- Biomedical Research (2011) Volume 22, Issue 4
Impact of depression and anxiety disorders on gastrointestinal symp-toms and its prevalence in the general population
Abdulbari Bener1, 2* and Elnour E. Dafeeah3
1Department of Medical Statistics & Epidemiology, Hamad General Hospital and Hamad Medical Corporation, Doha, Qatar.
2Department Evidence for Population Health Unit, School of Epidemiology and Health Sciences, University of Man-chester, Manchester, UK.
3Department of Psychiatry, Rumailah Hospital, Hamad Medical Corporation, Doha, Qatar.
- *Corresponding Author:
- Abdulbari Bener
Department of Medical Statistics & Epidemiology
Hamad Medical Corporation and Department of Public Health, Dept. of Public Health, Weill Cornell Medical College, PO Box 3050, Doha- State of Qatar
Accepted Date: Accepted June 18 2011
Abstract
High rates of psychiatric disorder have been documented in patients with gastrointestinal (GI) symptoms. The aim of this study was to examine the prevalence of gastrointestinal (GI) symptoms among the general adult population and to determine if psychological dis-tress such as depression and anxiety disorder is associated with gastrointestinal disorders. This is a cross sectional study conducted during the period September 2009 to May 2010 at the Primary Health Care Centers of the Supreme Council of Health, State of Qatar. A total of 1208 patients aged 20 years and above were approached and 934 patients (77.3%) participated in this study. The study was based on a face to face interview with designed diagnostic screening questionnaires for GI symptoms, Patient Health Questionnaire (PHQ-9) for depression and General Anxiety Disorders (GAD-7) for anxiety. The ques-tionnaire consists of questions about symptoms and signs of anxiety and depression disor-ders. Also, socio-demographic characteristics, life style habits and family history of pa-tients were collected. Of the studied subjects, 62.1% were males and 37.9% were females. Out of 934 subjects interviewed, the prevalence of gastrointestinal symptoms was 41.1%. Most of the sufferers with GI symptoms were male patients (69.8%) and in the age group 45-54 years (39.6%). The prevalence of severe levels of depression was nearly twofold (8.6%) in GI patients compared to their counterparts (4.5%). The prevalence rate of anxi-ety was higher in sufferers of GI symptoms (21.4%). Mental health severity (mean ± SD) was significantly higher in male patients with GI symptom compared to females; depres-sion (7.9±4.2 vs. 6.9±4.5, p<0.001) and anxiety 7.0±3.6 vs. 6.1±3.6, p=0.001). More than de-pression, anxiety was more common in patients of GI symptoms of constipation (22.3%), upper dysmotility (21.4%) and diarrhoea (20.7%). The present study findings revealed that the prevalence rate of gastrointestinal disorders is high in the primary care settings. Also, GI symptoms are associated significantly with depression and anxiety. Anxiety was more common than depression in GI patients
Keywords
prevalence, depression, Primary health care, anxiety, Qatar
Introduction
Gastrointestinal symptoms are very common in the gen-eral population and a frequent reason for consulting a health care professional [1]. In Western countries, GI symptoms are very common and are reported within three months by almost every other adult [2,3]. Gastro-intestinal disturbances commonly include symptoms of stomach pain, heart burn, diarrhoea, constipation, nau-sea and vomiting. In the United States, abdominal pain accounts for more than 10 million clinical visits annu-ally [4]. In the Netherlands, digestive diseases occur in 2 million of the country’s citizens annually, and make up 13% of the total mortality, 12% of the hospital admis-sions and 17% of total hospital days [5]. Many patients with irritable bowel syndrome (IBS) or other functional gastrointestinal disorders present extraordinary man-agement problems for physicians. The impact of GI may be very psychological and stress provoking. It was re-ported that higher rates of psychiatric co-morbidity occur with the functional bowel disorders that are particu-larly high in community populations [6]. An estimated 57 million adults suffer from anxiety disorders [7]. De-pression and anxiety have been implicated in several chronic physical illness including gastrointestinal disor-ders, heart diseases and chronic respiratory disorders. Comorbid psychiatry disorders can adversely influence the management and outcome of GI disorders particu-larly health-related quality of life [8]. Mental disorders are common in all countries and cause immense suffer-ing [9].
Psychiatric disorders are prevalent in medical practice, especially in primary care, where as many as one-third of patients may suffer from one or more current diag-nosable psychiatric disorders, especially depressive and anxiety disorders [10]. Two recent studies done in Qatar by Bener [11,12] revealed that depression and anxiety were more prevalent in Qatari population and a good proportion of sufferers with anxiety and depres-sion were quite disturbed in their day to day life. Over the past two decades, the State of Qatar has experienced a rapid transition in its socio-economic status and wit-nessed rapid change in many aspects of life. Similarly, several changes in factors associated with the develop-ment and treatment of GI disorders have taken place. Although these changes might have altered the aetiology and prevalence of underlying disorders, GI symptoms are still very common in the general population. In line with the rapid life style changes among population, the prevalence of overweight and obesity is increasing. These developments strengthened the need for a re-search on the current prevalence of GI symptoms in the general population and its association with the psycho-social factors.
