Research Article - Journal of Public Health Policy and Planning (2023) Volume 7, Issue 3
Geographic outreach of a temporary COVID-19 hospital in India: A critical retrospect
Harikrishnan P1*, Anchit Raj Singh2, Basant Kumar Pathak3 and Yogendra Mishra4
1Department of Internal Medicine, Armed Forces Medical College, Pune, India
2Department of Internal Medicine, Base Hospital Barrackpore, Kolkata, India
3Department of Internal Medicine, Military Hospital Allahabad, Prayagraj, India
4Department of Internal Medicine, Armed Forces Medical College, Pune, India
- Corresponding Author:
- Harikrishnan P
Department of Internal Medicine
Armed Forces Medical College
Pune, India.
E-mail: harikrisshh1991@gmail.com
Received: 10-Mar-2023, Manuscript No. AAPHPP-23-91270; Editor assigned: 14-Mar-2023, PreQC No. AAPHPP-23-91270 (PQ); Reviewed: 27-Mar-2023, QC No. AAPHPP-23-91270; Revised: 03-May-2023, Manuscript No. AAPHPP-22-91270 (R); Published: 10-May-2023, DOI: 10.35841/aaphpp- 7.3.178
Citation: Krishnan HP. Geographic outreach of a temporary COVID-19 hospital in India: A critical retrospect. J Public Health Policy Plan. 2023;7(3):178
Keywords
Makeshift hospital, Surge capacity, Pandemic, Geographic outreach.
Introduction
Towards the end of 2019, the erstwhile unassuming coronavirus spread its vicious tentacles when the country office of the World Health Organisation (WHO) was informed about a cluster of cases of pneumonia with unknown etiology in Wuhan, China [1]. The COVID-19 pandemic as we know it today battered even the most established economies beyond limits and crippled them for resources. With the threat of further outbreaks looming around, a paradigm shift in our approach toward healthcare provision is required [2]. One of the most feared ideas during the initial days of the pandemic was the overwhelming of healthcare resources [3]. This was reported during the early days from Italy which saw a rapid rise in the number of cases and deaths in a short period when the healthcare infrastructure was not prepared for them [4]. The increase in workload was measured in surge capacity, which is the ability to deal with a rapid increase in patients in a short period [5]. The concept of surge capacity planning is not new, but in light of the COVID-19 pandemic, has gained unprecedented significance [6]. To supply the demand for beds during a pandemic, many approaches have been used like converting regular hospitals into dedicated COVID-19 facilities, increasing the number of ventilators and Intensive Care Unit (ICU) beds in existing hospitals, and setting up temporary COVID-19 hospitals in areas showing a surge in cases. Temporary hospitals have been set up worldwide to combat the pandemic, however, there have been mixed results. Fangcang shelter hospitals in China were one perceived success story, however, there were quite a few failures including temporary hospitals in New York at the Javits center and Europe which had to be close down due to underutilization of their facilities even at a time when there were reports of the permanent healthcare system in the respective cities being overwhelmed [7-9].
In one such effort, the Government of India established temporary COVID-19 hospitals across different parts of the country to tackle the crisis, the first of which was in the national capital, Delhi. With an increasing burden upon the existing healthcare facilities in terms of bed availability, staffing, and resources, such temporary hospitals catering only to COVID-19 cases were established on a war footing to mitigate the impact of the pandemic [10,11].
In July 2020, to combat the COVID-19 surge in Delhi, a COVID-19 hospital temporarily set up in the South West district of Delhi was inaugurated. The facility was one of its kinds and widely publicized in print and digital media. The hospital had a total of 1000 beds including 250 intensive care beds with ventilators. This facility was designed for moderate and severe patients of COVID-19; however, any confirmed COVID-19 patient was eligible for admission here. Treatment in the hospital was made available without any charges from patients. This mega facility was projected to boost the COVID-19 bed capacity in Delhi by 7% with an increase in ICU beds by 11% [12].
This raises an important question about the rationale of setting up a single mega facility to cater to a large metropolitan area versus setting up smaller facilities throughout the metropolitan area. Initial strategies that were adopted at the beginning of the pandemic were based on lessons learned from combating the SARS pandemic in Southeast Asia. A single designated hospital in a city proved to be an effective strategy for SARS, however, policymakers were quick to realize that this strategy will not work for COVID-19 as this pandemic was of an unprecedented scale [13-15]. We can learn from the experience of combating the COVID-19 pandemic to prepare ourselves for similar health crises in the future.
