD) | 7.67 (± 4.47) | 5.93 (± 3.89) | <0.05 |
| Operations per injury location | |||
| Home | 7 (17.50) | 27 (43.55) | <0.001 |
| Playground | 7 (17.50) | 6 (9.67) | 0.25 |
| Sports | 9 (22.50) | 7 (11.30) | 0.13 |
| Traffic | 6 (15.00) | 13 (21.00) | 0.45 |
| Kindergarten/School | 11 (27.50) | 10 (16.13) | 0.1 |
Table 2. Proportional comparison of surgical cases in 2019 and 2020.
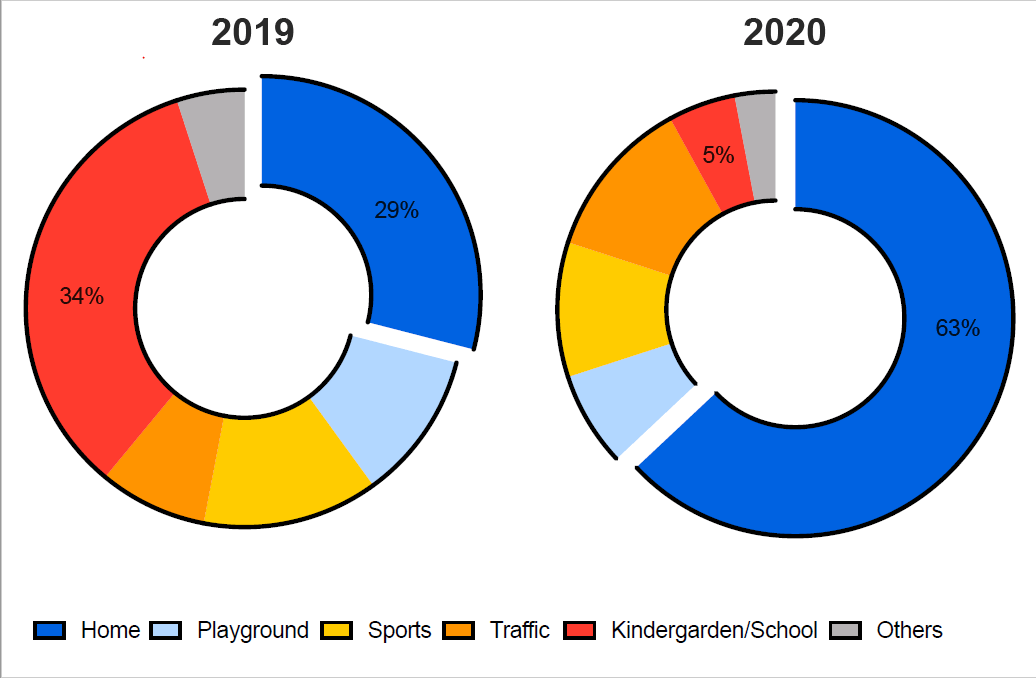
The location of injury was found to differ between lockdown and pre-pandemic period (Figure 1). There was a significant increase in the proportion of injuries occurring in or around the home (28.88% vs. 63.12%; p<0.001) and in traffic accidents (8.07% vs. 11.78%; p<0.05). Children during the pandemic were less frequently injured during sports (12.82% vs. 10.15%; p<0.05), on playgrounds (10.86% vs. 6.51%; p<0.001) and in kindergarten and school (34.16% vs. 5.07%; p<0.001). There was no difference in the incidence of fractures (15.31% vs. 15.90%; p=0.69) and contusions and strains (59.12% vs. 54.59%; p=0.08) during lockdown. However, there was a significant increase in soft tissue injuries (25.56% vs. 29.50%; p<0.05).
During lookdown children were injured at home (63% vs. 29%, p<0.001) and during traffic (12% vs. 8%, p<0.05) and less often during sports (10% vs. 13%; p<0.05), on playgrounds (6.51% vs. 10.86%; p<0.001) and in kindergarten and school (5.07% vs. 34.16%; p<0.001).
