Research Article - Biomedical Research (2017) Volume 28, Issue 9
Hepatocyte growth factor shows benefits for patients with chronic renal failure induced type 2 diabetes
Gan Yu1, Zhou Hui Hua2*, Zhang Li2 and Li Tong Wei31Department of Physical Examination, Hongqi Hospital of Mudanjiang Medical University, Mudanjiang, China
2Department of Scientific Research, Hongqi Hospital of Mudanjiang Medical University, Mudanjiang, China
3Labor Union, Hongqi Hospital of Mudanjiang Medical University, Mudanjiang, China
- *Corresponding Author:
- Zhou Hui Hua
Department of Scientific Research
Hongqi Hospital of Mudanjiang Medical University, China
Accepted on January 24, 2017
Abstract
Chronic renal failure patients receiving haemodialysis and continuous ambulatory peritoneal dialysis often encounter inflammation troubles during long-period treatment. Patients with type 2 diabetes induce different degree chronic renal failure and represent low quality of life. Type 2 diabetes may be one of the most important arch-criminal factors that aggravate syndrome and renal insufficiency. These impairments of kidney’s function may lead to chronic renal failure though disqualify of cellular activities. Hepatocyte Growth Factor (HGF) is one of the most extensive biological activity factors and presents multifunctional anti-fibrosis factor that plays a critical role in the progression of chronic renal failure. The purpose of this study was to investigate whether HGF treatment could decrease inflammation and improve chronic renal failure. Clinical investigations were performed in 138 (75 men and 63 women) chronic renal failure patients induced by type 2 diabetes with 98 healthy volunteers (51 men and 41 women) as control. Our experimental data showed that serum level of HGF and IL-6 were decreased and correlated with age and sex in patients with chronic renal failure induced by type 2 diabetes (r=0.864, r=0.743, respectively). Serum levels of IL-1, MCP-1 and TNF-α were increased compared between patients with severe renal failure and healthy volunteers (**P<0.01). HGF injection (MTD dose) improved the inflammatory factor expression levels for patients with chronic renal failure compared to placebo group. The most common treatment-emergence adverse events were hypertension and proteinuria. Taken together, level of HGF in serum was correlated with inflammation in chronic renal failure patients induced by type 2 diabetes, which presented beneficial outcomes through improvement of inflammatory factor expression in clinical.
Keywords
Hepatocyte growth factor, Chronic renal failure, Type 2 diabetes, Inflammation.
Introduction
Chronic renal failure is syndrome with serious metabolic disorders and other damage of a group of syndrome caused by a variety of chronic kidney disease [1]. Chronic renal failure is disease of chronic progressive renal parenchyma damage caused by a variety of reasons which leads to kidney obvious atrophy and irreversible damage of function [2]. The majorities of pathogenesis are glomerulonephritis, interstitial nephritis, high blood pressure, diabetes and obstructed kidney disease [3]. Currently, diabetes related chronic renal failure presented a raise trend in clinical investigation with the rapid increase of diabetes sufferers throughout the world [4,5]. Chronic renal failure induced by diabetes mellitus that significantly affects patients’ quality of life [6]. Therefore, it is vital to explore new horizon for diagnosis and treatment of chronic renal failure patients induced by type 2 diabetes.
Inflammatory cytokines, such as TNF-α, IL-1, IL-8, and IL-10 are the most common characteristics for patients with chronic renal failure [7-9]. Inflammation in patients with type 2 diabetes is related to dysfunction of urinary albumin excretion, endothelial function and cellular metabolism [10]. Long-term hypertension contributes to kidney damage and slowly develops chronic renal failure for patients with type 2 diabetes [11]. In addition, previous study has reported that inhibition of the renin-angiotensin system exerted potent decreasing blood pressure by reducing vascular inflammation [12]. However, long-term medication of anti-hypertension drug, Fimasartan, also leads to decline of renal function and even causes chronic renal failure in patients with type 2 diabetes [13].
Hepatocyte Growth Factor (HGF) is produced by mesenchymal cells during organ injury [14]. HGF is one of the most extensive a biological activity factor and presents multifunctional anti-fibrosis factor that plays a critical in kidney development, acute injury and regeneration, which is activated by proteolytic cleavage at the site of injury and results in a biological HGF protein [15]. Biologically active HGF suppresses fibrosis and molecular basis for HGF-mediated regression of renal fibrosis was elaborated in previous report [16,17]. Notably, plasma concentration of HGF exhibited decreasing trend in patients with type 2 diabetes, who may be regulated other inflammatory factor expression levels [18]. Therefore, HGF may be regarded as a local acute phase protein with chronic renal failure.
