Research Article - Biomedical Research (2018) Volume 29, Issue 2
Imaging diagnosis of gallbladder adenoma
Yuanxi Jian, Li Zhu, Lei Han, Yiyuan Xing, Facheng Lu, Siying Wu and Jiaping Wang*
Department of Radiology, the Second Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, PR China
- *Corresponding Author:
- Jiaping Wang
Department of Radiology
The Second Affiliated Hospital of Kunming Medical University, PR China
Accepted date: October 27, 2017
DOI: 10.4066/biomedicalresearch.29-17-3166
Visit for more related articles at Biomedical ResearchAbstract
Recent studies have shown that the gallbladder adenomas belong to precancerous lesions, with possible malignant transformation, and imaging examination is the first choice for the diagnosis. The study was involved in the diagnosis of gallbladder adenoma commonalities by ultrasound, CT and MRI in characterization of do retrospective analysis in order to improve the accuracy. 32 cases of hospitalized patients with the diagnosis of gallbladder adenoma were collected. The 32 patients were retrospectively analyzed by ultrasound, CT and MRI images to find its generality characteristic imaging. B ultrasonic echo showed that the diameter of the malignant papillary adenoma increased in 18 cases of cystic papillary adenoma; CT showed that adenoma internal density was uniform and CT values continue to rise; MRI in common displayed for contour shadow equally. The benign lesions were wide and the malignant lesions were narrow. Portal phase lesions around was continuous reinforced obviously and the central displayed slightly lower density area. In the 14 cases of gallbladder tubular papillary adenoma, ultrasound showed that medium echoes, and commonness CT in enhanced arterial phase, portal phase and delay lesions was progressively light-moderate strengthened. MRI was performed for single nodule “cauliflower” shaped surface and signal shadow, and high signal stove, borders, “cauliflower” shaped surface was tested on the malignant nodules. Imaging diagnostic methods can improve the detection rate of gallbladder adenoma and reduce missed diagnosis.
Keywords
The gallbladder adenoma, Ultrasound, Computed tomography, Magnetic resonance imaging
Introduction
Gallbladder adenoma (AG) is a clinical common gallbladder benign tumor, and includes papillary adenoma, tubular adenoma and tubular papillary adenoma [1-3]. Studies have shown that the gallbladder adenomas belong to precancerous lesions, and the rate is about 10%~15% [4,5]. Studies have found that adenoma is multiple with the diameter greater than 1 cm is risk combined with gallstones or adenoma [6,7]. Whether the clinical for gallbladder adenoma underwent surgical treatment of diagnosis is given priority to imaging diagnosis. The study was involved in the diagnosis of gallbladder adenoma in our hospital by ultrasound, CT and MRI to discuss the characteristic of gallbladder adenoma imaging performance in order to improve the detection rate of gallbladder adenoma and reduce missed diagnosis.
Materials and Methods
Patients with general information
Thirty two (32) cases of hospitalized patients with the diagnosis of gallbladder adenoma in the second affiliated hospital of Kunming medical university in the phrase of June 2012 to June 2015 were collected: 19 cases of male, aged 42~67, an average old of 52.6 ± 1.9 years, average course of 4 years; 13 cases of female, age 47~65, an average old of 49.3 ± 2.4 years, average duration of 4.5 years. Major clinical symptoms and signs: 23 patients had repeated right epigastric discomfort, intermittent pain of right humeral back radiation with the right course of 1~6 years. 32 patients were recurrent right upper quadrant and xiphoid process under pain, tenderness, 19 cases showed the Murphy signs, and 2 cases with obstructive jaundice. 19 patients in the process of disease were with fever, chills, vomiting, nausea and gastrointestinal symptoms. 9 cases were combined gallstones, 3 cases were secondary acute pancreatitis, 1 case was with the gallbladder bile duct carcinoma.
The study protocol was approved by the Research Ethics Committee of the second affiliated hospital of Kunming medical university, and all patients gave their informed consent before study commencement.