While many factors influence healthcare utilization, accessibility is one of the more important factors [16]. With some temporary COVID-19 hospitals being utilized satisfactorily and others being underutilized, it seems prudent to study the importance of distance to the hospital. This could lead to better resource management and scaling of hospitals for equitable distribution of resources. There is no published literature on this topic, and since the outbreak is far from over and new variants of the virus still emerging, the anticipation of larger outbreaks and preparation to mitigate it effectively is the need of the hour.
Methods
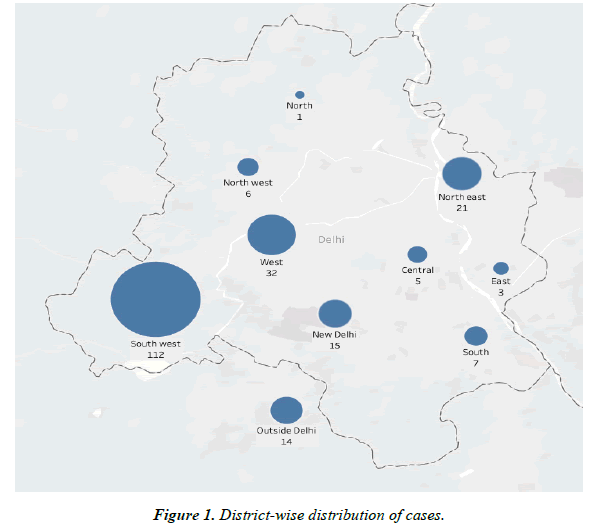
This is a cross-sectional study based on a temporary COVID-19 hospital in India. We performed this study to outline the geographical outreach of a temporary COVID-19 hospital in times of a pandemic when the existing healthcare facilities are being overwhelmed. Data were collected from the hospital records of all patients admitted to the hospital between 13 July 2020 and 05 August 2020. This included their age, sex, the severity of COVID-19, and home addresses. Individuals, who resided farther than 300 km away from the hospital, were excluded from the study. As part of this study, written informed consent was taken. The study was approved by the Institutional Ethics Committee. Distance in kilometres (Km) to their respective places of residence was calculated using Google maps. Cases were defined as per the World Health Organisation (WHO) case definition for COVID-19, wherein a confirmed case is a person with laboratory confirmation of COVID-19 infection, irrespective of clinical signs and symptoms [17]. Cases were categorized into mild, moderate, and severe cases based on the Ministry of Health and Family Welfare, Government of India guidelines being followed in India. Mild cases were the ones who met the case definition with oxygen saturation (SpO2)>95% at room air and respiratory rate <24/min. Moderate cases had clinical evidence of pneumonia with oxygen saturation (SpO2) > 90% but <94% or respiratory rate ranging from 24 to 30/min on room air. Patients were categorized as severe COVID-19 if they had features of severe pneumonia characterized by tachypnoea > 30/min and/or SpO2<90 % on room air [18]. The data were compiled and analysed using IBM SPSS statistics version 25. Mean and standard deviation (SD) were calculated for the continuous variables while proportions were used for categorical variables. For proportions, 95% Confidence intervals (CI) were calculated. Spearman’s rank correlation coefficient test and Kruskal-Wallis test were used to study association and p-values less than 0.05 were considered statistically significant. District-wise data was plotted on a map using Tableau Desktop Professional Edition version 3.1.
Results
The hospital received laboratory-confirmed cases of COVID-19. A total of 216 patients were included in the study after four were excluded according to the exclusion criteria. The study population predominantly included male patients, n=161(74.5%; 95% CI, 68 to 80), as tabulated (Table 1). The age distribution of the study participants ranged from 08 to 85 years (42.1 +17.7 years). Patients in the age group ranging from 40 years to 49 years constituted the most common age group. The peak number of cases belonged to the age group of 40-49 years closely followed by the younger group of 20-29 years. Patients from nine of the eleven districts of Delhi and regions around Delhi were admitted to the hospital (Figure 1). Most patients admitted to the hospital belonged to South West district of Delhi, n=112 (51.9%; 95% CI, 45 to 58). The other leading districts were West Delhi with n=32 (14.8%; 95% CI, 10 to 19) and North East Delhi with n=21 (9.7%; 95% CI, 05 to 13). The distances from the place of residence of the patients to the hospital ranged between 01 to 142 Km (11.7 + 12.7 Km). The mean distances of patients from various parts of Delhi have been described in Table 2. It was also noted that a total of 14 patients (6.5%; 95% CI, 03 to 10) were from outside the national capital territory, Delhi with distances ranging from 21.5 to 142 Km (44.7 +2 9.9 km). A total of 154 patients (71.1%; 95% CI, 65 to 77) belonged to mild, 38 (17.6%; 95% CI, 12 to 22) were moderate category and the remaining 24 (11.1%; 95% CI, 06 to 15) had severe COVID-19 infection. Further analysis of distance and severity revealed a statistically significant positive correlation between severity and distance (p-value <0.001), boxplot plotted (Figure 2).
