Review Article - Journal of Cardiovascular Medicine and Therapeutics (2018) Volume 2, Issue 4
General review on cardiac implants and study of the methods for reducing electromagnetic interference (EMI).
- *Corresponding Author:
- Hamidreza Shirzadfar
Department of Biomedical Engineering Sheikhbahaee University Isfahan, Iran
Tel: +98 31 3681 6761
E-mail: h.shirzadfar@shbu.ac.ir; h.shirzadfar@gmail.com
Accepted date: November 13, 2018
Citation: Shirzadfar H, Khanahmadi M. General review on cardiac implants and study of the methods for reducing electromagnetic interference (EMI). J Cardiovasc Med Ther. 2018;2(4):1-8.
Abstract
Human heart can produce pulses and electrical impulses based on electrical specialized cells and with the use of sympathetic and parasympathetic nerves, these beats can also be adjusted. Cardiac arrhythmias and heart disease affect the electrical activity of the heart and impair cardiac function. Therefore, medical equipment and various therapies should be used to improve cardiac function. The pacemaker is designed to produce pulses and regular beats for those whose heart does not function properly and does not have regular beats. Pacemakers and cardiac implants have several types that are inserted into the body of cardiac patients. The main elements of the pacemakers include generators, batteries, and leads, which generator to produce pulses and batteries to power the device and finally, the pulses produced through the leads are sent to the heart. The pacemakers are divided into different types based on the number of leads and catheters, each of which has its own function.
Keywords
Pacemaker, Electromagnetic interference, Cardiac, Electrical device, Electric generator.
Introduction
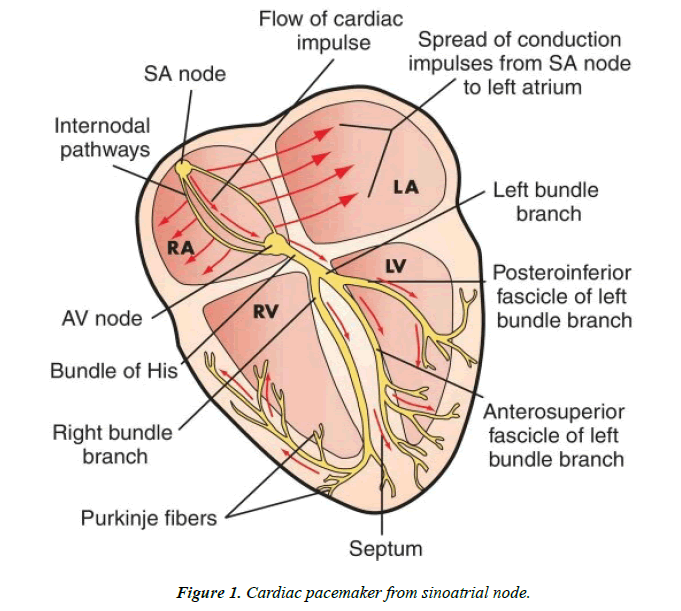
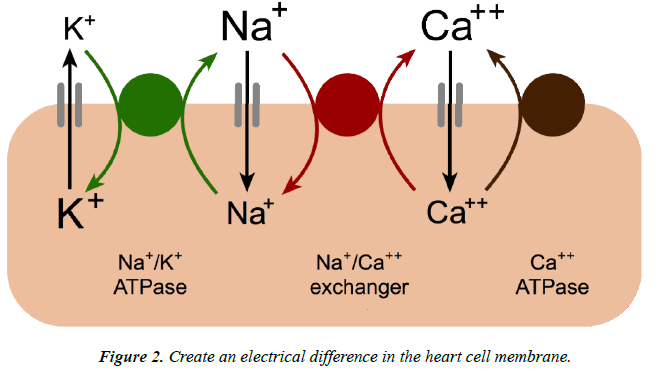
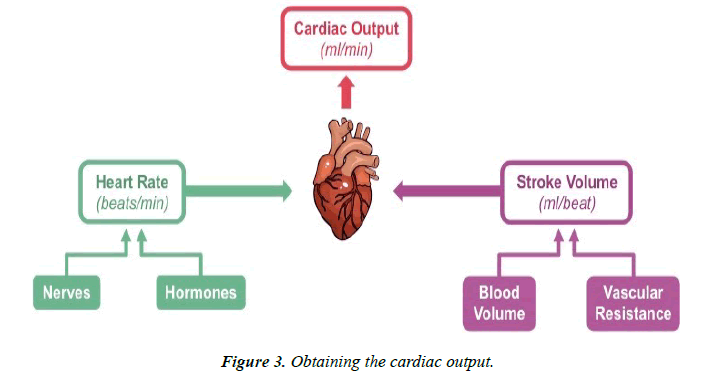
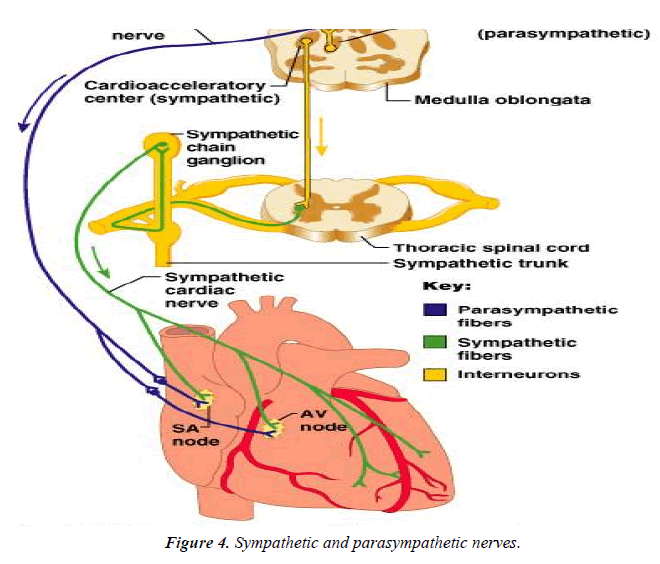