Pathological diagnosis
Thirty two (32) patients with gallbladder adenoma are open or minimally invasive surgical for the removal of the gallbladder. Postoperative pathological results showed that 18 cases were cystic papillary adenoma, accounting for 56.25% of all patients: 11 cases of men and women in 7 cases, aged 52-66, an average of 62.3 ± 2.2 years old. Pathological results showed that 14 cases were gallbladder tubular papillary adenoma, accounting for 43.75% of all patients: 8 cases of male, female 6 cases, aged 48 to 63, an average of 50.6 ± 2.7 years old.
Instrument and the methods
Ultrasound: GE Logiq 9 ultrasonic diagnostic instrument, broadband convex array probe, center frequency of 3.5 MHz. Patients were fast for more than six hours, and the shape, number of lesions and echo, and the size of the lesions were measured by the conventional ultrasonic method and color doppler flow imaging (of a CDFI) was used to observe the pathological changes in blood flow. CT: CT examination was tested by dual-source CT 64 layer (SOMATOM Definition Definition) scans.
Patients in calm with fast for more than six hours were scanned from the diaphragmatic top to 2 edge of lumbar vertebral body. After routine scan, using high pressure injector by the elbow vein injection at a rate of 3 ml/s injected 300 mg/ml nonionic iodine contrast agent 80 ml to scan twice (bai arterial pulse period). Scanning: 120 kv, Eff. MAs230; Pitch of 0.8, the detector collimating 64 × 0.6 mm, gathering matrix 512 × 512, FOV310~338 mm. Conventional image layer 5 mm, thickness 5 mm.
MRI: GE Signa Infinity Twinspeed 1.5 T superconducting MRI imaging system. The areas of scan cover gallbladder bile duct area. Using 8 channel phased array body coils. Check sequence including: (1) the horizontal axis a fiesta T2WI fat suppression sequence, 6 mm thickness, 2 mm intervals, TR6000 ms, TE85 ms, 320 × 220, matrix FOV38 cm, NEX2 times, 62.5 kHz bandwidth; (2) 2 d fiesta coronary fat suppression sequence with a thickness 5 mm, interval 1 mm, TR 3.6 ms, TE1.6 ms, turning angle 60°, matrix 192 × 224, FOV35 cm, NEX1, 83.3 kHz bandwidth; (3) MRCP, SSFSE fat suppression sequence, the layer thickness of 50 mm, TR5000 ms, TE 1186 ms, matrix 320 × 288, FOV32 cm, bandwidth of 31.25 kHz. MRI of 32 patients was analyzed by the two experienced radiologists MRI in the diagnosis of physicians (subtropical high above the title). The evaluation contents were included lesion at the bottom of the neck, body, and the size (the size of the lesion with maximum diameter), the number of signals, edge, shape, basal, and whether with gallstones. Quantity is divided into single and multiple lesions. Compared with the muscle signal tree, above the muscle signals and close to the cerebrospinal fluid were considered for high signal, and below the muscle signal and close to the bone cortex were considered for the low signal, and below the muscle but higher than that of bone cortex signal were considered for the equally low signal. The lesions displayed edge smooth, coarse, leaf, shape classification rounded, irregular shape, base narrow base, wide base (lesions basal width<maximum diameter for narrow base, vice for wide base).
Statistical analysis
All measurement data were presented by ͞x ± S. SPSS 19.0 statistical software was used for statistical analysis. Data between multiple groups was used by the two samples of inspection. P<0.05 was considered the statistically significant difference.
Results
Imaging of cystic papillary adenoma
Ultrasound is the preferred way with the characteristics of noninvasive and economic for the check of gallbladder, and also is the screening examination way of the gallbladder adenoma at the beginning. 18 patients with lesions were characterized by clumps of medium echo, papillary. The smallest diameter was 0.7, the maximum diameter was 3.9 cm and the average diameter was (1.25+0.44) cm, the diameter of 5 cases were higher than 1.0 cm. Single lesion in 16 cases of 18 patients (13 cases by pathological diagnosis of benign and malignant in 3 cases), 2 cases of multiple lesions (by pathological diagnosis were malignant). 5 cases of malignant lesions on average (3.12-0.9) cm diameter (2.4~3.7 cm), the diameter in the lesions of the malignant group is bigger than the size of benign group (P<0.05).