| Characteristics | COVID-19 cases (N=216) |
|---|---|
| Age(in years) Mean(SD) | 42.1 (17.7) |
| Age group(in years) | |
| 0-9, no (%) | 5(2.3%) |
| 10-19, no (%) | 13(6%) |
| 20-29, no (%) | 46(21.2%) |
| 30-39, no (%) | 38(17.6%) |
| 40-49, no (%) | 48(22.2%) |
| 50-59, no (%) | 27(12.5%) |
| 60-69, no (%) | 18(8.3%) |
| 70-79, no (%) | 16(7.4%) |
| 80-89, no (%) | 5(2.3%) |
| Gender | |
| Male, no (%) | 161(74.5%) |
| Female, no (%) | 55(25.5%) |
| Severity Profile | |
| Mild, no (%) | 154(71.29%) |
| Moderate, no (%) | 38(17.6%) |
| Severe, no (%) | 24(11.1%) |
Table 1. Clinical characteristics at baseline
| District | Distance(Km) Mean(SD) |
Mild No (%) |
Moderate No (%) |
Severe No (%) |
|---|---|---|---|---|
| All patients (N=216) | 11.7(12.7) | 154(71.3) | 38(17.6) | 24(11.1) |
| Central Delhi (n=5) | 13.9(1.9) | 5(100) | 0(0) | 0(0) |
| East Delhi (n=3) | 10.9(4.5) | 2(66.7) | 1(33) | 0(0) |
| New Delhi (n=15) | 9.8(4.3) | 10(66.7) | 2(13.3) | 3(20) |
| North East Delhi (n=21) | 10(4.3) | 18(85.7) | 3(14.3) | 0(0) |
| North Delhi (n=1) | 16.3(0) | 0(0) | 0(0) | 1(100) |
| North West Delhi (n=6) | 18.4(14.1) | 3(50.0) | 1(16.7) | 2(33.3) |
| South Delhi (n=7) | 11.8(6.0) | 3 (42.9) | 3(42.9) | 1(14.3) |
| South West Delhi (n=112) | 8.1(4.9) | 82(73.2) | 21(18.8) | 9(8.0) |
| West Delhi (n=32) | 10.5(6.9) | 22(68.8) | 5(15.6) | 5(15) |
| Outside Delhi (n=14) | 44.7(29.9) | 9(64.3) | 2(14.3) | 3(21.4) |
Table 2. Distances of patient’s residence to the hospital
Discussion
As COVID-19 spread, the healthcare systems of countries across the globe experienced a major setback. With an inordinate increase in the number of cases and no signs of respite, governments were forced to take on novel ways to tackle the pandemic [19-22]. In one such effort, a makeshift dedicated COVID-19 hospital was established in the South West district of the national capital territory, Delhi, India within a short period of 12 days [23]. In our study, the mean age of patients admitted to the hospital was 42.1 years which was much lower than what has been observed in other countries like the United States of America, China, and Italy [24,25]. It was observed that the distribution of cases between males and females has shown a marked difference wherein 74.5% of the study population were males.
The major proportion of patients who were admitted to the hospital was from South West district of Delhi which constituted 51.9% of the total patients. The location of the hospital within South West Delhi could be the obvious reason for a such large proportion of patients coming from this region. Although the absolute number of patients admitted to the hospital was proportionately very high for southwest Delhi, the same did not hold true concerning the severity profile of the patients. While only 8.0% of patients from South West Delhi belonged to the severe category, the proportion was much higher (21.4%) for patients from outside Delhi. Among the districts of Delhi, there was no significant difference in the severity profile when patients were from comparable distances. The higher proportion of severe cases from farther distances could be because of the much higher costs involved in the management of severe cases as compared to mild and moderate cases in private hospitals. Thereby milder cases would prefer going to a nearby healthcare facility as compared to a severe case who would come farther distances given the lower costs involved. In this hospital, all treatment and investigation were free of cost, which would have resulted in a higher proportion of severe cases from farther places, despite the problems faced in transferring severe patients. Thus, the utility of such temporary COVID-19 hospitals although irrefutable in managing all grades of severity, its scaling plays a vital role in the profile of patients being drawn from farther distances. This indicates a demand for beds for severe patients that exceed the supply. This is contrary to what would be expected assuming that severe patients would tolerate a shorter duration of the transfer due to limitations of critical care provision in ambulances. With increasing distance, the problem of transportation arises, and its role in limiting the provision of better care has been established [26]. Thus, a single mega hospital catering to a large city, even though appears to be an attractive proposition, might not always be a viable option. Instead, smaller hospitals distributed widely might be a better strategy.