There has been limited research on the prevalence of GI symptoms and aetiology of anxiety and depression in primary care in developing countries. However, there is only limited knowledge on the association of GI symp-toms, anxiety, and depression in medical settings, and primary care studies investigating this issue are com-pletely lacking. Also, in the Middle East region, no study has yet been conducted on the prevalence of GI symptoms among the general population as well as their psychosocial impact. The aim of this study was to inves-tigate the prevalence of GI symptoms in the primary care setting and its relationship with depression and anxiety disorders.
Subjects and Methods
This is a cross-sectional study based in the primary health care centers (PHC). The survey was conducted among the population residing in the State of Qatar from September 2009 to May 2010. Primary health care centers are frequented by all levels of the general popula-tion as a gateway to specialist care. The study was ap-proved by the Hamad General Hospital, Hamad Medical Corporation. All human studies have been approved by the Research Ethics Committee and have been per-formed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
A multistage stratified random sampling design was developed using an administrative division of the Qatar into 21 primary health care centers in terms of number of inhabitants. Of these health centers, 10 health centers in urban areas and 3 health centers in semi-urban areas were visited mostly by Qatari people and remaining health centers were excluded from the survey. Also, we have selected 13 health centers representing geographi-cally and have taken equal proportion of subjects from these selected health centers according to the inhabitants in that district. The sample size was determined on a priori presumption that the prevalence rate of somatisa-tion in Qatar would be more or less similar to rates found for several other countries in the Arabian Gulf and Eastern Mediterranean [11-12], where the reported prevalence of GI symptoms among adults ranged from 20 to 25%. Assuming the prevalence of depression and anxiety disorders to be 22.5%, with the 99% confidence interval for an error of 3% at the level of significance, a sample size of 1208 subjects would be required to meet the objectives of the study. During the study period, 1208 subjects were approached, of whom 934 subjects responded to the questionnaire, with a response rate of 77.3%. The survey instrument [13-14] was tested on 100 patients who visited the health centers and thus validated the questionnaire. The study excluded pa-tients below 20 years and above 65 years, patients with any cognitive or physical impairment and who refused to give consent to take part in the study.
The data was collected through validated self-administered questionnaires with the help of qualified nurses. The questionnaire had three sections. The first part included the socio-demographic details, medical and family history, and dietary habits of patients. The second part included the most prevalent GI symptoms in primary care like oesophageal symptoms, upper dysmo-tility symptoms, constipation, and diarrhoea. Depres-sion was assessed with the eight-item depression mod-ule of the PHQ-9 [15]. Patients were asked to answer the questions by grading them from 0 to 3; with 0 for “not at all”, 1 for “several days”, 2 for “more than half days” and 3 for “nearly every day”. Anxiety was as-sessed with the GAD-7[16]. Patients were asked to an-swer the questions by grading them from 0 to 3; with 0 for “not at all”, 1 for “several days”, 2 for “more than half the days”, and 3 for “nearly every day”. PHQ-9 ≥15 represent severe symptoms of depression and GAD≥11 represent severe symptoms of anxiety disor-ders. We used cutoff scores of ≥ 15 on PHQ-9 and cut-off score of ≥ 11 on GAD-7, because this threshold re-flects severe levels of depression and anxiety disorders.
Student-t test was used to ascertain the significance of differences between mean values of two continuous variables. Chi-square analysis was performed to test for differences in proportions of categorical variables be-tween two or more groups. In 2x2 tables, the Fisher's exact test (two-tailed) replaced the chi-square test if the assumptions underlying violated, namely in case of small sample size and where the expected frequency is less than 5 in any of the cells. The level p<0.05 was considered as the cut-off value for significance.
