Case Report - Current Trends in Cardiology (2023) Volume 8, Issue 10
Holt-Oram syndrome: A case report.
Kamal Kant Jena*
Department of Cardiology, Government Stanley Medical College, Tamil Nadu, India
- Corresponding Author:
- Dr. Kamal Kant Jena
Department of Cardiology
Government Stanley Medical College
Tamil Nadu
India
Email: kamalkanth.jena92@gmail.com
Received: 15 December, 2020, Manuscript No. AACC-20-23363; Editor assigned: 18 December, 2020, PreQC No. AACC-20-23363 (PQ); Reviewed: 02 January, 2021, QC No. AACC-20-23363; Revised: 03 August, 2022, QI No. AACC-20-23363; Manuscript No. AACC-20-23363 (R); Published: 31 August, 2022, DOI: 10.35841/aacc-6.4.116.
Citation: Jena KK. Holt-Oram syndrome: A case report.Curr Trend Cardiol.2022;26(3):1-3.
Abstract
Holt-Oram Syndrome (HOS) also known as hand-heart syndrome is a very rare autosomal dominant disease caused by a mutation in the TBX5 gene located on chromosome 12. Clinically it manifests with morphological abnormalities of the upper limbs and congenital cardiac defects leading to variety of complications. Cardiac malformations go undiagnosed till late in life. With routine antenatal checkup, external physical deformities can be found out with high suspicion of congenital heart malformations as well, which can lead to early effective management. We here by describe a case of 20 year-old female with known morphological alterations of the upper limbs since birth presented with right heart failure diagnosed to have atrial septal defect.
Introduction
The congenital cardiac and upper limb deformities occurring together are known as heart-hand syndrome. The most common among them is HOS with incidence of 1 in 100,000 live births. It is an autosomal disorder occurring due to the mutation in chromosome 12q24.1, which codes for the human transcription factor TBX5 gene. Mary Clayton Holt and Samuel Oram in 1960 described HOS as a triad of ASD, Conduction disturbances and digital malformations. Our patient also has ASD along with left distal phocomelia and digital anomalies on both hands [1].
Case Report
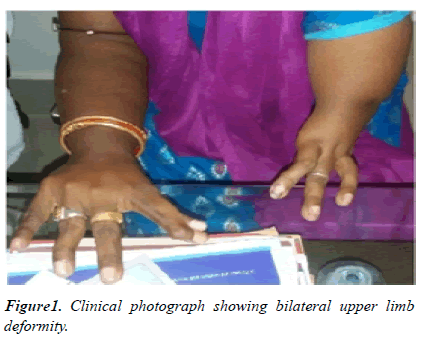
A 20-year-old girl was referred to the department of cardiology, with the history of dyspnea (NYHA grade 2) and palpitation for the past 1 year. Her past medical and family history was unremarkable. On musculoskeletal examination, she had obvious bilateral upper limb deformities.
The left upper limb was abnormally short with absent forearm and hand arising from the arm, which falls under type III distal phocomelia and with oligo-dactyly (Figure 1) [2].
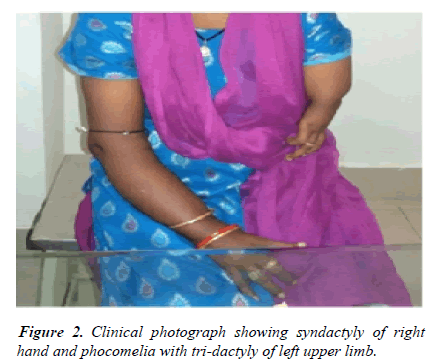
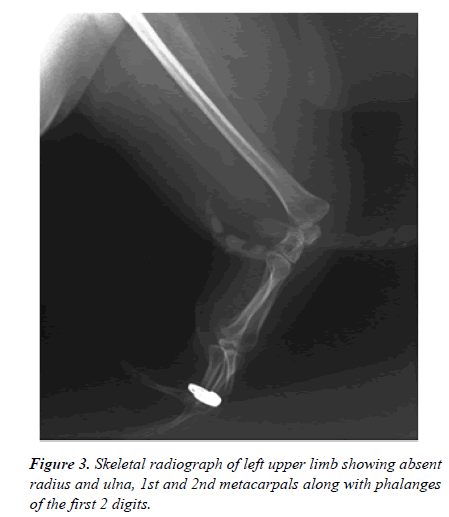
The right upper limb also had hypo plastic thumb with syndactyly of the thumb and index finger. Skeletal radiographs of the left upper limb depicted absent radius, ulna, 1st and 2nd metacarpals along with the phalanges of the first two digits. There were no obvious lower limbs or spine deformities (Figure 2) [3].