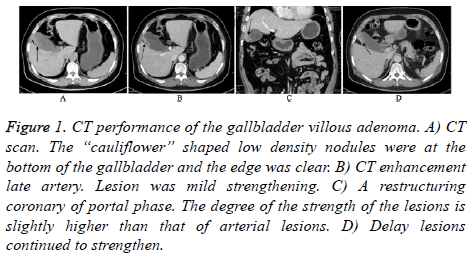
CT is the most mature of the imaging examination method for the gallbladder disease, because it can show the size morphology, and boundary of the gallbladder adenoma. 18 cases of cystic papillary adenoma: 14 cases of adenoma located in the body, 2 cases of gallbladder located at the bottom, 2 cases of gallbladder located at neck of gallbladder. All patients were papillary adenoma form and uniform internal adenoma density with the scan CT value of 32~48 Hu. No bleeding in the adenoma, calcification and cystic lesion, and the boundaries of lesion were clear. After the enhancement, it was obviously enhanced in arterial phase of lesions and the CT values were continue to rise with the 67~67 Hu in arterial phase and the CT value of 79~132 Hu in portal period. There were annular thickening of gallbladder wall with the structural integrity. It was uniformly mild or moderate reinforced after enhanced scan and the boundaries of lesion were clear. The average size of 5 cases of malignant lesions was 32.0 mm × 14.0 mm. Moderate enhancement was in the arterial lesions after enhanced scanning, and it was obviously reinforced around the lesions in portal phase, and slightly lower density area was in the central. Tumor and adjacent to the gallbladder was irregular thickening, and transverse, sagittal and/or coronary in patients showed that tumor was adhesion with gallbladder wall and the dividing line is not clear (Figure 1).
Figure 1: CT performance of the gallbladder villous adenoma. A) CT scan. The “cauliflower” shaped low density nodules were at the bottom of the gallbladder and the edge was clear. B) CT enhancement late artery. Lesion was mild strengthening. C) A restructuring coronary of portal phase. The degree of the strength of the lesions is slightly higher than that of arterial lesions. D) Delay lesions continued to strengthen.
MRI showed that the maximum diameter of lesions in 18 patients with cystic papillary adenoma was 3.86 cm, and the minimum was 0.71 cm in diameter, and the average diameter was (1.24+0.48) cm with the diameter of >1 cm were 5 cases. 18 cases of cystic papillary adenoma: 14 cases of adenoma located in the body, 2 cases of adenoma located at the bottom, 2 cases of adenoma located at neck of gallbladder. 16 cases of single lesion and the rest 2 cases of multiple lesions were in the 18 patients. The shape of lesions was similar to round in 12 cases and was irregular shape in 6 cases. The edges of lesions were smooth in 16 cases, were coarse in 2 cases, and were with lobulated in 12 cases. 14 cases of T2 WI has high signal shadow (13 cases of benign lesions, 1 case of malignant lesions), and these cases were accounted for 77.7% of 18 cases of cystic papillary adenoma with 4 cases of lesions in such as the equal signal (all of them are benign lesions). 16 cases of wide base18 cases of lesions, which were accounted for 88.9% (including 1 cases of benign lesions, and the rest for malignant lesions), and the rest 2 cases of lesions were in narrow base (both for malignant lesions).