The proportion of injuries to the upper extremity (p=0.665) and the lower extremity (p=0.281) showed no difference compared to 2019 (Table 3). Injuries to the head accounted for the largest proportion of injuries in lockdown as well as in 2019 (49.44% vs. 51.91%). This was followed by injuries to the elbow/forearm (12.60% vs. 11.30%), injuries to the wrist/hand (12.00%, 12.00%) and injuries to the ankle/foot (9.10% vs. 10.00%). Significant differences could only be demonstrated for injuries to the Knee/Lower leg (6.90% vs. 4.30%; p<0.05). Furthermore, we did not see any changes in any of the other body regions compared to the pre-pandemic period in 2019 (neck: 1.05% vs. 1.70%; chest: 0.80% vs. 1.10%; abdomen/pelvis/spine: 3.20% vs. 2.00%; shoulder/upper arm: 4.40% vs. 4.00%; hip joint/thigh: 1.05% vs. 1.00%).
| Comparison period 2019 | Lockdown 2020 | p-value | |
|---|---|---|---|
| Injuries to body regions (%) | |||
| Head | 657 (49.55) | 542 (51.91) | 0.598 |
| Neck | 23 (1.70) | 11 (1.05) | 0.166 |
| Chest | 15 (1.10) | 8 (0.80) | 0.368 |
| Abdomen/pelvis/thoracic and lubar spine | 27 (2.00) | 33 (3.20) | 0.083 |
| Sholder/upper arm | 53 (4.00) | 46 (4.40) | 0.621 |
| Elbow/forearm | 167 (12.60) | 118 (11.30) | 0.337 |
| Wrist/hand | 159 (12.00) | 126 (12.00) | 0.954 |
| Hip Joint/thigh | 13 (1.00) | 11 (1.05) | 0.859 |
| Knee/lower leg | 91 (6.90) | 45 (4.30) | <0.05 |
| Ankel/foot | 121 (9.10) | 104 (10.00) | 0.49 |
| Upper extremity | 379 (28.50) | 290 (27.70) | 0.665 |
| Lower extremity | 225 (17.00) | 160 (15.30) | 0.281 |
| Others | 722 (54.36) | 594 (56.89) | 0.218 |
Table 3. Injury characteristics in pre-pandemic and pandemic time period.
During the lockdown more patients required operative intervention (3.00% vs. 6.00%; p<0.001) compared with 2019 (Table 2), which was due to an increase in soft tissue interventions (32.5% vs. 51.61%; p<0.001). The age group of 0-5 year olds was particularly affected (p=0.1). However, there was a clear reduction in the patients mean age requiring an operation (7.67 ± 4.47 vs. 5.93 ± 3.89; p<0.05). Injuries sustained by domestic accidents during lockdown required more surgical interventions compared to the previous year (17.50% vs. 43.55%; p<0.001), while otherwise the injuries in traffic accidents, in sports, on playgrounds and in school and kindergarten did not change substantially (Table 2).
Discussion
The SARS-CoV-2 pandemic has impacted all aspects of daily life, especially for children. With the combination of the closure of schools and kindergarten, public parks, playgrounds and many other facilities as well as the indefinite disbanding of organized sports, changes in the epidemiology of pediatric trauma injuries was expected. Several countries around the world have studied the local effects of SARS-CoV-2 lockdown on pediatric and adult traumatology patients. Most studies reported a decrease of emergency consultations in Spain [16] and fractures in children in New Zealand [5]. This resulted in a simultaneous decrease in surgical interventions for trauma cases in 30%-60% [6-13]. Only, two studies found an increase in domestic’s accidents (23% vs. 59%) requiring surgery compared to recreational sports accidents (24% vs. 2%). Moreover, an increase in home trampoline injuries were reported [12].
The present study found a decrease in the pediatric trauma emergency consultations of almost 30%. This may be explained by the closure of schools and kindergartens, public parks and playgrounds and recreational sports, which has already been reported [6,14,17]. In addition, the decline in emergency consultations can be explained by the fear of possible infection in the hospital, which may have discouraged families with minor injuries. This is reflected by a lowered mean value of the Manchester triage and could already be shown in the context of the current pandemic as well as previous epidemics like the H1N1 outbreak in Hong Kong [18], Taiwan [19] or Turkey [20,21] in in 2009.
In contrast to previous reports, the number of injuries in which surgery was required increased significantly in the current study; especially, in the age group of 0–5 year olds. Most notably, an increase in soft tissue injuries requiring surgery was found, which was also see in the study by Bolinger et al. [13]. This may be explained by the fact that in comparison to many other studies, our work included not only injuries to the extremities, but also injuries to other body regions such as to the head and face, which often occur particularly in preschool children (<5 years) at home [22-24].