The lack of previous comparisons limits the interpretation of this study and further extrapolation. Also, additional travel undertaken in case of transfer-ins has not been accounted for. To add, many factors that affect healthcare utilization have not been studied as they are beyond the scope of this study.
COVID-19 had crippled our existing healthcare facilities for want of resources and manpower. Makeshift facilities with capabilities to hold a large number of patients with supporting manpower are deemed to affect the outcome of such pandemics. Countries or regions with the preparedness of such kind may emerge successful in tackling the outbreak. Realizing the key role played by communication and widespread publicity of such facilities, unprecedented measures are to be taken by the government and health care staff to ensure maximal utilization of such makeshift hospitals. Considering this severity-guided outreach of the hospital, it would be wise to decentralize such facilities into smaller centres catering to severe cases in multiple places. Such an effort might mean more targeted care and reduce unnecessary fatigue of staff and underutilization of beds. With the threat of more vicious and deadly outbreaks persisting, better planning of available resources would enable us to fight the pandemic better.
References
- Li JY, You Z, Wang Q, et al. The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future. Microbes Infect. 2020;22(2):80-5.
- Covid resurgence in China?: The Tribune India. 2022.
- Chatterjee K, Chatterjee K, Kumar A, et al. Healthcare impact of COVID-19 epidemic in India: A stochastic mathematical model. Med J Armed Forces India. 2020;76(2):147-55.
- Chidini G, Villa C, Calderini E, et al. SARS-CoV-2 infection in a pediatric department in Milan: a logistic rather than a clinical emergency. Pediatr Infect Dis J. 2020;39(6):e79-80.
- Sheikhbardsiri H, Raeisi AR, Nekoei-Moghadam M, et al. Surge capacity of hospitals in emergencies and disasters with a preparedness approach: a systematic review. Disaster Med Public Health Prep. 2017;11(5):612-20.
- Buerhaus PI, Auerbach DI, Staiger DO. Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA. 2020;323(18):1777-8.
- Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305-14.
- Mareiniss DP. The impending storm: COVID-19, pandemics and our overwhelmed emergency departments. Am J Emerg Med. 2020;38(6):1293.
- Sun K, Chen J, Viboud C. Early epidemiological analysis of the coronavirus disease 2019 outbreak based on crowdsourced data: a population-level observational study. Lancet Digit Health. 2020;2(4):e201-8.
- India’s DRDO to set up temporary 1000-bed hospital for Covid-19 patients. Hosp Manag. 2021.
- DRDO builds 1000-bed temporary covid hospital in 12 days 2. 2020.
- Explained: The Covid-19 hospital in Delhi that came up in just 12 days. 2020.
- Willan J, King AJ, Jeffery K, et al. Challenges for NHS hospitals during covid-19 epidemic. BMJ. 2020;368.
- Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8(4):e488-96.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67(5):568-76.
- Arcury TA, Gesler WM, Preisser JS, et al. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Re. 2005;40(1):135-56.
- WHO COVID-19 Case definition.
- Ministry of Health and Family Welfare. Clinical management protocol?: COVID-19. 2020.
- John TJ. How prepared is India to control the COVID-19 pandemic? Econ Polit Wkly. 2020;55(11):13-15.
- Cohen J, Kupferschmidt K. Strategies shift as coronavirus pandemic looms. Sci. 2020;367(6481):962-963.
- Ebrahim SH, Ahmed QA, Gozzer E, et al. Covid-19 and community mitigation strategies in a pandemic. BMJ. 2020;368..
- Ayebare RR, Flick R, Okware S, et al. Adoption of COVID-19 triage strategies for low-income settings. Lancet Respir Med. 2020;8(4):e22.
- Delhi: 1,000-bed dedicated Covid hospital ready to be operational. 2020.
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-9.
- Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020;323(14):1335.
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38:976-93.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref