Case Report - Journal of Gastroenterology and Digestive Diseases (2018) Volume 3, Issue 2
Gastric carcinoma recurring as an isolated breast secondary after three years from curative treatment.
Donnell SO1*, Abd Elwahab S1, Auchwraz N1, Lal A1, Tormey S1, Coate L2 and El-Bassiouni M3
1Mid-western Breast Unit, University Hospital Limerick, Republic of Ireland
2Department of Oncology, University Hospital Limerick, Republic of Ireland
3Department of Radiation Oncology, University Hospital Limerick, Republic of Ireland
- *Corresponding Author:
- Donnell S
Mid-western Breast Unit
University Hospital Limerick
Republic of Ireland
Tel: +353 61 301 111
E-mail: sineadod47@gmail.com
Accepted on Sep 05, 2018
Citation: Donnell SO, Abd Elwahab S, Auchwraz N, et al. Gastric carcinoma recurring as an isolated breast secondary after three years from curative treatment. J Gastroenterol Dig Dis 2018;3(2):41-43.
Abstract
Extra-mammary tumour metastases to the breast are extremely rare accounting for less than 2% of all breast lesions. Breast secondaries were reported with lymphoma, melanoma, ovarian carcinoma, renal cell carcinoma, colonic adenocarcinoma and gastric carcinoma. Stomach cancer metastases to the breast are very rare, with an incidence believed to be around 2.1% of all breast secondaries. The presentation is usually quite similar to breast primary; therefore clinicians need to keep an open mind when discussing histology as additional immune-histo-pathological tests are usually necessary to fully diagnose the cancer. Our case was a 55-years-old female who was treated for gastric signet ring carcinoma in 2013. She was referred to our breast clinic three years post curative surgical and chemotherapeutic management of her stomach cancer with a right breast lump with oedema and thickening of the overlying skin. She was thought to have inflammatory breast carcinoma; however, further histological tests demonstrated signet ring cells consistent with metastatic gastric carcinoma. Radiological staging tests confirmed single isolated breast secondary with no other metastatic lesions. To best of our knowledge, this is the only case of isolated breast secondary from gastric tumour. In this report, we reviewed the literature; discussed patient presentation and management, including breast metastectectomy. Keywords: Gastric carcinoma,
Keywords
Gastric carcinoma, Immuno-histopathological, Chemothrerapy, Extramammary, Metastatic.
Introduction
Breast cancer metastasis is common however metastatic disease is rarely seen in the breast. Gastric cancer metastasis to the breast is extremely rare, with only about 38 cases reported in literature to date since 1908 [1]. Despite being quite rare, the possibility of metastatic disease should be considered when assessing breast masses, which occur in patients with previous cancer history. Correct diagnosis as extramammary metastasis is essential as the treatment options differ to that of primary breast cancer. Clinicians need to keep an open mind when discussing histology, as additional immune-histo-pathological testing is usually necessary to fully diagnose the type of cancer involved.
In this report, we present a gastric cancer recurring three years after curative treatment as an isolated malignant breast lump.
Case Presentation
A 55-year-old female was referred to the Mid-Western Breast Unit complaining of hard lump in her right breast for the past two and a half weeks. She has history of gastric signet ring cell carcinoma (pT3N2M0) in 2013 treated by total gastrectomy, Roux-en-Y, splenectomy for an infarcted spleen as well as modified McDonald adjuvant regimen; radiotherapy and chemotherapy with Capecitabine. Histology revealed an infiltrating poorly differentiated adenocarcinoma with 8 positive lymph nodes out of the 16 resected. She was three years’ post-curative surgical and chemotherapeutic management of her stomach cancer when she noticed this breast lump.
Physical examination revealed a highly suspicious two centimeter mass in the right breast associated with nipple inversion, edema and thickening of the overlying skin. The left breast and both axillae were normal on examination.
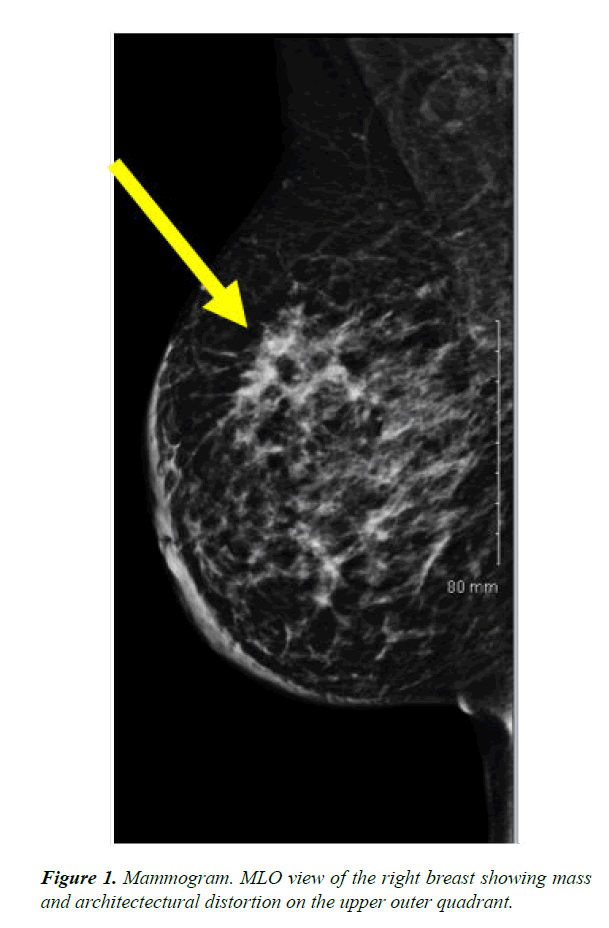
Mammography showed scattered fibroglandular densities and diffuse tissue asymmetry within the right breast (Figure 1). Ultrasound revealed a diffuse, vague hypoechoic abnormality in the superior right breast with ill-defined margins (Bi-RADS Score: R5). Ultrasound-guided core needle biopsies demonstrated signet ring cell adenocarcinoma, strongly expressed CK7 and CK20, and not reactive to GCFP-15. This was discussed in a multidisciplinary meeting (MDM) and thought to be consistent with metastatic gastric carcinoma. Staging CT-TAP demonstrated a marked increased size and density of irregular parenchymal tissue of the right breast with generalized skin thickening throughout the breast. Radiological staging tests confirmed single isolated breast secondary with no other metastatic lesion.
After MDM discussion, the patient underwent neo-adjuvant radiotherapy and chemotherapy with 6 cycles of ACT of which there was a partial response. She then underwent right mastectomy with no axillary procedure, as it was not indicated. The patient had an uneventful post-operative course and her wounds healed well on review.
Discussion
According to the National Cancer Registry Ireland, it is estimated that 1 in 10 women will develop breast cancer before their 75th birthday. While breast cancer remains the second most common type of cancer in women, extra-mammary tumour metastases to the breast are extremely rare, accounting for less than 2% of all breast lesions [2]. Breast secondaries were reported with lymphoma, melanoma, ovarian carcinoma, colonic adenocarcinoma and gastric carcinoma. Stomach cancer metastases to the breast are very rare, with an incidence believed to be around 2% of all breast secondaries.
Misdiagnosis of breast secondaries as a primary cancer is common [3]. The importance of the distinction is to ensure that the most appropriate management plan is considered for the patient. The presence of metastasis is indication of systemic disease and therefore requires systemic treatment with additional therapies to surgical resection. Prognosis in these cases is generally poor as it is usually indicative of extensive metastatic disease, with a high mortality rate. The median survival from the time of breast metastasis diagnosis is about 10 months [4].
Metastatic disease of the breast typically occurs in patients with widespread metastatic disease [5]. However, as our case demonstrates breast secondaries may be the first manifestation of metastatic spread.
While the mechanisms behind breast metastasis from gastric cancer remains controversial. It has been suggested that there is a higher incidence of metastasis in premenopausal women potentially due to the increased blood supply to the breast in this particular group [1,6]. It has also been proposed that hormonal factors have a role to play in promoting adhesion and growth of breast metastases from gastric cancer [7].
Immunohistochemical testing of the cancer cells can be beneficial in determining the primary origin. While the presence of ER and PR in breast cancer is well known, it has been shown that up to 20% of gastric cancers have been ER positive [8]. A combination of the use of ER and CK20 staining has been proven useful in determining if the metastatic carcinoma is originating from the gastrointestinal tract or from mammary tissue [9], GCFP-15 has been widely used as a marker for breast carcinoma. Immunostaining with GCFP-15 has been shown to have specificity of up to 95% in the detection of breast cancer [10]. Our patient was seen to be CK20 positive and unreactive to GCFP-15, which would add validity to the primary origin being from the gastrointestinal tract.
Conclusion
Isolated single metastectomy was shown to improve patient outcomes. Reports showed that it increased survival and reduced mortality by up to 88% [11]. Surgical management usually involves conservative management with wide local excision, however as in the case with our patient, mastectomy is required for large bulky tumours [12]. While surgery is often the treatment of choice for these patients, the focus needs to remain on the treatment of the primary origin of the cancer [12]. Systemic chemotherapy has been shown to improve the prognosis of patients with breast secondaries6, as is the case with our patient.
References
- He CL., Chen P, Xia BL, et al. Breast metastasis of gastric signet-ring cell carcinoma: A case report and literature review. World J Surg Oncol. 2015;13(1):120.
- Georgiannos SN, Chin Aleong J, Goode AW, et al. Secondary neoplasms of the breast. Cancer. 2001;92(9): 2259-66.
- Lee SK, Kim WW, Kim SH, et al. Characteristics of metastasis in the breast from extramammary malignancies. J Surg Oncol. 2010;101(2):137-140.
- Lee AHS. The histological diagnosis of metastases to the breast from extramammary malignancies. J Clinical Pathol. 2007;60(12):1333-41.
- Noguera J, MartínezMiravete P, Idoate F, et al. Metastases to the breast: A review of 33 cases. J Med Imaging Radiat Oncol. 2007;51(2):133-138.
- Iesato A, Oba T, Ono M, et al. Breast metastases of gastric signet-ring cell carcinoma: A report of two cases and review of the literature. OncoTargets Ther. 2015;8:91.
- Vergier B, Trojani M, De Mascarel I, et al. Metastases to the breast: Differential diagnosis from primary breast carcinoma. J Surg Oncol. 1991;48(2):112-16.
- Kojima O, Takahashi T, Kawakami S, et al. Localization of estrogen receptors in gastric cancer using immunohistochemical staining of monoclonal antibody. Cancer. 1991;67(9):2401-06.
- Tot T. The role of cytokeratins 20 and 7 and estrogen receptor analysis in separation of metastatic lobular carcinoma of the breast and metastatic signet ring cell carcinoma of the gastrointestinal tract. APMIS. 2000;108(6):467-72.
- Wick MR, Lillemoe TJ, Copland GT, et al. Gross cystic disease fluid protein-15 as a marker for breast cancer: Immunohistochemical analysis of 690 human neoplasms and comparison with alpha-lactalbumin. Human Pathol. 1989;20(3):281-87.
- Williams SA, Ehlers RA, Hunt KK, et al. Metastases to the breast from nonbreast solid neoplasms. Cancer. 2007;110(4):731-37.
- McFarlane ME. Metastasis to the breast: A rare site for secondary malignancy. Int J Surg. 2006;4(4):204-205.