Results
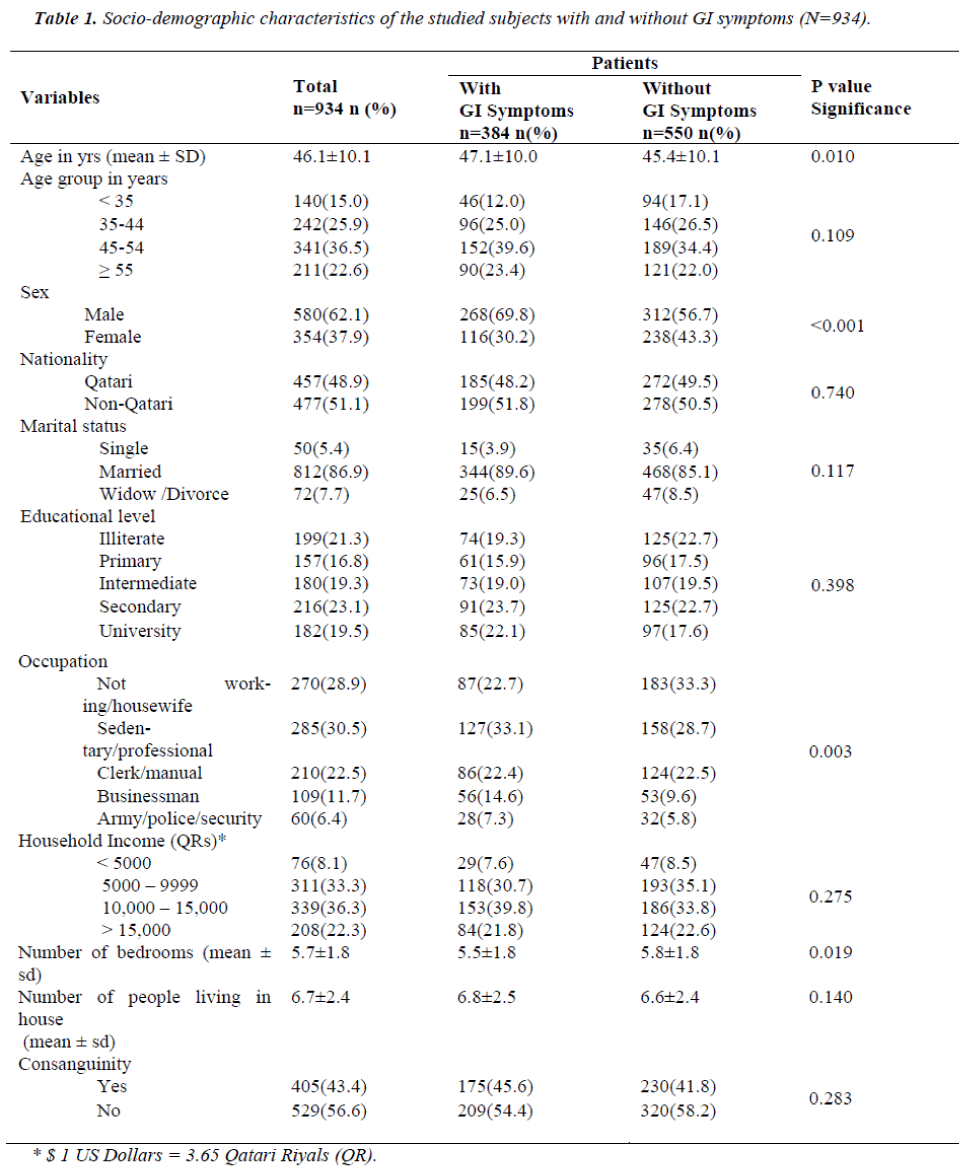
Table 1 shows the socio-demographic characteristics of the studied subjects with and without GI symptoms. Of the studied subjects, 62.1% were males and 37.9% were females. Most of the respondents were in the age group 45 - 54 years (36.5%). The majority of them were mar-ried (86.9%), educated with secondary school certificate (23.1%) and with sedentary/professional job (30.5%). Out of 934 subjects interviewed, the prevalence of gas-trointestinal symptoms was 41.1%. Most of the suffer-ers with GI symptoms were in the age group 45 – 54 years (39.6%), followed by 20 – 44 years (25%). Pa-tients with GI symptoms were significantly more often men (69.8%;p<0.001) and professionals (33.1%; P=0.003). Nearly half of the patients with GI symptoms were consanguineous (45.6%).