According to WHO reports and studies, cardiovascular disease is one of the major causes of death in the world [1,2]. The cardiac has millions of specialized cells that generate electrical impulses throughout the cardiac that produce these waves at the sinoatrial node (SA) that sinoatrial node is the pacemaker of the cardiac [3,4] (Figure 1). The electrical activity of the cardiac is due to the concentration and movement of sodium, potassium and calcium ions from the cell membrane, which causes an electrical difference [5,6] (Figure 2). Cardiac output is one of the cardiac parameters that is used to evaluate the function of the cardiac system. The amount of blood that goes out of the cardiac at each beat is equal to the stroke volume. When the heart rate is multiplied by the stroke volume, a cardiac output is obtained [7-9] (Figure 3). The heart rate is adjusted based on the sympathetic and parasympathetic nervous system [10,11] (Figure 4).
In some cases, the heart electrical system may have flaws and the heart has irregular and arrhythmic beats, which include tachycardia and bradycardia, and atrial fibrillation is one of the common cardiac arrhythmias. Various factors can cause these arrhythmias that include cardiac artery stenosis, cardiac valve diseases, blood pressure, abnormalities in metabolic glands, and so on [12,13].
Literature Review
There are various treatments for heart disease. One of the treatment methods for impaired electrical and heart rates is the use of Implantable Cardioverter Defibrillators (ICDs) and pacemakers, which is a very efficient and suitable method [14].
Examination of pacemakers and ICDs
Pacemaker is one of the vital medical devices that performs pacemaking heart function and is used for patients with cardiac diseases [15] (Figure 5).
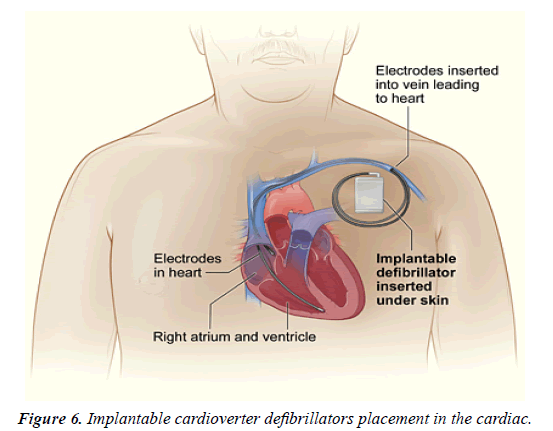
Using this device, can be adjust the heart rate, and thus can be adjust the heart rate normal and regular. Pacemakers simulate heartbeat and produce regular pulses [16,17]. ICDs with pacemakers are functionally different. ICDs are used for patients who have severe heart attacks, and the device produces more power electric shocking, which makes the heartbeat return to normal [18,19] (Figure 6).
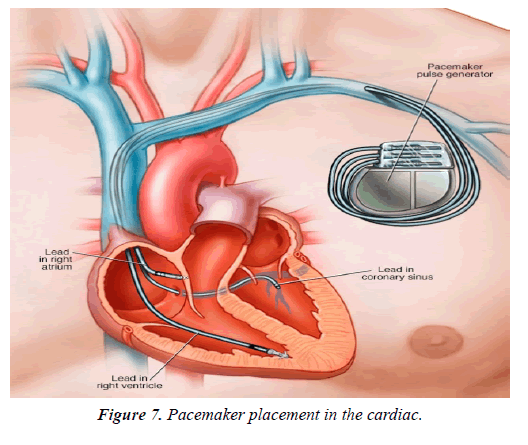
The pacemaker devices are small, and they have weighed too little, which are planted on the left side of the body and along the clavicle bone and under the skin, and the device's leads are placed in the vessels of the heart [20] (Figure 7).
The pacemakers have different types and are made up of miniature electrical circuits. The pacemakers have batteries that are needed for energy. Basically, the life span of these batteries varies from 5 to 10 years, and they are made of lithium. Recently, pacemakers have been designed that do not require a battery and get their energy from heart activity [21,22]. The pacemakers have the generator and the lead, which generator produces electrical pulses and is sent to the heart via electrodes [23]. Also, pacemakers have two types of unipolar and bipolar catheters, which are electrodes that transmit electrical impulses to these catheters [24].
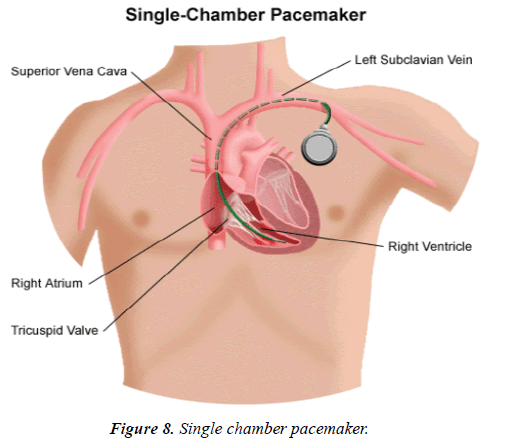
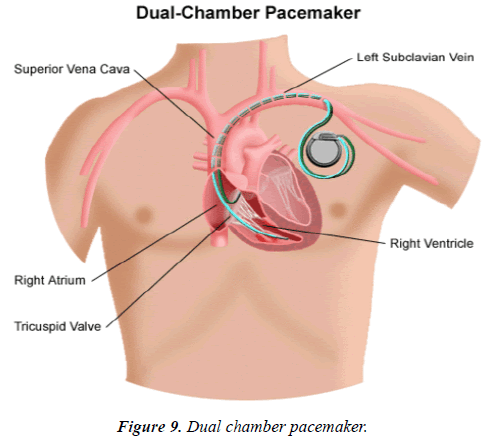
The pacemakers are divided into three general categories based on the number of leads. A single chamber is referred to a pacemaker that has a lead and this lead connects to the ventricle (Figure 8). The other pacemaker has two leads, the leads connect to the ventricle and atrium, and perform better than the first type and this kind of pacemaker is called the dual chamber [25,26] (Figure 9). The third type has three leads called Triple Chamber or Biventricular [27].
The pacemakers are divided into different types based on the location of the leads in the ventricles or atriums and the stimulated sensation in the ventricles and atria, each of which has its own characteristics and different output rates. Some pacemakers permanently and continuously generate regular electrical pulses, but some of the pacemakers begin to work when the heart rate is slowed down or stopped. The expert physician can check and control the pacemaker by the programmer and pass the necessary commands to the pacemaker [28]. Some pacemakers use a sensor that can monitor heart rhythms and control the transmission of electrical pulses. The pacemakers can use the clock placed in the circuit of this device to control the pulse transmission time and generate a pulse with a constant period of time. As a result, the pacemakers have two synchronous and asynchronous modes that are different in the transmission of electrical impulses [29,30].
An expert physician evaluates the performance of the pacemaker using the ECG recorder, which examines electrical stimulation and impulses with regard to the ECG. The size of the curve derived from the ECG depends on several factors, including the number of leads and the electrical output of the pacemaker [31].
Materials used in making parts and circuits for pacemakers should be non-toxic and biocompatible. The pacemaker circuit is made of silicone material and the body of the pacemakers is made of titanium and its alloys. The pacemaker lead should be durable and flexible, which are made of metal alloys with a polymeric coating [32].
The pacemakers also have complications. These unwanted complications include damage to the vessels that causes bleeding or infection.
Pacemakers are sensitive to electromagnetic and electrical waves, causing electromagnetic and electrical interference, and affects the performance of the pacemaker. This is very important for people who have a pacemaker and they work in electrical and generators for electricity production environments, and so on [33,34].
Various factors including electromagnetic field and high voltage electric field, flow leakage from electrical device, etc. can cause these interferences, which can cause the pulse generator to stop and cause damage to the pacemaker circuits [35,36]. Devices such as industrial generators, radiotherapy devices, MRI imaging device, etc. are sources of electrical and electromagnetic interference [37].
Today, methods have been proposed to prevent electromagnetic and electrical interferences on pacemakers, which will further explore these interferences and methods of reducing interferences.
Study of electromagnetic interference (EMI)
Electromagnetic interference is caused by the superposition of electromagnetic waves and electromagnetic radiation generated by circuits of electrical devices. These interferences are obtained by electromagnetic induction from electronic circuits These interferences cause noise and disturbances on waves and adjacent devices and undesirable effects on the performance of electronic equipment circuits [38,39].
Electromagnetic interference is transferred to equipment, circuits and other waves based on conduction and radiation. Electromagnetic interferences that are transferred to other equipment based on the conduction method are divided into common mode and differential mode. Electromagnetic interference with the radiation method by the emission of electromagnetic waves in the physical environment [40].
Electromagnetic interference has various sources that include electrostatic discharge, sun, thunderbolt, electronic equipment, electromechanical circuits, and so on [41].
Reducing electromagnetic interference on the performance of the pacemakers
Now-a-days, using in vitro methods, can be test and investigate the effects of electric and magnetic fields on pacemakers [42]. In some studies, experts have been able to experiment of electromagnetic interference using numerical simulation of the anatomical human body in the form of real with the insertion of a cardiac implant [43].
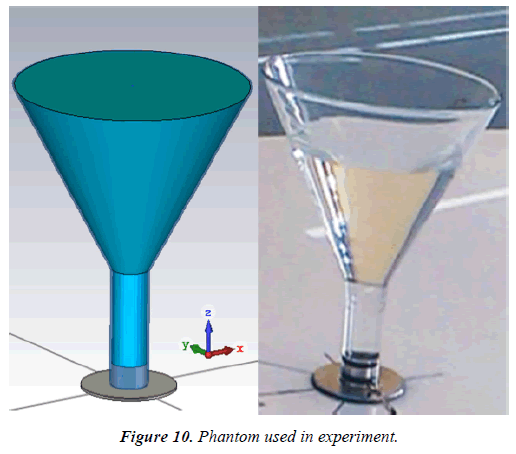
In one of these studies, the phantom used in experiment resembles a glass funnel that has a height of 35.2 cm and is filled with a salt solution, and the end of the funnel has a metal that connects to the ground (Figure 10). This phantom is then placed in a bench that produces a high voltage electric field, and this phantom is examined under the influence of electric and magnetic waves [44].
In other studies, using finite integral technic, anatomical human body was placed in a field of 50 Hz and the effects of this field on the pacemaker on this model were investigated and therefore the voltage interference in unipolar and bipolar mode [45].
To reduce electromagnetic interference in the pacemaker device, should be consider the circuit design of this device and check it. For example, using ICs and new microcontrollers in the design of the pacemaker circuit, the amount of electromagnetic interference can be reduced [46].
To reduce electromagnetic interference, it is also possible to isolate leads and pacemaker electrodes, which prevents lowfrequency noise and reduces electrical interference. In this method, suitable coatings and cover are used that are isolated from another element. Using thin films made of several layers of graphene at very small sizes, which reduces electromagnetic interference [47].
Magnetic nanoparticles can be used as filters for electromagnetic interference. In this way, electromagnetic waves can be absorbed by the magnetic nanoparticles and become heat, and thus reduce the electromagnetic interference [48].
By using protective coatings (shielding) made up of polyaniline films, the effect of electromagnetic interference on pacemaker can be reduced. These films are made of emeraldine salt, which are obtained using materials as a base on polyethylene terephthalate film [49].
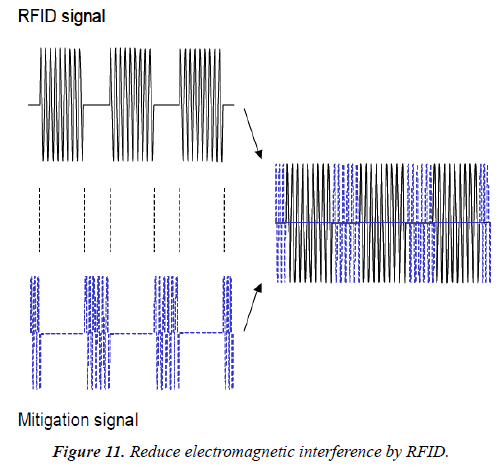
One of the ways to reduce electromagnetic interference is the use of RFID (Radio Frequency Identification) technology. RFID systems can create and transmit periodic signals. This system has a signal transmission period and a stop period. Signals of the system during the stopping period can reduce the magnetic signals that cause interference. As a result, the magnetic signal passes through a very low frequency, and electromagnetic interferences are reduced [50] (Figure 11).
Discussion and Conclusion
In this article, a general review of the pacemakers was given. The main components of the pacemakers include batteries, generators, leads and electrodes. The pacemaker can transmit electric impulses to the heart and normalize the heart rate. Pacemakers are designed and manufactured in a variety of ways, each with its own function. The pacemakers have electromagnetic and electrical interferences by electric generators, high voltage electronics devices, and flow leakage from electrical device. These interferences cause damage to the pacemaker electrical circuit that is very dangerous for patients with pacemaker. Therefore, researchers have examined various methods that can reduce these electromagnetic interferences. The methods for reducing the electromagnetic interference discussed in this paper include RFID technology, magnetic nanoparticles, protective coatings, isolation of leads and electrodes and so on.
References
- Ettehad D. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. The Lancet 2015;387:957-67.
- Shirzadfar H, Ghaziasgar M, Piri Z, et al. Heart beat rate monitoring using optical sensors. Int J Biosen Bioelectron. 2018;4:45-51.
- Unudurthi S, Wolf R, Hund T. Role of sinoatrial node architecture in maintaining a balanced source-sink relationship and synchronous cardiac pacemaking. Front Physiol. 2014;5:446.
- Shirzadfar H, Khanahmadi M, Mahlouji E, et al. Wavelet technique and function for noise removal from ECG signal. International Journal of Bioinformatics and Computational Biology. 2018;3:1-5.
- Vikram A, Lewarchik CM, Yoon JY, et al. Sirtuin 1 regulates cardiac electrical activity by deacetylating the cardiac sodium channel. Nat Med. 2017;23:361-7.
- Wu F, Wang C, Xu Y, et al. Model of electrical activity in cardiac tissue under electromagnetic induction. Scientific Reports. 2016;6:28.
- Slagt C, Malagon I, Groeneveld A. Systematic review of uncalibrated arterial pressure waveform analysis to determine cardiac output and stroke volume variation. Br J Anaesth. 2014;112:626-37.
- Ameloot K, Palmers P, Malbrain M. The accuracy of noninvasive cardiac output and pressure measurements with finger cuff: A concise review. Curr Opin Crit Care. 2015;21:232-9.
- Lee JY, Kim JY, Choi CH, et al. The ability of stroke volume variation measured by a noninvasive cardiac output monitor to predict fluid responsiveness in mechanically ventilated children. Pediatr Cardiol. 2014;35:289-94.
- Pereira MR, Leite PE. The involvement of parasympathetic and sympathetic nerve in the inflammatory reflex. J Cell Physiol. 2016;231:1862-9.
- Shirzadfar H, Khanahmadi M. Introduction to design and manufacture of a heart signal simulator and graphic displayer based on the ATmega microcontroller. J Biol Med Sci 2018;2:2.
- Ballestri S, Lonardo A, Bonapace S, et al. Risk of cardiovascular, cardiac and arrhythmic complications in patients with non-alcoholic fatty liver disease. World J Gastroenterol. 2014;20:1724-45.
- Shen M, Zipes D. Role of the autonomic nervous system in modulating cardiac arrhythmias. Circ Res. 2014;114:1004-21.
- Zaremba T, Jakobsen AR, Søgaard M, et al. Radiotherapy in patients with pacemakers and implantable cardioverter defibrillators: A literature review. Europace. 2016;18:479-91.
- Kokotsakis J, Chaudhry UA, Tassopoulos D, et al. Surgical management of superior vena cava syndrome following pacemaker lead infection: A case report and review of the literature. J Cardiothorac Surg. 2014;9:107.
- Reddy VY, Exner DV, Cantillon DJ, et al. Percutaneous implantation of an entirely intracardiac leadless pacemaker. N Engl J Med. 2015;373:1125-35.
- Siontis GC, Jüni P, Pilgrim T, et al. Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing TAVR. J Am Coll Cardiol. 2014;64:129-40.
- Parthiban N, Esterman A, Mahajan R, et al. Remote monitoring of implantable cardioverter-defibrillators: A systematic review and meta-analysis of clinical outcomes. J Am Coll Cardiol. 2015;65:2591-600.
- Saeed M, Hanna I, Robotis D, et al. Programming implantable cardioverter-defibrillators in patients with primary prevention indication to prolong time to first shock: Results from the provide study. J Cardiovasc Electrophysiol. 2014;25:52-9.
- Bjerre TJ, Loh PH, Cholteesupachai J, et al. Reevaluation of the indications for permanent pacemaker implantation after transcatheter aortic valve implantation. J Invasive Cardiol. 2014;26:94-9.
- Cruciani S, Campi T, Maradei F, et al. Numerical simulation of wireless power transfer system to recharge the battery of an implanted cardiac pacemaker. International Symposium on Electromagnetic Compatibility. 2014.
- Miller MA, Neuzil P, Dukkipati SR, et al. Leadless cardiac pacemakers back to the future. J Am Coll Cardiol. 2015;66:1179-89.
- Noro M, Zhu X, Takagi T, et al. Left axillary pacemaker generator implantation with a direct puncture of the left axillary vein. Pacing Clin Electrophysiol. 2015;38:35-41.
- Gemein C, Haj M, Schmitt J. Combining a subcutaneous ICD and a pacemaker with abdominal device location and bipolar epicardial left ventricular lead: first-in-man approach. Europace. 2016;18:1279.
- Anandhi K, Nagarajan R. Mutex-Heart: Fail safe dual chamber cardiac pacemaker device with rate responsive control and cryptographic security. Int J for Scientific Research & Development. 2015;3:489-93.
- Veselka J, Krejcà J, Toma?ov P, et al. Outcome of patients after alcohol septal ablation with permanent pacemaker implanted for periprocedural complete heart block. Int J Cardiol. 2014;171:37-8.
- Calvagna GM, Patanè S. Venous occlusion after transvenous pacemaker implantation: Is there a role for new oral anticoagulants?. Cardiovasc Drugs Ther. 2015;29:99-100.
- Chwyczko T, Dabrowski R, Maciag A, et al. Potential prevention of pacing-induced heart failure using simple pacemaker programming algorithm. Ann Noninvasive Electrocardiol. 2013;18:369-78.
- Chen T, Diciolla M, Kwiatkowska M, et al. A simulink hybrid heart model for quantitative verification of cardiac pacemakers. Proceedings of the 16th International Conference on Hybrid Systems: Computation and Control. 2013.
- Park H, Nadeem M, Malik A, et al. The cardiac pacemaker: System vs. safety critical java. Proceedings of the 12th International Workshop on Java Technologies for Real-time and Embedded Systems. 2014.
- Toutouzas K, Synetos A, Tousoulis D, et al. Predictors for permanent pacemaker implantation after core valve implantation in patients without preexisting ECG conduction disturbances: The role of a new echocardiographic index. Int J Cardiol. 2014;172:601-3.
- Hwang GT, Park H, Lee JH, et al. Self-powered cardiac pacemaker enabled by flexible single crystalline PMN-PT piezoelectric energy harvester. Adv Mater. 2014;26:4880-7.
- Biner S, Michowitz Y, Leshem-Rubinow E, et al. Hemodynamic impact and outcome of permanent pacemaker implantation following transcatheter aortic valve implantation. Am J Cardiol. 2014;113:132-7.
- Anselme F, Moubarak G, Savouré A, et al. Implantable cardioverter-defibrillators in lamin A/C mutation carriers with cardiac conduction disorders. Heart Rhythm. 2013;10:1492-8.
- Labedi MR, Alharethi R, Kfoury AG, et al. Electromagnetic interference of automatic implantable cardioverter defibrillator and heart-ware left ventricular assist device. ASAIO J. 2013;59:136-9.
- Periyasamy M, Dhanasekaran R. Electromagnetic interference on critical medical equipments by RF devices. International Conference on Communication and Signal Processing. 2013.
- Shirzadfar H, Khanahmadi M. Physical principles and recent advances of medical imaging systems. AASCIT Journal of Health. 2018;5:21-7.
- Thomassin JM, Jérôme C, Pardoen T, et al. Polymer/carbon-based composites as electromagnetic interference (EMI) shielding materials. Materials Science and Engineering. 2013;74:211?32.
- Guo YJ, Wang LF, Liao CL. Modeling and analysis of conducted electromagnetic interference in electric vehicle power supply system. Progress in Electromagnetics Research. 2013;139:193?209.
- 40. Chen Z, Xu C, Ma C, et al. Lightweight and flexible graphene foam composites for high-performance electromagnetic interference shielding. Advanced Materials. 2013;25:1296-300.
- Genender E, Garbe H, Sabath F. Probabilistic risk analysis technique of intentional electromagnetic interference at system level. IEEE Transactions on Electromagnetic Compatibility. 2014;56.
- Misiri J, Kusumoto F, Goldschlager N. Electromagnetic interference and implanted cardiac devices: The medical environment (Part II). Clin Cardiol. 2012;35:321-8.
- Gercek C, Magne I, Kourtiche D, et al. Numerical and experimental study of implanted cardiac defibrillators immunity to ELF electric fields. International Symposium on Electromagnetic Compatibility-EMC Europe.2017.
- Gercek C, Kourtiche D, Nadi M, et al. An in vitro cost-effective test bench for active cardiac implants, reproducing human exposure to electric fields 50 Hz. Int J on Smart Sensing and Intelligent Systems. 2017;10:1-17.
- Gercek C, Kourtiche D, Nadi M, et al. Computation of pacemakers immunity to 50 Hz electric field: Induced voltages 10 times greater in unipolar than in bipolar detection mode. Bioengineering (Basel). 2017;4:19.
- Napp A, Stunder D, Maytin M, et al. Are patients with cardiac implants protected against electromagnetic interference in daily life and occupational environment?. Eur Heart J. 2015;36:1798-804.
- Yousefi N, Sun X, Lin X, et al. Highly aligned graphene/polymer nanocomposites with excellent dielectric properties for high-performance electromagnetic interference shielding. Adv Mater. 2014;26:5480-7.
- Shubitidze F, Kekalo K, Stigliano R, et al. Magnetic nanoparticles with high specific absorption rate of electromagnetic energy at low field strength for hyperthermia therapy. J Appl Phys. 2015;117:094302.
- Kim B, Lee H, Park S, et al. Electromagnetic interference shielding characteristics and shielding effectiveness of polyaniline-coated films. Thin Solid Films. 2011;519:3492-6.
- Kawamura Y, Futatsumori S, Hikage T, et al. A novel method of mitigating EMI on implantable medical devices: Experimental validation for UHF RFID reader/writers. IEEE International Symposium on Electromagnetic Compatibility. 2009.