The frequent occurrence of wounds at the head in toddlers can certainly be explained by the disproportionately large head and with the lack of coordination and fundamental movement skills. Fundamental Movement Skills (FMS) are the basic building blocks required for mastering the complex, task-specific movements needed for participation in sports, playing and other activities [25]. FMS consist of object control (e.g. throwing or catching a ball or ball skills), loco motor (e.g. running, hopping, skipping), and stability (e.g. balance) skills [26]. The appropriate development of FMS, which occurs during the preschool period (children aged 3–5 years) through copying and repetitive exercise, allows building the basis for performing complex movements and task-specific abilities [27-30]. Moreover, several studies reported that the practice of physical activity in preschool improves FMS level by inducing a higher motor skill competence in childhood [31-34]. For these reasons, the practice of structured physical activity in kindergarten during this period results to be crucial [35-38]. Physical activity of 15 to 20 minutes 4 days a week is enough to improve fundamental movement skills and therefore motor development [39]. The absence of fine motor development was found by Myhre et al. to be the cause of an increased risk of injuries in toddler’s [40]. Toddlers' physical development often precedes their ability to understand the consequences of their actions, and early physical mobility can significantly increase the risk of injury to children. An impaired fine motor development may be linked to clumsiness, leading to injury proneness. As children were deprived from typical motor activities during lookdown measure, lack of FMS may explain the increase of severe injuries resulting in surgery during the pandemic [41].
In addition, children may be looked after differently at home by their parents than in kindergarten or school. It has been reported that mothers have to organize home office, housekeeping and child care simultaneously which little external support by other family members and social support systems [42]. Adequate adult supervision is essential for toddlers to stay free from harm [43-45]. Many domestically injuries among young children are the results of inadequate supervision. Differences in parental supervision or the possibility that older siblings sometimes act as chaperones may also explain the increased injury rate in our cohort. It has been reported that children may behave more riskily and show poor compliance if they are supervised by their sibling’s. In addition, due to the lack of leisure activities and sports, children are underutilized, which can lead to impulsiveness and carelessness, which may contribute to the tendency of children to put themselves in potentially dangerous situations.
Conclusion
The present study shows a decrease in pediatric emergency consultations during lockdown of almost one third with a significant decrease in the proportion of injuries occurring during sports, on playgrounds and in kindergarten and school. There was an increase in accidents at home, with younger children in particular being affected. Soft tissue injuries were more frequent than in pre-pandemic time. Above all, the rate of surgically treated injuries rose in times of lockdown, which can probably be explained by changes in supervision, leisure time activities and as a consequence, in motor skills. These findings could help health authorities and scientific societies to develop public information campaigns to prevent domestic accidents in young children and to provide support for parents during times of pandemics.
References
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
- Xie J, Tong Z, Guan X et al. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med 2020; 46: 837–840. [Crossref][Google Scholar][Indexed]
- Cauchemez S, Ferguson NM, Wachtel C, et al. Closure of schools during an influenza pandemic. The Lancet Infectious Diseases 2009; 9(8): 473–481. [Crossref][Google Scholar][Indexed]
- Jackson C, Mangtani P, Hawker J, et al. The effects of school closures on influenza outbreaks and pandemics: Systematic review of simulation studies. PLoS ONE 2014; 9(5): e97297. [Crossref][Google Scholar][Indexed]
- Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop 2020; 40(8): 373-379. [Crossref][Google Scholar][Indexed]
- Gumina S, Proietti R, Villani C, et al. The impact of COVID-19 on shoulder and elbow trauma in skeletally immature population. An Italian survey. JSES Int 2021; 5(1): 3-8. [Crossref][Google Scholar][Indexed]
- Nabian MH, Vosoughi F, Najafi F, et al. Epidemiological pattern of pediatric trauma in COVID-19 outbreak: Data from a tertiary trauma centre in Iran. Injury 2020; 51(12): 2811-2815. [Crossref][Google Scholar][Indexed]
- Greenhalgh M, Dupley L, Unsworth R, et al. Where did the entire trauma go? A rapid review of the demands on orthopaedic services at a UK major trauma centre during the COVID?19 pandemic. Int J Clin Pract 2021; 75(3): e13690. [Crossref][Google Scholar][Indexed]
- Turgut A, Arli H, Altundag U, et al. Effect of COVID-19 pandemic on the fracture demographics: data from a tertiary care hospital in turkey. Acta Orthop Traumatol Turc 2020; 54(4): 355–363. [Crossref][Google Scholar][Indexed]
- Murphy T, Akehurst H, Mutimer J. Impact of the 2020 COVID-19 pandemic on the workload of the orthopaedic service in a busy UK district general hospital. Injury 2020; 51(10): 2142–2147. [Crossref][Google Scholar][Indexed]
- Ibrahim Y, Huq S, Shanmuganathan K, et al. Trampolines injuries are bouncing back. Bone Jt Open 2021; 2(2): 86-92. [Crossref][Google Scholar][Indexed]
- Bolzinger M, Lopin G, Accadbled F, et al. Pediatric traumatology in "green zone" during Covid-19 lockdown: A single-center study. Orthop Traumatol Surg Res 2020; 102946. [Crossref][Google Scholar][Indexed]
- Joeris A, Lutz N, Wicki B, et al. An epidemiological evaluation of pediatric long bone fractures: A retrospective cohort study of 2716 patients from two swiss tertiary pediatric hospitals. BMC Pediatrics 2014; 14(1): 1-9. [Crossref][Google Scholar][Indexed]
- Critical care crisis and some recommendations during the COVID-19 epidemic in China.
- Nuñez JH, Sallent A, LakhanI K, et al. Impact of the COVID-19 pandemic on an emergency traumatology service: Experience at a tertiary trauma centre in Spain. Injury 2020; 51(7): 1414–1418. [Crossref][Google Scholar][Indexed]
- Naranje SM, Erali RA, Warner WC, et al. Epidemiology of Pediatric Fractures Presenting to Emergency Departments in the United States. Journal of Pediatric Orthopaedics 2016; 36(4): e45–e48. [Crossref][Google Scholar][Indexed]
- Lau JTF, Griffiths S, Choi KC, et al. Avoidance behaviours and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect Dis 2010; 10: 139. [Crossref][Google Scholar][Indexed]
- Chang HJ, Huang N, Lee CH, et al. The Impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health 2004; 94(4): 562–564. [Crossref][Google Scholar][Indexed]
- Nicholson E, Mc Donnell T, Conlon C, et al. Parental hesitancy and concerns around accessing paediatric unscheduled healthcare during COVID-19: A cross-sectional survey. Int J Env Res Public Health 2020; 17(24): 9264. [Crossref][Google Scholar][Indexed]
- Gayg?s?za Ü, Gayg?s?zb E, Özkanc T, et al. Individual differences in behavioral reactions to H1N1 during a later stage of the epidemic. J Infect Public Health. 2012; 5(1): 9-21. [Crossref][Google Scholar][Indexed]
- Hawley C, Wilson J, Hickson C, et al. Epidemiology of paediatric minor head injury: Comparison of injury characteristics with indices of multiple deprivations. Injury 2013; 44(12): 1855-61. [Crossref][Google Scholar][Indexed]
- Quayle KS, Holmes JF, Kuppermann N. Epidemiology of blunt head trauma in children in US emergency departments. N Engl J Med 2014; 371(20): 1945–1947. [Crossref][Google Scholar][Indexed]
- Kang MS, Kim HS. Characteristics and trends of traumatic injuries in children visiting emergency departments in South Korea: A retrospective serial cross-sectional study using both nationwide-sample and single-institutional data. PLOS ONE 2019; 14(8): e0220798. [Crossref][Google Scholar][Indexed]
- Clark JE. From the beginning: A developmental perspective on movement and mobility. Taylor Francis Online 2005; 57(1); 37–45. [Crossref][Google Scholar]
- Stodden DF, Goodway JD, Langendorfer SJ, et al. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. 2008; 60(2): 290–306. [Crossref][Google Scholar][Indexed]