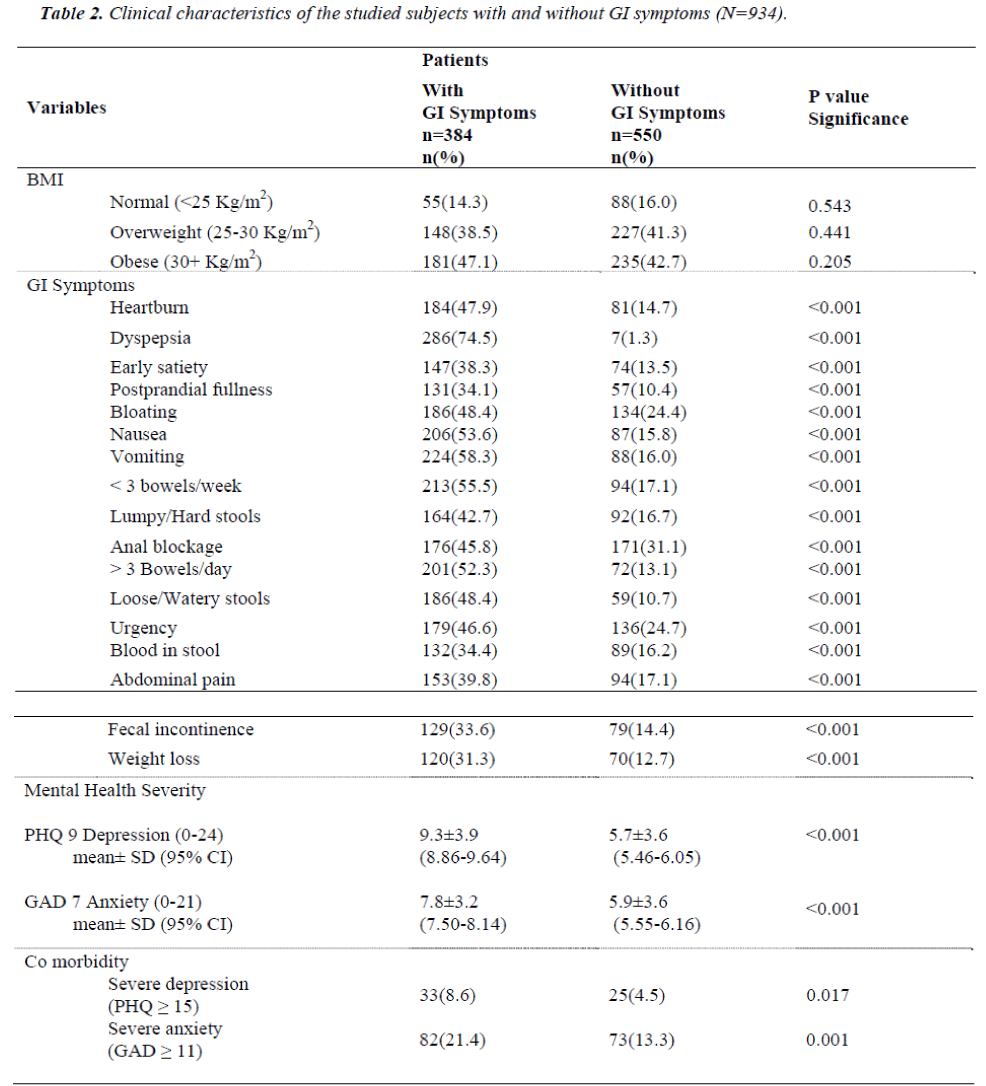
Table 2 presents the clinical characteristics of the stud-ied subjects with and without GI symptoms. Obesity was higher in patients with GI symptoms (47.1%) com-pared to the patients without GI symptoms (42.7%). The most frequently reported GI symptoms were dys-pepsia (74.5%), vomiting (58.3%), <3 bowels/week (55.5%) and> 3 bowels/day (52.3%). Patients with GI symptoms had significantly higher mean±SD scores of depression (9.3±3.9 vs 5.7±3.5;p<0.001) and anxiety (7.8±3.2 vs 5.9±3.7;p<0.001) compared to patients without GI symptoms. The prevalence of severe levels of depression was nearly twofold (8.6%) in patients with GI symptoms compared to patients without GI symp-toms (4.5%) and the prevalence of severe levels of anxi-ety was 21.4% in patients with GI symptoms, whereas it was lower in patients without GI symptoms (13.3%).