The purpose of this study was to investigate whether the expression and function of HGF was decreased and associated with inflammation in patients chronic renal failure induced by type 2 diabetes. HGF treatment improves inflammatory cytokines for patients with chronic renal failure induced by type 2 diabetes. These clinical data provided significant reference for doctors and clinicians in treatment of patients with chronic renal failure induced by type 2 diabetes.
Materials and Method
Ethics statement
Research protocols were approved by the University Ethical Committee of Zhujiang Hospital, Southern Medical University and Committee of The Academic Medical Center in China (20150618521). All subjects (patients and volunteers) gave written consent in this clinical investigation.
Patients
138 (75 men and 63 women) chronic renal failure in patients with type 2 diabetes and 98 healthy volunteers (51 men and 47 women) were enrolled into investigated IL-1, IL-8, IL-10, HGF, MCP-1 and IL-6 serum concentration levels and their correlations with patients’ age and gender. All patients and volunteers were divided into three groups (18-30, 30-45 and 45-64 years old) according patients’ and volunteers’ age after giving the informed consent. Mean age of the volunteers and patients was 41 ± 21 and 41 ± 23 years, respectively. Mean value of kt/V was equal 1.1 ± 0.2 and mean value of the Glomerular Filtration rate (GFT) was 7.2 ± 2.9 ml/min in patients with chronic renal failure and Type 2 diabetes. Mean of blood glucose was 7.2 ± 3.3 mmol/l and the mean of blood pressure was 153 ± 32 mm Hg in patients with chronic renal failure and Type 2 diabetes.
Enzyme linked immunosorbent assay (ELISA)
In the protein expression assay, TNF-α, IL-1, IL-8, IL-10, HGF, MCP-1 and IL-6 proteins ELISA kits (R&D, Bio-Techne China Co. Ltd, USA) were used to determine serum concentration levels of the TNF-α, IL-1, IL-8, IL-10, HGF, MCP-1 and IL-6, respectively. The operating steps were conducted according to the manufacturer’s instructions. The final results were recorded at 450 nm on an ELISA plate reader.
Study design
The double-blind study was carried out in 3 phases: baseline stage, the double-blind treatment phase (4-week dose-titration treatment) and 4-week post-treatment for patients with chronic renal failure induced by type 2 diabetes who volunteered to continue to complete the ongoing extension study. Patients were randomized to once every three days, double-blind treatment with HGF or placebo treatment. Patients with chronic renal failure induced by type 2 diabetes continued treatment with the dose of HGF (5 mg/kg) or placebo to achieve the final investigation throughout the maintenance period (52 weeks).
Outcomes measures
Renal function tests were used for assessing the function of patients with chronic renal failure induced by type 2 diabetes. Clinical chronic renal failure scores were evaluated descripted in previous study [19]. The date was recorded and calculated the degree of chronic renal failure.
Efficacy and safety assessments
Efficacy assessments including the median percent reduction scores and response rate were analysed in patients with knee osteoarthritis from baseline during the 4-week and double-blind period in the presence of HGF (5 mg/kg) or placebo. In addition, the overall safety and pharmacokinetic analysis were conducted according to previous clinical studies [20,21]. Furthermore, the safety assessments of the most frequent treatment-emergent adverse events were evaluated in all randomized patients who received the study drug and had at least one post-dose safety assessment. Dose-responses analysis was conducted when the last dose drugs injection.
Glomerular filtration rate
Glomerular filtration rate in patients with chronic renal failure induced by type 2 diabetes and healthy volunteers were analysed by Gates Method (BioPAL offers FIT-GFR™. The procedures were performed according to the manufacturer’s instructions. The final results were recorded at 450 nm on an ELISA plate reader.
Analysis of blood glucose and blood pressure
Blood glucose in patients with chronic renal failure induced by type 2 diabetes and healthy volunteers was detected by glucometer (Sifsof Global Trade, USA). Blood pressure was recorded by electronic sphygmomanometer.