- Figueroa R, An R. Motor skill competence and physical activity in pre-schoolers: a review. Matern Child Health J. 2017; 21: 136–146. [Crossref][Google Scholar][Indexed]
- Alves JGB, Alves GV. Effects of physical activity on children's growth. J Pediatr 2019; 95: 72–78. [Crossref][Google Scholar][Indexed]
- Iivonen KS, Sääkslahti AK, Mehtälä A, et al. Relationship between fundamental motor skills and physical activity in 4-year-old preschool children. Perceptual and Motor Skills 2013; 117(2): 627–646. [Crossref][Google Scholar][Indexed]
- Aivazidis D, Venetsanou F, Aggeloussis N, et al. Enhancing motor competence and physical activity in Kindergarten. J Phys Act Health 2019; 16: 184–190. [Crossref][Google Scholar][Indexed]
- Fisher A, Reilly JJ, Kelly LA, et al. Fundamental movement skills and habitual physical activity in young children. Med Sci Sports Exerc 2005; 37: 684–688. [Crossref] [Google Scholar][Indexed]
- Hardy LL, King L, Kelly B, et al. Munch and move: Evaluation of a preschool healthy eating and movement skill program. Int J Behav Nutr Phys Act 2010; 7: 80. [Crossref][Google Scholar][Indexed]
- Battaglia G, Alesi M, Tabacchi G, et al. The development of motor and pre-literacy skills by a physical education program in preschool children: A non-randomized pilot trial. Front Psychol 2018; 9: 2694. [Crossref][Google Scholar][Indexed]
- Nilsen AKO, Anderssen SA, Johannessen K, et al. Bi-directional prospective associations between objectively measured physical activity and fundamental motor skills in children: A two-year follow-up. Int J Behav Nutr Phys Act 2020; 17: 1. [Crossref][Google Scholar][Indexed]
- Deli E, Bakle I, Zachopoulou E. Implementing intervention movement programs for kindergarten children. J Early Childhood Res 2006; 4: 5–18. [Crossref][Google Scholar]
- Barbosa SC, Coledam DH, Stabelini NA, et al. School environment, sedentary behaviour and physical activity in preschool children. Rev Paul Pediatr 2016; 34: 301–308. [Crossref][Google Scholar][Indexed]
- Kippe KO, Lagestad PA. Kindergarten: Producer or reducer of inequality regarding physical activity levels of preschool children. Front Public Health 2018; 6: 361. [Crossref][Google Scholar][Indexed]
- Jarraya S, Wagner M, Jarraya M, et al. 12 Weeks of kindergarten-based yoga practice increases visual attention, visual-motor precision and decreases behavior of inattention and hyperactivity in 5-year-old children. Front Psychol 2019; 10: 796. [Crossref][Google Scholar][Indexed]
- Bellows LL, Davies PL, Anderson J, et al. Effectiveness of a physical activity intervention for head start pre-schoolers: A randomized intervention study. Am J Occup Ther 2012; 67(1): 28–36. [Crossref][Google Scholar][Indexed]
- Garcia C, Garcia L, Floyd J, et al. Improving public health through early childhood movement programs. J Phys Educ Recreat 2002; 73(1): 27–31. [Crossref][Google Scholar]
- Myhre MC, Thoresen S, Grøgaard JB, et al. Familial factors and child characteristics as predictors of injuries in toddlers: A prospective cohort study. BMJ Open 2012; 2(2): e000740. [Crossref][Google Scholar]
- Xiao Y, Becerik-Gerber B, Lucas G, et al. Impacts of working from home during covid-19 pandemic on physical and mental well-being of office workstation users. J Occup Environ Med 2021; 63(3): 181-190. [Crossref][Google Scholar][Indexed]
- Morrongiello BA, Corbett M, Brison RJ. Identifying predictors of medically-attended injuries to young children: Do child or parent behavioural attributes matter? Inj Prev 2009; 15(4): 220-5. [Crossref][Google Scholar][Indexed]
- Schwebel DC, Brezausek CM, Ramey SL, et al. Interactions between child behavior patterns and parenting: implications for children's unintentional injury risk. Pediatr Psychol 2004; 29(2): 93-104. [Crossref][Google Scholar][Indexed]
- Morrongiello BA, Klemencic N, Corbett M. Interactions between child behaviour patterns and parent supervision: Implications for children's risk of unintentional injury. Child Dev. 2008; 79(3): 627-38. [Crossref][Google Scholar][Indexed]
- Morrongiello BA, Schell SL, Schmidt S. "Please keep an eye on your younger sister": sibling supervision and young children's risk of unintentional injury. Injury Prevention 2010; 16: 398-402. [Crossref][Google Scholar][Indexed]