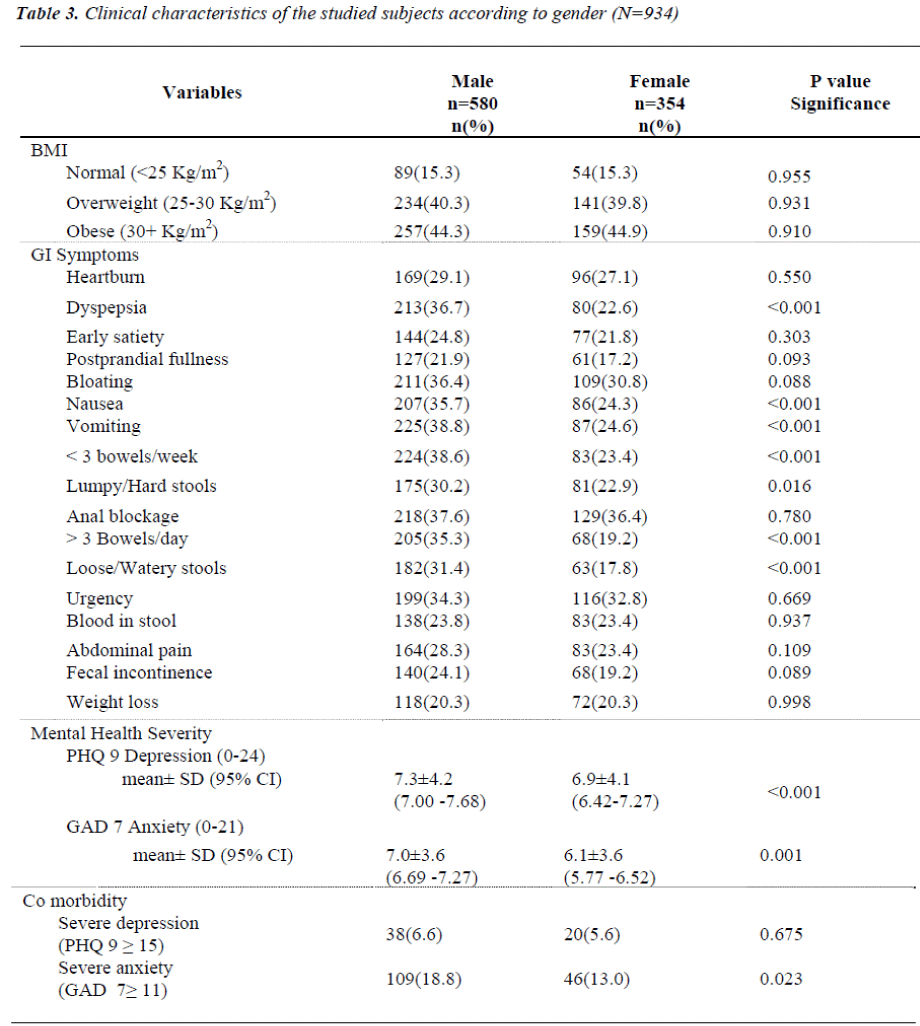
Table 3 examines the clinical characteristics of the stud-ied subjects with and without GI symptoms according to gender. Importantly, there were few significant differ-ences in prevalence of symptoms between males and females; dyspepsia (36.7% vs 22.6%;p<0.001), nausea (35.7% vs 24.3%;p<0.001), vomiting (38.8% vs 24.6%; p<0.001), <3 bowels/week (38.6% vs 23.4%; p<0.001), >3 bowels/day (35.3% vs 19.2%; p<0.001) and loose/watery stools (31.4% vs 17.8%, p<0.001). Mental health severity (mean±SD) was significantly higher in male patients with GI symptoms compared to females; for depression (7.9±4.2 vs 6.9±4.5, p<0.001) and for anxiety 7.0±3.6 vs 6.1±3.6, p=0.001).
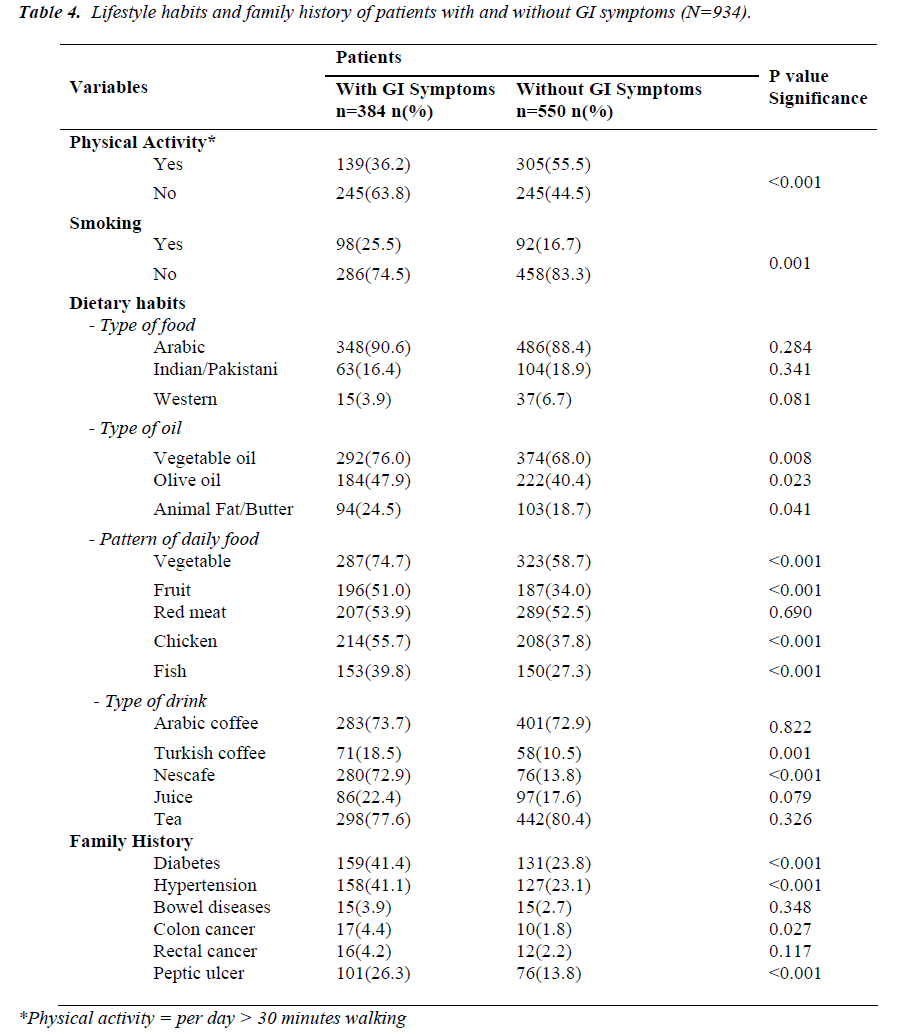
Table 4 shows the lifestyle habits and family history of subjects with and without GI patients. Physical activity was significantly less frequent in patients with GI symp-toms (36.2% vs 55.5%; p<0.001), while smoking was significantly higher in patients with GI symptoms (25.5%) compared to their counterparts (16.7%). Fam-ily history of diabetes (41.4%; p<0.001), hypertension (41.1%;p<0.001) and Peptic ulcer (26.3%; p<0.001) was significantly higher in sufferers of GI symptoms. Ma-jority of the patients with GI symptoms preferred arabic food (90.6%), arabic coffee (73.7%), tea (77.6%) and nescafe (72.9%).
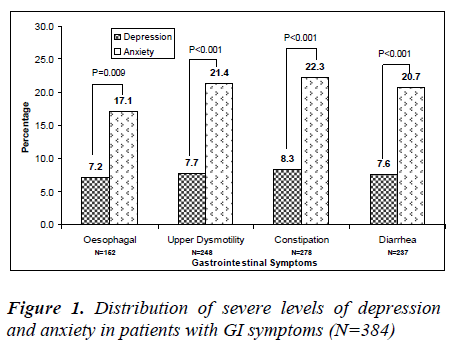
Figure 1 reveals the distribution of severe levels of de-pression and anxiety in patients with GI symptoms. Prevalence of anxiety was observed more in patients with GI symptom of constipation (22.3%), followed by upper dysmotility (21.4%) and diarrhoea (20.7%) (p<0.001). The prevalence of depression was similar in all the reported GI symptoms; constipation (8.6%), up-per dysmotility (8.1%), diarrhoea (8%) and oesophagal symptoms (7.9%).
Discussion
Gastrointestinal diseases are common worldwide. The present study is the first primary care based survey of gastrointestinal symptoms in the State of Qatar and ex-amines the impact of comorbid anxiety and depression on GI symptoms. The present study revealed that the prevalence of gastrointestinal symptoms in Qatar popu-lation was considerably high (41.1%). A community study done by Haug et al [17] found that 48% of the population reported one or more of the GI symptoms which is similar to the rate found in the Qatari commu-nity. These prevalence rates are consistent with a study from Northern Sweden in which prevalence of gastro-esophagal reflux symptoms over a three month period was found to be about 40% [18]. On the contrary, NIMH Epidemiologic Catchment Area (ECA) study revealed a lower prevalence of gastrointestinal symp-toms in the general population (6-25%) [19].
In the present study, men were more likely than women to be adversely affected by GI symptoms (69.8%). On the contrary, in the U.S [20], women are twice as likely as men to be diagnosed with the irritable bowel syn-drome as well as in other western countries. In other country like India [20], an equal number of men and women are diagnosed with GI symptoms. A recent study by Longstreth et al [21] also supported this result that Irritable bowel syndrome, which is one of the most common and well studied of the functional gastrointes-tinal disorders, occurred in women twice as frequently as in men. Among the studied patients, most of the GI sufferers were in the age group 45-54 years (39.6%). Another study revealed similar results that mean age of the participating patients with GI symptoms was found 46.3 years [4]. These study findings support each other that GI symptoms are a major problem in the commu-nity.
In the present study, the most bothersome GI symptoms were dyspepsia (74.5%), vomiting (58.3%), <3 bow-els/week (55.5%) and >3 bowels/day (52.3%). In an-other study, the most frequently reported gastrointestinal symptoms were bloating (37%), abdominal rumbling (40%), alternating solid and loose faeces (31%) and strong urgency (24%) [22]. Similar GI symptoms were noted by Creed et al in his study that the most common GI disorder was Irritable bowel syndrome, which comes in three general forms, namely constipation, diarrohoea and alternating diarrhoea and constipation [23]. But in few studies, the reported GI symptoms were upper ab-dominal pain or discomfort ranged from approximately 8% to 54%, while the prevalence of heartburn ranged from 10% to 48% [24].
