Editorial - Journal of Infectious Diseases and Medical Microbiology (2017) Volume 1, Issue 1
Fungal infections: a veritable worldwide problem.
André LS Santos1*, Marta H Branquinha1, Lucimar F Kneipp21Department of General Microbiology, Institute of Microbiology Paulo de Góes, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
2Oswaldo Cruz Institute, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil
- *Corresponding Author:
- André LS Santos
Department of General Microbiology
Institute of Microbiology Paulo de Góes
Federal University of Rio de Janeiro
Rio de Janeiro
Brazil
Tel: +55 21 3938 6740
E-mail: andre@micro.ufrj.br
Accepted date: October 24, 2017
Citation: Santos ALS, Branquinha MH, Kneipp LF. Fungal infections: a veritable worldwide problem. J Infectious Disease Med Microbiol. 2017;1(1):1-2.
Editorial
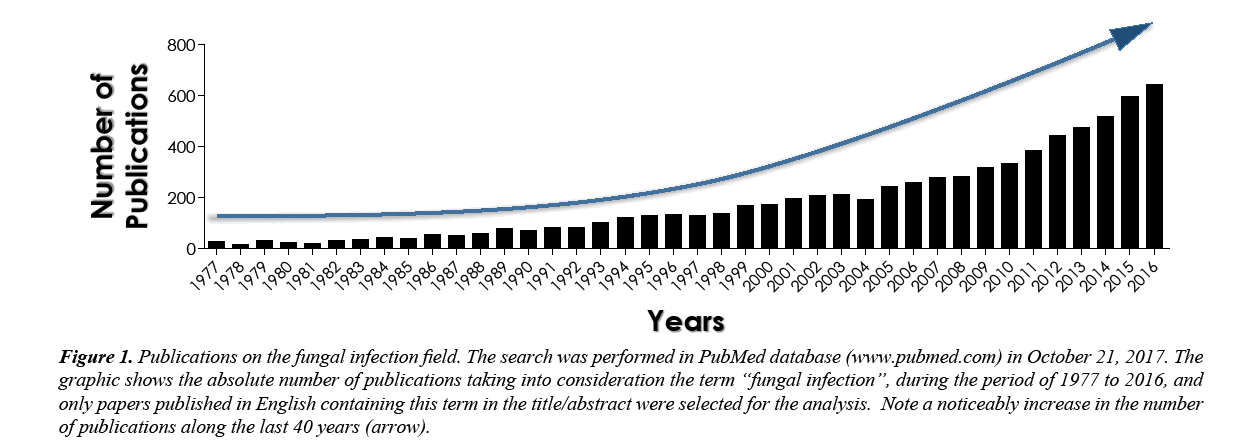
Fungi comprise an extremely diversified group of eukaryotic single-celled or multinucleated organisms, which can be found in virtually all the planet environments, including soil, water and air. Over the last decades, the incidence of fungal infections in human beings has considerably increased [1-3], as can be noticed by a simple and quick query to the PubMed database (www.pubmed.com) (Figure 1), reiterating that it is an effervescent field of scientific research in the biomedical field. In addition, a clear epidemiologic change regarding the fungal infections has been reported in many hospitals around the world [4,5]. In this new scenario, for example, the species of Candida causing infection are more diverse than previously and Candida albicans does not predominate as it once did. In this context, several non-albicans Candida (e.g., Candida glabrata, Candida tropicalis, Candida parapsilosis, Candida guilliermondii and Candida krusei) have become prevalent in some hospitals due to the intrinsic resistance against widespread antifungal agents used currently in the clinical arena, particularly fluconazole. Similarly, changes in the epidemiology of filamentous fungal infections have also occurred. Aspergillus species remain the most common cause of mold infections in humans, but there has been an increase in infections due to other molds, such as Scedosporium/ Pseudallescheria spp., Fusarium spp., Mucor spp., Rhizopus spp.; several of them are resistant to amphotericin B [1-9].
Figure 1: Publications on the fungal infection field. The search was performed in PubMed database (www.pubmed.com) in October 21, 2017. The graphic shows the absolute number of publications taking into consideration the term “fungal infection”, during the period of 1977 to 2016, and only papers published in English containing this term in the title/abstract were selected for the analysis. Note a noticeably increase in the number of publications along the last 40 years (arrow).