Statistical analysis
All data were reported as means and SEM. Statistical significance of differences between mean values was assessed by Student’s t test for unpaired data. Comparisons of data between multiple groups were performed with Analysis of Variance (ANOVA). Continuous variables were reported as mean and 95% Confidence Interval (CI). Treatment effect is presented as median reduction in knee osteoarthritis over the treatment period. Robust nonparametric Hodges-Lehmann estimates of median drugs treatment effects and 95% confidence interval are provided. Responder rates and treatment-emergent adverse events were analysed by χ2 test. P<0.05 was considered statistically significant.
Results
Characterizations of patients
A total of 138 chronic renal failure patients induced by type 2 diabetes (75 men and 63 women) and 98 healthy volunteers (51 men and 47 women) were enrolled for analysis in this study. The characteristics of the patient and healthy volunteer are summarized in Table 1. There were no sex significant difference in numbers both in patients and healthy volunteers. The mean blood pressure in chronic renal failure patients induced by type 2 diabetes was higher than healthy volunteers. Antihypertensive medications were not taken during the treatment period until the high pressure was more than 170 mm mercury column. In addition, the body weight in chronic renal failure patients induced by type 2 diabetes was significant lower than healthy volunteers. Furthermore, most of chronic renal failure patients induced by type 2 diabetes were needed to haemodialysis.
| Number of patients or parameters | % | |
|---|---|---|
| Patients | 138 | 100 |
| Male | 73 | 52.9 |
| Female | 65 | 47.1 |
| Age | 18-64 | 100 |
| 18-30 | 48 | 34.8 |
| 30-45 | 32 | 23.2 |
| 45-64 | 58 | 42 |
| Blood pressure | 153 ± 32 | 100 |
| Blood glucose | 7.2 ± 3.3 mmol/L | 100 |
| kt/V | 1.1 ± 0.2 | 100 |
| GFT | 7.2 ± 2.9 ml/min | 100 |
| Health volunteers | 98 | 100 |
| Male | 51 | 52 |
| Female | 47 | 48 |
| Age | 20-62 | 100 |
| 20-30 | 21 | 21.4 |
| 30-45 | 33 | 33.7 |
| 45-62 | 44 | 44.9 |
| Blood pressure | 93 ± 13 | 100 |
| Blood glucose | 4.4 ± 2.6 mmol/L | 100 |
| kt/V | 2.6 ± 0.6 | 100 |
| GFT | 13.6 ± 3.3 ml/min | 100 |
Table 1. Characterizations of chronic renal failure patients with Type II diabetes.
Analysis of HGF, TNF-α, MCP-1, IL-1 and IL-6 expression in serum
The serum levels from renal failure patients induced by type 2 diabetes and volunteers were used to analysis HGF, TNF-α, MCP-1, IL-1 and IL-6 expression. The analysis revealed mean serum level of HGF (-24%) and IL-6 (-11%) were decreased and correlated with age and sex in patients with chronic renal failure induced by type 2 diabetes (r=0.864, r=0.743, respectively). The patients and healthy volunteers were divided into three groups according to the age of research objects. The mean serum levels of IL-1, MCP-1 and TNF-α were increased compared between patients with severe renal failure and healthy volunteers (**P<0.01). TNF-α, MCP-1, HGF, IL-8, IL-10, IL-1 and IL-6 concentration changes were summarized in Table 2. This detection showed that serum concentration levels of IL-1, MCP-1 and TNF-α were increased in chronic renal failure patients induced by type 2 diabetes compared to healthy volunteers. There was no correlation between IL-1, MCP-1 and TNF-α expression and chronic renal failure patients induced by type 2 diabetes. Also, no significant change of serum IL-10 and IL-8 concentration was observed between patients and healthy volunteers in our cohort study.
| Inflammatory factors | Patients | Volunteers |
|---|---|---|
| IL-1 | 1.22 pg/ml | 0.36 pg/ml** |
| MCP-1 | 1.08 pg/ml | 0.40 pg/ml** |
| TNF-α | 0.94 pg/ml | 0.29 pg/ml** |
| IL-10 | 0.89 pg/ml | 0.31 pg/ml** |
| IL-8 | 1.14 pg/ml | 0.42 pg/ml** |
| IL-6 | 0.68 pg/ml | 1.42 pg/ml** |
| HGF | 0.35 pg/ml | 1.47 pg/ml** |
Table 2. Analysis of serum concentration levels of inflammatory factors in chronic renal failure patients with type II diabetes.
Correlation analysis of HGF
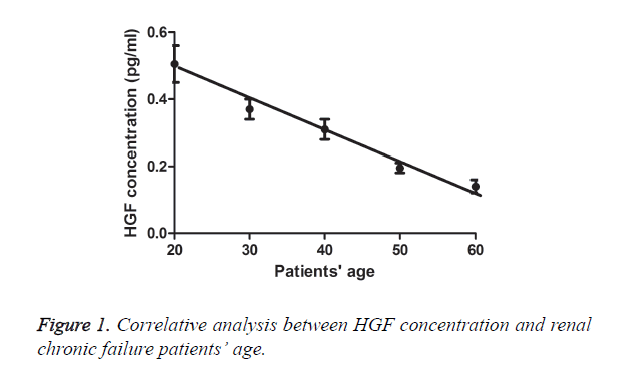
To study levels of HGF in serum correlate with chronic renal failure in patients, we analysed HGF serum concentration levels and correlation analysis with gender and age of chronic renal failure patients induced by type 2 diabetes. Statistical analysis in Table 2 showed that mean concentration of HGF in chronic renal failure in male patients induced by type 2 diabetes was 0.35 pg/ml (Inter Quartile Range, IQR: 0.18-0.52 pg/ml), and healthy male volunteers was 1.46 pg/ml (IQR: 0.59-2.32 pg/ml). However, concentration of HGF in chronic renal failure in female patients with Type 2 diabetes was 0.54 pg/ml (IQR: 0.28-1.04 pg/ml), and healthy female volunteers was 0.49 pg/ml (IQR: 0.32-0.76 pg/ml), which suggested that HGF concentration presented a positive correlation with gender. In addition, no difference between male and female patients in 45-64 years old groups was observed in this study (Table 3). Furthermore, 18-30 and 30-45 years old groups presented a higher serum concentration in male patients compared to female patients. The correlative analysis showed a positively relative between HGF concentration and patients’ age (Figure 1). Our date indicated that all chronic renal failure patients induced by type 2 diabetes were in condition of high blood pressure (Table 1).
| Male | Female | |
|---|---|---|
| Patients | 0.45 pg/ml | 0.23 pg/ml* |
| 18-30 | 0.64 pg/ml | 0.30 pg/ml* |
| 30-45 | 0.51 pg/ml | 0.24 pg/ml** |
| 45-64 | 0.15 pg/ml | 0.17 pg/ml |
| Volunteers | 1.26 pg/ml | 1.28 pg/ml |
| 20-30 | 1.28 pg/ml | 1.32 pg/ml |
| 30-45 | 1.18 pg/ml | 1.34 pg/ml |
| 45-62 | 1.32 pg/ml | 1.27 pg/ml |
Table 3. Correlation analysis of HGF serum concentration levels in chronic renal failure patients with type II diabetes.
Correlation analysis of IL-6
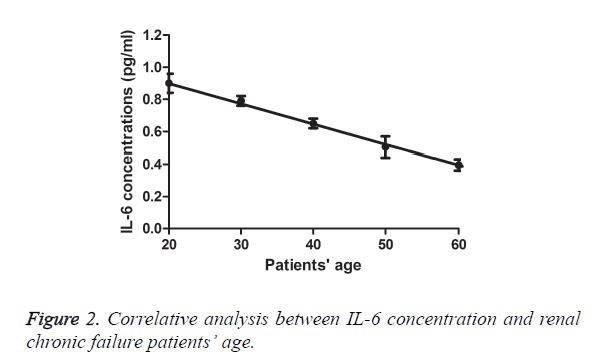
We also analysed serum concentration levels of IL-6 and correlation analysis with gender and age of chronic renal failure patients induced by type 2 diabetes. Statistical analysis in Table 4 showed that mean serum concentration level of IL-6 in chronic renal failure patients was 0.66 pg/ml (IQR: 0.39-1.22 pg/ml), and healthy male volunteers was 1.35 pg/ml (IQR: 0.78-1.72 pg/ml). And mean serum concentration level of IL-6 in chronic renal failure in female patients induced by type 2 diabetes was 0.89 pg/ml (IQR: 0.58-1.35 pg/ml), and healthy female volunteers was 1.47 pg/ml (IQR: 0.82-1.81 pg/ ml). With contrary to HGF, mean concentration of IL-6 were higher (IQR: 0.61-1.82 pg/ml) in 18-30 years old groups and its serum concentration levels were relative lower in 30-45 (IQR: 0.42-0.82 pg/ml) and 45-64 (IQR: 0.33-0.68 pg/ml) years old groups in patients (Figure 2). Date indicated that a positively relative between IL-6 serum concentration levels in chronic renal failure patients induced by type 2 diabetes. However, the correlation between IL-6 serum concentration levels with gender was not observed in this study. These date suggested that serum concentration level of IL-6 was decreased with aged older in chronic renal failure in male patients.
| Male | Female | |
|---|---|---|
| Patients | 0.66 pg/ml | 0.89 pg/ml* |
| 18-30 | 0.75 pg/ml | 1.14 pg/ml* |
| 30-45 | 0.52 pg/ml | 0.85 pg/ml* |
| 45-64 | 0.35 pg/ml | 0.57 pg/ml* |
| Volunteers | 1.35 pg/ml | 1.47 pg/ml |
| 20-30 | 1.57 pg/ml | 1.63 pg/ml |
| 30-45 | 1.48 pg/ml | 1.47 pg/ml |
| 45-62 | 1.24 pg/ml | 1.25 pg/ml |
Table 4. Correlation analysis of IL-6 serum concentration levels in chronic renal failure patients with type II diabetes.
Duration of treatment, dose-limiting toxicities, and maximum tolerated dose
Median overall duration of HGF treatment was eight weeks. Across all dosing cohorts were 1.0, 2.5, 5.0, 8.5, and 13.0 mg/kg. Our date in Table 5 showed that 13 mg/kg ml of HGF once every three days was identified as the Maximum Tolerated Dose (MTD) and 8.5 mg/kg of HGF once a week was identified as dose-limiting toxicity (DLT). The lowest-dose cohorts of HGF presented the fewest number of HGF dose reductions. We observed that the common treatment-emergent adverse events of HGF injection were hypertension, diarrhoea, rash, proteinuria, fatigue, and oedema peripheral. Most of patients with knee osteoarthritis required to reduce drug dose for cumulative toxicity after treatment with DLT dose. Therefore, most of patients were enrolled at a dose of 5.0 mg/kg of HGF to meet further clinical experiment of the tolerability and therapeutic effects for patients with chronic renal failure.
| Total (n=36) | 1.0-2.5 mg/kg (n=12) | 5.0-8.5 mg/kg (n=16) | 13.0 mg/kg (n=8) | |
|---|---|---|---|---|
| Adverse event | ||||
| Hypertension | 8 | 2 | 3 | 3 |
| Diarrhoea | 4 | 1 | 1 | 2 |
| Proteinuria | 7 | 1 | 3 | 3 |
| Rash | 4 | 0 | 2 | 2 |
| Fatigue | 4 | 0 | 1 | 3 |
| Oedema peripheral | 4 | 1 | 1 | 2 |
| Treatment-emergent adverse events were analysed by χ2 test. | ||||
Table 5. Treatment-emergence adverse events of HGF with an overall incidence.
Treatment-emergent adverse events of HGF treatment
Patients with chronic renal failure received at least one dose of study therapy with post-baseline safety evaluation were included in the safety population. After the last dose of PRP, we observed that the most common treatment-emergent adverse events of HGF treatment (0.5 mg/kg) were hypertension and proteinuria (≥ 10% each) (Table 6). The data for the 0.85 mg/kg (n=10) and 13.0 mg/kg (n=8) doses are not advisable for more side effects and few patients were treated at these dose levels. Of the total patients, 72 patients with chronic renal failure completed the overall maintenance period of this study.
| Total (n=36) | 1.0-2.5 mg/kg (n=12) | 5.0-8.5 mg/kg (n=16) | 13.0 mg/kg (n=8) | |
|---|---|---|---|---|
| Adverse event | ||||
| Hypertension | 8 | 2 | 3 | 3 |
| Grade 1 | 2 | 0 | 1 | 1 |
| Grade 2 | 4 | 1 | 1 | 2 |
| Grade 3 | 2 | 1 | 1 | 0 |
| Proteinuria | 7 | 1 | 3 | 3 |
| Grade 1 | 4 | 1 | 1 | 2 |
| Grade 2 | 2 | 0 | 1 | 1 |
| Grade 3 | 1 | 0 | 1 | 0 |
| Treatment-emergent adverse events were analysed by χ2 test. | ||||
Table 6. Treatment hypertension and proteinuria by common toxicity criteria grade.
Efficacy of HGF treatment
The clinical outcomes of HGF treatment were analysed in this analysis. Preliminary clinical analyses exhibited that renal functions were markedly improved in drug-treatment groups after 8 weeks therapy regiment compared to placebo. Treatment of HGF improved meaningfully in physical function and renal function for patients with chronic renal failure (Table 7). These clinical outcomes showed that HGF therapy of PRP (5.0 mg/kg) improved the clinical features of patients with chronic renal failure induced by type 2 diabetes.
| Study groups | Urinary concentration (mean and SEM) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| UPO | BUN | Scr | BUA | Cr | SPI | PSP | Ccr | β2mc | |
| Placebo group | |||||||||
| Baseline | 98 | 8.6 | 158.8 | 86.6 | 3.2 | 0.48 | 0.32 | 3.8 | 89 |
| week 52 | 84 | 8.2 | 144.2 | 80.2 | 3.5 | 0.38 | 0.36 | 3.7 | 82 |
| P value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
| HGF group | |||||||||
| Baseline | 96 | 8.5 | 163.8 | 94.8 | 3.1 | 0.46 | 0.34 | 4.3 | 86 |
| week 52 | 58 | 4.2 | 87.4 | 52.2 | 6.8 | 0.068 | 0.61 | 1.3 | 41 |
| P value | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
Table 7. Renal function index changes during the study period.
Discussion
Many clinical trials and studies have demonstrated that chronic renal failure could induce symptom complex and markedly decreased the quality of life in patients [22,23]. In addition, clinical survey has showed that incidence rate of chronic renal failure was increasing with the rapid increase of diabetes in the world [24]. Patients with chronic renal failure frequently developed into uremia for dysfunctions of glomerular cells and led to loss of the biological activity of kidney cells [25]. Dialysis is the most effective treatments for kidney failure and deterioration of the quality of the life and that pathogenesis is genetic and multifactorial [26,27]. Previous study has indicated that age of the patients with chronic renal failure played a fatal factor for survival period, limitation of physical activity and quality of life in patients with chronic renal failure [28]. In this study, we investigated whether the expression and function of HGF was decreased and associated with inflammation. Date confirmed previous observations and presented that inflammatory factors may be correlate with the age and gender of patients with chronic renal failure.
Inflammation is one of the most common characteristics of in patients with type 2 diabetes [29]. Temelkova et al. reported that subclinical inflammation was up-regulated in patients with type 2 diabetes that indicated that inflammatory responses may be associated with the occurrence, degree and prognosis of diabetes [30]. Varughese et al. reported that inflammation was related with hypertension and urinary albumin excretion in patients with type 2 diabetes [10]. In addition, previous study demonstrated vascular inflammation played important role in drug induced rapid and persistent reduction of in patients with hypertension and type 2 diabetes [29]. Furthermore, Bitar et al. showed that inflammation was associated with degree pathogenesis condition in aortic tissues of aged type 2 diabetes by phosphatidylinositol 3-kinase/Akt- dependent signal pathway [31].
In this study, our investigation found that HGF and IL-6 serum concentration levels were decreased and correlated with age of patients with chronic renal failure induced by type 2 diabetes. In addition, we also found that serum concentration levels of HGF were positive correlated with gender of patients with chronic renal failure induced by type 2 diabetes based on our mathematical statistics. These investigations were focused on HGF treatment for patients with chronic renal failure induced by diabetes mellitus and provided new horizon for reducing inflammation and improving patient’s quality of life.
Though previous study has reported that inflammation indeed associated with hypertension in patients with type 2 diabetes, correlations between these inflammatory factors with type 2 diabetes were not analysed in clinical [32]. For data on HGF and IL-6 serum concentration levels related the hypertension, clinical survey has been performed with the recorded by blood pressure values in patients with chronic renal failure induced by type 2 diabetes in our study. In addition, our mathematical statistics indicated that serum concentration level of HGF was positive correlation with blood pressure values in patients with chronic renal failure induced by type 2 diabetes. However, serum concentration level of HGF was significantly increased when patients received antihypertensive drugs (date not shown). Furthermore, the therapeutic effects of HGF for patients with chronic renal failure induced by type 2 diabetes were investigated in this clinical trial. Our data suggested that HGF presented benefits for patients with chronic renal failure induced by type 2 diabetes through improvement of renal function. However, symptoms of type 2 diabetes were not systematically investigated in this work.