The present study findings have shown that primary care patients with GI symptoms have adverse health behaviour such as obesity, sedentary life style and smo-king. For example, physical activity (36.2% vs. 55.5%) was significantly less frequent in GI patients, while smoking (25.5% vs. 16.7%) was significantly higher in them compared to their counterparts. GI patients were more obese (47.1%) than patients without GI symptoms (42.7%). A high body mass index and the life style hab-its that precede that are associated with the development of both upper and lower gastrointestinal symptoms, such as regurgitation, gastro-oesophageal reflux and altered bowel movements [25].
A substantial literature supports clinically important associations between psychiatric illness and chronic medical conditions. However, very few primary care studies have investigated the relationship between gas-trointestinal symptoms, depression and anxiety. Because depression and anxiety disorders and GI symptoms commonly occur together [26,27], this study has care-fully evaluated whether depression and anxiety are linked to gastrointestinal symptoms in Qatar. It was re-ported that patients [26] with GI symptoms report more life stress and psychological distress than healthy con-trols. More severe life stress has been found to be a very strong predictor of subsequent symptom severity in pa-tients with GI symptoms and diabetes [28]. The data in the present study strongly support the association of GI symptoms with depression and anxiety disorders.
In the present study, the prevalence of mental distress differed significantly between patients with GI symp-toms and without GI symptoms. Mental health severity (mean±SD) was considerably higher in patients with GI symptoms when compared to patients without GI symp-toms; depression (9.3±3.9 vs. 5.7±3.5) and anxiety (7.8±3.2 vs. 5.9±3.7). The prevalence of severe levels of depression was nearly twofold (8.6%) in patients with GI symptoms and the prevalence of severe levels of anxiety was 21.4% in GI patients. A lower prevalence rate was observed for depression among subjects who report at least one of the GI symptoms, when compared with those reporting no gastrointestinal symptoms (7.5% vs 2.9%) [19]. Another study [17] revealed a higher prevalence rate than in the present study; 15.3% of the GI patients had an anxiety disorder and 10.4% depression. A population based study documented that psychological illness proved to be an important comor-bidity factor among patients with GI symptoms and the severity of the two were linked [27]. Prevalence of anxiety was observed more in patients with GI symptom of constipation (22.3%), followed by upper dysmotility (21.4%) and diarrhoea (20.7%). In this study, patients who report GI symptoms have an elevated risk for anxi-ety disorders than depression. A previous study [9,11,12,28] on mental health illness in Qatar highlighted the great need for the effective promotion of good mental health awareness programs in the community.
These findings suggest that mental disorders in patients with GI symptoms are not merely a consequence of se-lection bias in patients, but connected to the symptoms themselves. These study findings suggest that anxiety disorders in GI patients should not be ignored and could be considered with depression when developing strate-gies for screening and intervention, particularly in pri-mary care. Future studies are needed in primary care populations where prevalence of psychiatric illness are probably high.
Conclusion
The study findings revealed that gastrointestinal symp-toms were considerably high in Qatar population which is consistent with previous studies done in the primary care setting. Most of the GI sufferers were in the age group 45-54 years. In this population study, there was a strong relationship between gastrointestinal symptoms, anxiety disorder and depression. Patients with GI symp-toms had significantly higher mean score of depression and anxiety. The prevalence of severe levels of anxiety and depression was considerably higher in patients with GI symptoms.
Role of funding source
This research was supported by the by the Qatar Na-tional Research Fund- QNRF NPRP 30-6-7-38. The sponsor of the study had no role in study design; in the collection, analysis and interpretation of data; in the writing of this report; and in the decision to submit the paper for publication.
Contributors
A. Bener designed and supervised the study and was involved in data collection, statistical analysis the writ-ing of the paper. E.E. Dafeeah was involved in data col-lection, interpretation of data. All authors approved the final version.
Conflict of interest
All authors declare that they have no conflicts of inter-est.
Acknowledgements
This study was generously supported and funded by the Qatar National Research Fund- QNRF NPRP 30-6-7-38. The authors would like to thank the Hamad Medical Corporation for their support and ethical approval (ref: RP#7100/07).
References
- Maconi G, Tosetti, Stanghellini V, Blanchi PG, Cori-naldesi R. Dyspeptic symptoms in primary care,an Observational study in general practice, Eur J Gastro-enterol Hepatol, 2002; 14: 985-990.
- Agreus L. Natural history of dyspepsia, Gut, 2002; 50: 2-9.
- Talley N, Boyce P, Jones M. Identification of upper and lower gastrointestinal symptom groupings in an urban population, Gut, 1998; 42:690-695.
- Mussel M, Kroenke K, Spitzer RL, Williams JBW, Herzog W, Lowe B. Gastrointestinal symptoms in primary care: Prevalence and association with depres-sion and anxiety. Journal of Psychomatic Research, 2008; 64:605-612.
- HeneGouwen GPVB. Present position of Gastroen-terology in the Netherlands, Gut, 1994; 35:1326-1327.
- Bener A, Ghuloum S, Burgut FT. Gender Differences in Prevalence of Somatoform Disorders in Patients Visiting Primary Care Centers. Journal of Primary Care & Community Health, 2009; 1(1):37-42.
- The link between anxiety and physical illness. Acces-sible at www.health.harvard.edu/health beat/HEALTH beat_080508.htm
- Van Oijen MG, Jose Mandere DF, Laheiji RJ, Van Rossum LG, Tan AC, Jansen JB. Gastrointestinal dis-orders and symptoms: does body mass index matter? Neth J Med, 2006;64:45-49.
- Bener A, Gholoum S, Abou-Saleh, MT. Prevalence, Symptom Pattern and Co-morbidity of Anxiety and Depressive Disorders in Primary Care in Qatar. So-cial Psychiatry and Psychiatric Epidemiology 2011 Feb. (In the Press).
- Cassano P, Fava M. Depression and Public Health: an overview, J Psychosom Res, 2002; 53:849-857.
- Ghuloum S, Bener A, Burgut FT. Epidemiological Survey of Knowledge, Attitude and Health Literacy concerning Mental Illness in a National Community Sample: A Global Burden Disease. Journal of Pri-mary Care and Community Health, 2010a.; 1(2) 111-118.
- Ghuloum S, Bener A, Burgut FT. Ethnic Differences in Satisfaction with Mental Health Services among Psychiatry Patients. The Open Psychiatry Journal, 2010b; 4: 19-24.
- Kroenke K, Spitzer RL, Williams JB, et al. Physical symptoms in primary care. Predictors of psychiatric disorders and functional impairment. Arch Fam Med 1994; 3:774-779.
- Jackson JL, O'Malley PG, Kroenke K. Clinical pre-dictors of mental disorders among medical outpa-tients. Validation of the “S4” model. Psychosomatics 1998; 39: 431–436.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9. Validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606-613.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disor-der: the GAD-7, Arch Intern Med 2006; 166:1092–1097.
- Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to Gastrointestinal symptoms in the general population, Scandinavian Journal of Gas-troenterology, 2002; 37: 294-298.
- Ronkainen J, Aro P, Storskrubb T et al, Gastro-esophagal reflux symptoms and health related quality of life in the adult general population – The Kalix-anda study, Aliment Pharmacol Ther, 2006; 23:1725-1733.
- Walker EA, Katon WJ, Jemelka RP, Roy-Bryne PP, Co-morbidity of gastrointestinal complaints, depres-sion, and anxiety in the Epidemiologic Catchment Area (ECA) study, AM J Med, 1992; 24:92:26-36.
- Irritable Bowel Syndrome. www.uptodate.com/patients/content/topic (accessed on 23/5/2010).
- Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC, Functional bowel disor-ders, Gastroenterology, 2006;136:1480-1491.
- Vankerkhoren LAS, Elikendal T, Laheij RJF, Van Oijen MGH, Jansen JBM. GI symptoms are still common in a general western population, Netherland Journal of Medicine, 2008; 66(1): 18-22.
- Creed F. The relationship between psychosocial pa-rameters and outcome in irritable bowel syndrome, AM J Med, 1999;107:745-805.
- Heading RC, Prevalence of upper gastrointestinal symptoms in the general population: A Systematic Review, Scandinavian Journal of Gastroenterology, 1999; 34: 3 -8.
- Creed F, Olden KW. Gastrointestinal disorders. In: Levenson JL, ed. American Psychiatric Publishing Textbook of Psychosomatic Medicine, Washington, DC: American Psychiatry Publishing: 2005:465-482.
- Locke GR, Weaver AL, Melton J, Talley NJ. Psycho-social factors are linked to Functional Gastrointestinal Disorders: A population-based case control study, The American Journal of Gastroenterology, 2004; 99(2): 350-357.
- Alander T, Svardsudd K, Johansson SE, Agreus L, Psychological illness is commonly associated with functional gastrointestinal disorders and is important to consider during patient consultation: a population based study, BMC Med, 2005; 3: 8.
- Bener A, Al-Hamaq AOAA, Dafeeah E. High preva-lence of depression anxiety and stress disorder among type 2 diabetes mellitus patients. The Open Psychia-try J 2011 (in press).