Imaging diagnosis of the gallbladder tubular papillary adenoma
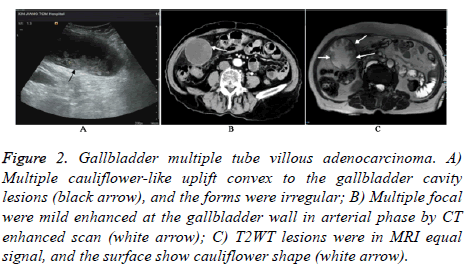
Ultrasound showed that 14 patients with gallbladder tubular papillary adenoma lesions were characterized by patches of medium echo, papillary. The maximum diameter of lesions in 14 patients was 3.4 cm, and the minimum was 0.6 cm in diameter, and the average was (1.15+0.27) cm. There were 3 cases with the diameter of lesions >1.0 cm. 13 cases of single lesion were in 14 patients (12 cases of benign and 1 case of malignant by pathological diagnosis), and 1 case of multiple lesion (with the pathological diagnosis of malignant). 2 cases of malignant lesions were characterized by single or multiple cauliflower-like apophysis lesions convex to the gallbladder cavity. Its average diameter was (3.42+0.7) cm (2.7~3.8 cm), and the diameter of lesions in the malignant group is bigger than the size of the benign group (P<0.05) (Figure 2).
Figure 2: Gallbladder multiple tube villous adenocarcinoma. A) Multiple cauliflower-like uplift convex to the gallbladder cavity lesions (black arrow), and the forms were irregular; B) Multiple focal were mild enhanced at the gallbladder wall in arterial phase by CT enhanced scan (white arrow); C) T2WT lesions were in MRI equal signal, and the surface show cauliflower shape (white arrow).
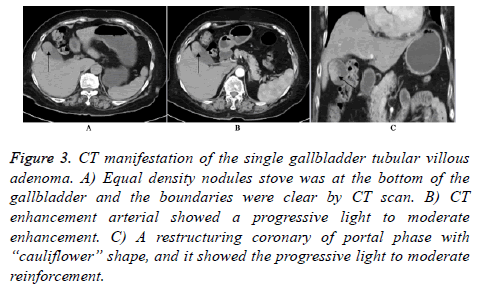
The internal image of 13 cases of single benign tubular papillary adenoma was uniform density. The scan CT value was 34~42 Hu, and there was no bleeding in the benign tubular papillary adenoma, calcification and cystic lesion, and the boundaries of lesions were clear. The lesions in the arterial, portal and delay phase were progressively light-moderate strengthening. CT values in portal vein phase were continue to rise with of 65~87 Hu in the arterial phase and the CT value of 83~127 Hu in portal period. 1 case of multiple tubular papillary adenoma showed that multiple focal arterial gallbladder wall was mild enhancement, enhanced CT in arterial phase, portal phase, and the delay lesions was progressively light-moderate strengthening. The clearance fat around bile duct was clear, and intrahepatic bile ducts were mild expansion (Figure 3).
Figure 3: CT manifestation of the single gallbladder tubular villous adenoma. A) Equal density nodules stove was at the bottom of the gallbladder and the boundaries were clear by CT scan. B) CT enhancement arterial showed a progressive light to moderate enhancement. C) A restructuring coronary of portal phase with “cauliflower” shape, and it showed the progressive light to moderate reinforcement.
MRI showed that the maximum diameter of lesions in gallbladder tubular papillary adenoma in 14 patients was 3.46 cm, and the minimum was 0.71 cm in diameter, and the average diameter was (1.24+0.48) cm with the diameter of >1 cm were 3 cases. 14 cases with gallbladder tubular papillary adenoma: 11 cases of adenoma located in the body, 2 cases of adenoma located at the bottom, 1 case of adenoma located at neck of gallbladder. 17 cases of single lesion and the rest 1 cases of multiple lesions were in the 18 patients. The shape of lesions was similar to round in 12 cases and was irregular shape in 6 cases. The edges of lesions were smooth in 16 cases, were coarse in 2 cases, and were with lobulated in 12 cases. Single nodules T2WI lesions has equal signal and the surface was shaped with “cauliflower”; Multiple focal nodular has the slightly high signal and the surface was shaped with “cauliflower”.