Physical examination revealed elevated Jugular venous pressure, blood pressure of 110 mmHg-70 mmHg, pulse rate of 96 beats/min and O2 saturation was 98% in room air on cardiovascular examination, right parasternal heave of grade 2 was present; auscultation revealed wide fixed split of the second heart sound with loud pulmonary component was noted along with ejection systolic murmur of grade III, best heard over the pulmonary area (Figure 3) [4].
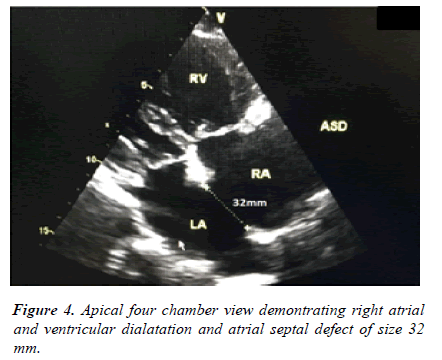
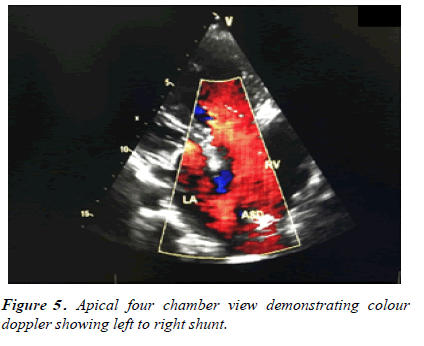
Electrocardiogram demonstrated normal sinus rhythm and right axis deviation with incomplete right bundle branch block. Chest X ray showed cardiomegaly due to right atrial and ventricular dilatation with dilated pulmonary trunk. Two-dimensional transthoracic echocardiography in four chamber view revealed a large ostium secundum type of ASD (32 mm) with left to right shunt, right atrial and ventricular dilatation, severe pulmonary artery hypertension (58 mmHg), and an left ventricular ejection fraction of 55%. Tricuspid Annular Plane Systolic Excursion (TAPSE) was 15 mm suggesting mild Right Ventricular (RV) systolic dysfunction (Figure 4) [5].
All other laboratory investigations were normal. Hence the diagnosis of HOS was formulated based on clinical, radiographic and echocardiographic evidence. She was stabilized with medical management (ACE inhibitors, diuretics and beta blocker) and referred to cardiovascular surgery for complete intracardiac repair with pericardial patch closure of the septal defect (Figure 5) [6].
Discussion
Holt Oram Syndrome (HOS) is an autosomal dominant disorder involving the deformities of the heart and upper limbs. The mutation is identified on chromosome 12q24.1 inactivating the TBX5 gene. As the mode of transmission is autosomal dominant, it is inherited from one generation to the other. Hence all the family members should be screened. But, in 85% of the affected cases there is a negative family history, indicating a de novo pathogenic variant. In suspected cases with positive family history, it can be detected antenatally by routine anomaly scan identifying upper limb deformities or by prenatal molecular testing of the TBX5 gene [7].