Conclusion
In summary, based on our clinical date, serum concentration levels of IL-1, TNF-α and MCP-1 were increased renal failure patients with type 2 diabetes. However, no correlation was found between their concentration with age or gender of chronic renal failure patients induced by type 2 diabetes. In contrary, serum concentration levels of IL-6 and HGF were not only down-regulated in renal failure patients with type 2 diabetes, which suggested that IL-6 and HGF should factored in forming clinical diagnosis and prognosis guidelines for patients with renal failure induced by type 2 diabetes. Importantly, HGF treatment improved symptoms of patients with chronic renal failure. This clinical study was researched in a small sample size, which will be further study in large number of patients with renal failure induced by type 2 diabetes.
Acknowledgements
This study was supported by grant from National Science Foundation.
Disclosure of Conflict of Interest
There was no conflict of interest in this study.
References
- Finlay E. Most interventions for preventing bone disease in chronic renal failure improved biochemical outcomes. Arch Dis Child Educ Pract Ed 2012; 97: 40.
- Benmoussa L, Renoux M, Radoi L. Oral manifestations of chronic renal failure complicating a systemic genetic disease: diagnostic dilemma. Case report and literature review. J Oral Maxillofac Surg Am Assoc 2015; 73: 2142-2148.
- Kasacka I. Involvement of gastric APUD cells in chronic renal failure. Acta Histochem 2003; 105: 319-327.
- Bos-Touwen I, Schuurmans M, Monninkhof EM. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: a cross-sectional survey study. PloS one 2015; 10: e0126400.
- Nair PA, Jivani NB, Diwan NG. Kyrles disease in a patient of diabetes mellitus and chronic renal failure on dialysis. J Family Med Prim Care 2015; 4: 284-286.
- Mowla A, Dastgheib SA, Chodedri A, Dastouri P. Chronic renal failure and diabetes mellitus: are they comparable risk factors of coronary artery disease? South Med J 2007; 100: 6-7.
- Sahasrabudhe P, Dighe T, Panse N, Deshpande S, Jadhav A, Londhe S. Prospective long-term study of patency and outcomes of 505 arteriovenous fistulas in patients with chronic renal failure: Authors experience and review of literature. Ind J Plast Surg Off Publ Assoc 2014; 47: 362-369.
- Van Sickle BJ, Simmons J, Hall R, Raines M, Ness K, Spagnoli A. Increased circulating IL-8 is associated with reduced IGF-1 and related to poor metabolic control in adolescents with type 1 diabetes mellitus. Cytokine 2009; 48: 290-294.
- Lampropoulou IT, Stangou M, Papagianni A, Didangelos T, Iliadis F. TNF-β and microalbuminuria in patients with type 2 diabetes mellitus. J Diabetes Res 2014; 2014: 394206.
- Varughese GI, Lip GY. Hypertension in patients with type-II diabetes: relation to urinary albumin excretion, endothelial function and inflammation. J Human Hypertens 2005; 19: 421-424.
- Sugimoto M, Yamaoka Y. Review of Helicobacter pylori infection and chronic renal failure. Therap Apher Dial Off J Int Soc Japan 2011; 15: 1-9.
- Daimon M, Kamba A, Murakami H. Association between pituitary-adrenal axis dominance over the renin-angiotensin-aldosterone system and hypertension. J Clin Endocrinol Metabol 2015; 3568: 2016.
- Ryu S, Shin JS, Cho YW. Fimasartan, anti-hypertension drug, suppressed inducible nitric oxide synthase expressions via nuclear factor-kappa B and activator protein-1 inactivation. Biol Pharm Bull 2013; 36: 467-474.
- Ramezani A, Nagga K, Hansson O, Lonn J, Sjowall J. Hepatocyte growth factor in cerebrospinal fluid differentiates community-acquired or nosocomial septic meningitis from other causes of pleocytosis. Fluids Barriers CNS 2015; 12: 22.
- Faletto DL, Kaplan DR, Halverson DO, Rosen EM, Vande Woude GF. Signal transduction in c-met mediated motogenesis. EXS 1993; 65: 107-130.