Discussion
Gallbladder adenoma is single, and often found in the body of middle-aged and old women. Tumors are usually discovered in the surgical of removal of the gall bladder stones or chronic cholecystitis by chance [8,9]. 32 cases of accounted for about 1.2% surgically resected specimens of 2672 cases of gallbladder the same period, which were close to the literature. Gallbladder adenoma was similar to other polypoid lesions in the gallbladder polypoid lesions (cholesterol, adenomatous and inflammatory) in clinical and ultrasound on the morphology. The incidence of gallbladder adenoma was accounted for only 4% [10]. Gallbladder adenoma itself exhibited no clinical symptoms, and the symptoms were mainly induced by cholecystitis, cholelith disease. About 1/3 to 3/5 of the gallbladder adenoma was accompanying with gallbladder stone [11-13]. The form of gallbladder adenoma was larger, multiple, and can cause a series of clinical symptoms [14]. Adenoma which was located at the neck of gallbladder can cause gallbladder obstruction and cholecystitis. The diameter of the most gallbladder adenoma was <15.0 mm or 20.0 mm [15-17], it was originated in body or bottom of the gallbladder with soft texture. It can be single and multiple. The surface showed granular or cauliflower shape. Study found that the transition of the gallbladder adenomas to adenocarcinoma is the usual way of gallbladder. The increased rate of carcinoma progression was related with the tumor size and the number of the nipple structure within the tumor [6,18]. Clinical research in abroad found [19,20]: (1) The transition of the gallbladder adenomas to gallbladder was with histological evidence. (2) Adenoma tissue was along with almost all of the growth of carcinoma in situ. (3) The incidence of the residual gland cancer is higher in invasive cancer. (4) The degree of deterioration was accompanied with the increase of adenoma. (5) The gallbladder adenoma progression rate also will increase as the growth of the age. (6) Gender factors play an important role in the gallbladder adenoma progression. Therefore early detection is the precondition for the treatment of malignant gallbladder adenoma. The preoperative diagnosis of gallbladder adenoma relies on imaging technologies, including ultrasound, CT and MRI. The differential diagnosis of suspected cases by imaging means to early detection of malignant gallbladder adenoma, differential diagnosis gallbladder adenoma and gallbladder (lumen or nodules) identification: gallbladder occurs in women, and the onset age is similar to the gallbladder adenoma. CT of the nodules or gallbladder cavity manifested that it was mainly for gall bladder lumen nodular or lobulated lesions, and the infiltration of mass base to the gallbladder wall. Advanced gallbladder was often accompanied by infringing upon the surrounding tissues and organs, including liver metastasis or distant metastasis with the swollen lymph nodes around the gallbladder and common bile duct. When the gallbladder adenoma >10.0 mm, uniform tumor reinforcement and low density area, and thickening of gallbladder wall, it maybe the gallbladder or gallbladder adenoma with malignant transformation. If the gallbladder adenomas <10.0 mm without clinical symptoms, gallstones, patients can conduct imaging regularly review [14,15]. Through the comparison of imaging data, the study put forward the imaging of the gallbladder adenoma (including ultrasound, CT and MRI) diagnosis characteristics to improve the diagnosis of gallbladder adenoma and reduce the misdiagnosis rate. The study also provides a new train of thought for clinical judgment whether surgery treatment or not.
Acknowledgment
This work was supported by Study on the application of basic science and technology project of Yunnan province (Kunming Medical joint special, No.2012FB045).
References
- Chlumská A, Waloschek T, Mukenšnabl P, Martínek P, Kašpírková J, Zámečník M. Pyloric gland adenoma: a histologic, immunohistochemical and molecular genetic study of 23 cases. Cesk Patol 2015; 51: 137-143.
- Hong SN, Lee TY, Yun SC. The risk of colorectal neoplasia in patients with gallbladder diseases. J Korean Med Sci 2015; 30: 1288-1294.
- Lange J, Bachmann R, Königsrainer A, Zdichavsky M. Appendiceal diverticulitis shortly after a performed laparoscopic sigma resection. J Surg Case Rep 2015.
- Akbulut S, Karagul S, Ertugrul I, Aydin C, Yilmaz M, Yilmaz S. Histopathologic findings of cholecystectomy specimens in patients who underwent donor hepatectomy for living donor liver transplantation. Transplant Proc 2015; 47: 1466-1468.