The cardinal feature of the syndrome is upper limb deformities. The lower limbs are spared as the mutant gene affects the embryonic differentiation during the 4th-5th week of gestation before the lower limbs have started to differentiate. The upper limb skeletal deformities can range from thumb hypoplasia, triphalangeal thumbs, absent carpel bones, absent radius or ulna to severe form like phocomelia. Although the deformities are bilateral, left side is affected more than the right. Our patient had left distal phocomelia with tridactyly and syndactyly of the right upper limbs [8].
The second major component is cardiac anomalies and the most common are atrial septal defects as in our patient. Approximately 60% are atrial septal defects (Ostium secundum type followed by ostium primum), the rest can be ventricular septal defects or complex congenital heart diseases. These cardiac lesions can cause early heart failure leading to poor prognosis; our patient also presented with heart failure. It is important to know that the degree of upper limb deformities does not correlate with the severity of cardiac anomaly. Electrocardiography shows subtle conduction disturbances to variable degree of atrio-ventricular block our patient also had incomplete right bundle branch block [9].
However, few other disorders can also present with cardiac and upper limb deformities like Thrombocytopenia Absent Radius Syndrome (TAR), fanconi anemia, roberts syndrome and thalidomide embryopathy. But the absence of hematological findings works in favor of HOS. The main aim of management is to provide functionality to the deformed upper limbs by physical therapy and early identification and surgical correction of the cardiac anomaly to prolong longevity [10].
Conclusion
In conclusion, we report a case of HOS associated with distal phocomelia and oligodactyly of left upper limb and syndactyly of the right hand along with ostium secundum type ASD in heart failure. Due to its high degree of cardiac complications and recent advancements in fetal echocardiogram, all patients with upper limb deformities in antenatal checkup should have cardiac evaluation with recent for early detection and effective management to have a better prognosis.
Funding
No financial support to disclose.
Conflict of Interest
The authors declare that there are no conflicts of interest.
References
- Brockhoff CJ, Kober H, Tsilimingas N, et al. Holt-Oram syndrome. Circulation. 1999;99(10):1395-6.
[Crossref] [Google Scholar] [PubMed]
- Basson CT, Bachinsky DR, Lin RC, et al. Mutations in human cause limb and cardiac malformation in Holt-Oram syndrome. Nat Gen. 1997;15(1):30-5.
[Crossref] [Google Scholar] [PubMed]
- Holt M, Oram S. Familial heart disease with skeletal malformations. Br Heart J. 1960;22(2):236.
[Crossref] [Google Scholar] [PubMed]
- Nourzad G, Baghershiroodi M. A case report on holt-oram syndrome (heart-hand). Atherosclerosis Risk Young Adult Atheroscler. 2011;7(2):87.
[Google Scholar] [PubMed]
- Hurst JA, Hall CM, Baraitser M. The Holt-Oram syndrome. J Med Gen. 1991;28(6):406-10.
[Crossref] [Google Scholar] [PubMed]
- Sletten LJ, Pierpont ME. Variation in severity of cardiac disease in Holt‐Oram syndrome. Am J Med Gen. 1996;65(2):128-32.
[Crossref] [Google Scholar] [PubMed]
- Shankar B, Bhutia E, Kumar D, et al. Holt-Oram syndrome: A rare variant. Iran J Med Sci. 2017;42(4):416.
[Google Scholar] [PubMed]
- Tidake A, Gangurde P, Shaikh Z, et al. Tetralogy of fallot with Holt-Oram syndrome: Case report and review. Cli Res Car. 2015;104(9):790-3.
[Crossref] [Google Scholar] [PubMed]
- Smith AT, Sack Jr GH, Taylor GJ. Holt-oram syndrome. J Pediatr. 1979;95(4):538-43.
[Crossref] [Google Scholar] [PubMed]
- Chin J, Pereira S, Camacho A, et al. Holt-Oram syndrome: A case report. Rev Port Cardiol. 2014;33(11):737-e1.
[Crossref] [Google Scholar] [PubMed]