- Mizuno S, Nakamura T. Molecular basis for HGF-mediated regression of renal fibrosis. Japan J Clin Med 2006; 64: 312-321.
- Zhang SH, Wen KM, Wu W, Li WY, Zhao JN. Efficacy of HGF carried by ultrasound microbubble-cationic nano-liposomes complex for treating hepatic fibrosis in a bile duct ligation rat model, and its relationship with the diffusion-weighted MRI parameters. Clin Res Hepatol Gastroenterol 2013; 37: 602-607.
- Bancks MP, Bielinski SJ, Decker PA. Circulating level of hepatocyte growth factor predicts incidence of type 2 diabetes mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). Metabol Clin Exp 2016; 65: 64-72.
- Oburai NL, Rao VV, Bonath RB. Comparative clinical evaluation of Boerhavia diffusa root extract with standard Enalapril treatment in Canine chronic renal failure. J Ayurv Integr Med 2015; 6: 150-157.
- Gobbi A, Lad D, Karnatzikos G. The effects of repeated intra-articular PRP injections on clinical outcomes of early osteoarthritis of the knee. Knee Surg Sport Traumatol Arthrosc Off J 2015; 23: 2170-2177.
- Filardo G, Kon E, DI Matteo B, DI Marino A, Sessa A. Leukocyte-poor PRP application for the treatment of knee osteoarthritis. Joints 2014; 1: 112-120.
- Akyuz A, Yildiz A, Akil MA. Assessment of right ventricular systolic function in patients with chronic renal failure before and after hemodialysis by means of various echocardiographic modalities. Turk Kardiyoloji Dernegi arsivi Turk Kardiyoloji Derneginin Yayin Organidir 2014; 42: 717-725.
- Ma HB, Wang R, Yu KZ, Yu C. Dynamic changes of early-stage aortic lipid deposition in chronic renal failure rats and effects of decorin gene therapy. Exp Therap Med 2015; 9: 591-597.
- Bandara JM, Wijewardena HV, Bandara YM, Jayasooriya RG, Rajapaksha H. Pollution of River Mahaweli and farmlands under irrigation by cadmium from agricultural inputs leading to a chronic renal failure epidemic among farmers in NCP, Sri Lanka. Env Geochem Health 2011; 33: 439-453.
- Vahedi M, Malekzadeh H, Haybar H, Soltanian AR, Abdollahzadeh S. The relationship between salivary beta-2 microglobulin and uremia intensity in men with chronic renal failure. Cell J 2013; 14: 276-281.
- Silverberg D, Yalon T, Rimon U. Endovascular treatment of lower extremity ischemia in chronic renal failure patients on dialysis: early and intermediate term results. Israel Med Assoc J IMAJ 2013; 15: 734-738.
- Berry PA, Thomson SJ. Prevalence and outcome of cirrhosis patients admitted to UK intensive care: a comparison against dialysis-dependent chronic renal failure patients. Intens Care Med 2012; 38: 1729-1730.
- Marcondes JA, Martins TC, Amaral AS, Nery M. Falsely elevated testosterone in a type 1 diabetes patients with acne and chronic renal failure on dialysis. Arquivos Brasileiros De Endocrinologia E Metabologia 2012; 56: 319-323.
- Takase H, Nakazawa A, Yamashita S. Pioglitazone produces rapid and persistent reduction of vascular inflammation in patients with hypertension and type 2 diabetes mellitus who are receiving angiotensin II receptor blockers. Metabol Clin Exp 2007; 56: 559-564.
- Temelkova-Kurktschiev T, Henkel E, Koehler C, Karrei K, Hanefeld M. Subclinical inflammation in newly detected type II diabetes and impaired glucose tolerance. Diabetologia 2002; 45: 151.
- Bitar MS, Ayed AK, Abdel-Halim SM, Isenovic ER, Al-Mulla F. Inflammation and apoptosis in aortic tissues of aged type II diabetes: amelioration with alpha-lipoic acid through phosphatidylinositol 3-kinase/Akt- dependent mechanism. Life Sci 2010; 86: 844-853.
- Cizmeci D, Arkun Y. Regulatory networks and complex interactions between the insulin and angiotensin II signalling systems: models and implications for hypertension and diabetes. PloS one 2013; 8: e83640.