- Rubio CA. Serrated adenoma of the gallbladder: a case report. Anticancer Res 2015; 35: 3485-3487.
- Gönen AN, Özkan Z, Emir S, Sarıcık B, Cihangiroğlu G, Yazar FM, Kanat BH. Villous adenoma in gallbladder volvulus: A rare coincidence. Turk J Gastroenterol 2014; 25: 308-309.
- Köseoğlu RD, Özkan N, Barut Ş, Markoç F. Pyloric gland type adenoma including intramucosal carcinoma focus of gallbladder. Turk J Gastroenterol 2014; 25: 234-236.
- Sun LP, Guo LH, Xu HX, Liu LN, Xu JM, Zhang YF, Liu C, Bo XW, Xu XH. Value of contrast-enhanced ultrasound in the differential diagnosis between gallbladder adenoma and gallbladder adenoma canceration. Int J Clin Exp Med 2015; 8: 1115-1121.
- Jeun JW, Cha JM, Lee JI, Joo KR, Shin HP, Lim JU. Association of gallbladder polyp with the risk of colorectal adenoma. Intest Res 2014; 12: 48-52.
- Mori Y, Sato N, Matayoshi N, Tamura T, Minagawa N, Shibao K, Higure A, Nakamoto M, Taguchi M, Yamaguchi K. Rare combination of familial adenomatous polyposis and gallbladder polyps. World J Gastroenterol 2014; 20: 17661-17665.
- You Y, Bui K, Bui MM, Malafa M, Coppola D. Histopathological and immunophenotypical features of intestinal-type adenocarcinoma of the gallbladder and its precursors. Cancer Control 2014; 21: 247-250.
- Acharya V, Ngai J, Whitelaw D, Motallebzadeh R. Primary gallbladder lymphoma presenting as a polyp. BMJ Case Rep 2014.
- Solaini L, Sharma A, Watt J, Iosifidou S, Chin Aleong JA, Kocher HM. Predictive factors for incidental gallbladder dysplasia and carcinoma. J Surg Res 2014; 189: 17-21.
- Matłok M, Migaczewski M, Major P, Pędziwiatr M, Budzyński P, Winiarski M, Ostachowski M, Budzyński A, Rembiasz K. Laparoscopic cholecystectomy in the treatment of gallbladder polypoid lesions-15 years of experience. Pol Przegl Chir 2013; 85: 625-629.
- Kim K, Kim DH, Chae SW, Shin JH, Kim HJ, Do SI, Lee HJ, Koo JH, Pyo JS, Sohn JH. Expression of cell cycle-related proteins, p16, p53 and p63 as important prognostic markers in gallbladder adenocarcinoma. Pathol Oncol Res 2014; 20: 409-415.
- Yamamoto K, Yamamoto F, Maeda A, Igimi H, Yamamoto M, Yamaguchi R, Yamashita Y. Tubulopapillary adenoma of the gallbladder accompanied by bile duct tumor thrombus. World J Gastroenterol 2014; 20: 8736-8739.
- Fei X, Lu WP, Luo YK, Xu JH, Li YM, Shi HY, Jiao ZY, Li HT. Contrast-enhanced ultrasound may distinguish gallbladder adenoma from cholesterol polyps: a prospective case-control study. Abdom Imaging 2015; 40: 2355-2363.
- Yuan HX, Cao JY, Kong WT, Xia HS, Wang X, Wang WP. Contrast-enhanced ultrasound in diagnosis of gallbladder adenoma. Hepatobiliary Pancreat Dis Int 2015; 14: 201-207.
- Xu Y, Yuan J, Chong V, Ding Z. Villous adenoma of gallbladder in a patient with systemic lupus erythematosus. J Res Med Sci 2012; 17: 811-813.
- Pai RK, Mojtahed K, Pai RK. Mutations in the RAS/RAF/MAP kinase pathway commonly occur in gallbladder adenomas but are uncommon ingallbladder adenocarcinomas. Appl Immunohistochem Mol Morphol 2011; 19: 133-140.