Medically important fungi can be characterized as either primary or opportunistic pathogens. Primary pathogens are those that are capable of routinely causing disease in otherwise healthy hosts, whereas opportunistic pathogens are those that generally require overt immunosuppression in order to cause disease [10-12]. Infection can be considered as an imbalance between the host defences and the infectious agent, with the host unable to control the proliferation of the infectious agent [10-12]. In general, two major populations have been at higher risk for acquiring invasive fungal infections: (1) individuals that live in endemic geographic location, for example in the United States of America it includes infections with Histoplasma capsulatum var. capsulatum along the Mississippi River Valley, Coccidioides immitis in the Southwest and Blastomyces dermatitidis in the central and southeastern States [13]; (2) persons with increased host susceptibility, who develop opportunistic infections, such as (a) severely ill, (b) hospitalized patient population who needs care in specialized units and the use of invasive monitoring devices, parenteral nutrition, broad-spectrum antimicrobial agents and assisted ventilation, (c) immunocompromised patients due to the newer technologies and therapies, such as bone marrow or solid-organ transplants and chemotherapeutic agents, or HIV infection, and (d) people with primary immunodeficiencies that are hereditary disorders involving one or multiple components of the immune system, including humoral, cellular, combined humoral and cellular, phagocytic, complement, and other, well characterized immunodeficiency syndromes [10-12]. These population presents increased susceptibility to fungal infections and significant morbidity and mortality if untreated. Fungal infections in these patients are often severe, rapidly progressive and difficult to diagnose or treat [10-12].
The rise in the incidence of fungal infections has exacerbated the need for the next generation of antifungal agents, since many of the currently available drugs have undesirable side effects, are ineffective against new or reemerging fungi and/ or lead to the rapid development of resistance. Furthermore, the improvement of new antifungal compounds is very limited due to the eukaryotic architecture of fungal cells, which is very similar to the human cells, and its huge genome plasticity [14]. Recently, another strategy in face of serious fungal disease is the use of combinations of drugs. Combination therapy can enhance efficacy over monotherapy, avoid toxic effects of either one or both drugs by reducing the dosage and increase the therapeutic benefits against fungal infections caused by multidrug-resistant strains [14,15]. Additionally, very little is known about the biochemical aspects of the pathogenicity of these organisms as well as the virulence attributes directly implicated in the fungal infectious process. For all these reasons, the search for novel fungal targets is an imperative task as well as the development of new antifungal drugs to improve the armamentarium to combat these severe, numerous and universal infections [14,15].
References
- Kauffman CA. Fungal infections. Proc Am Thorac Soc. 2006;3(1):35-40.
- Debourgogne A, Dorin J, Machouart M. Emerging infections due to filamentous fungi in humans and animals: only the tip of the iceberg? Environ Microbiol Rep. 2016;8(3):332-42.
- Suleyman G, Alangaden GJ. Nosocomial fungal infections: epidemiology, infection control, and prevention. Infect Dis Clin North Am. 2016;30(4):1023-52.
- Richardson MD. Changing patterns and trends in systemic fungal infections. J Antimicrob Chemother. 2005;56:i5-i11.
- Benedict K, Richardson M, Vallabhaneni S, et al. Emerging issues, challenges, and changing epidemiology of fungal disease outbreaks. Lancet Infect Dis. 2017.
- Cole DC, Govender NP, Chakrabarti A, et al. Improvement of fungal disease identification and management: combined health systems and public health approaches. Lancet Infect Dis. 2017.
- Jensen RH. Resistance in human pathogenic yeasts and filamentous fungi: Prevalence, underlying molecular mechanisms and link to the use of antifungals in humans and the environment. Dan Med J. 2016;63(10).
- Pilmis B, Puel A, Lortholary O, et al. New clinical phenotypes of fungal infections in special hosts. Clin Microbiol Infect. 2016;22(8):681-87.
- Perlin DS, Rautemaa-Richardson R, Alastruey-Izquierdo A. The global problem of antifungal resistance: prevalence, mechanisms, and management. Lancet Infect Dis. 2017.
- van Burik JA, Magee PT. Aspects of fungal pathogenesis in humans. Annu Rev Microbiol. 2001;55:743-72.
- Antachopoulos C, Walsh TJ, Roilides E. Fungal infections in primary immunodeficiencies. Eur J Pediatr. 2007;166(11):1099-117.
- Köhler JR, Casadevall A, Perfect J. The spectrum of fungi that infects humans. Cold Spring Harb Perspect Med. 2014;5(1):a019273.
- Reingold AL, Lu XD, Plikaytis BD, et al. Systemic mycoses in the United States, 1980–1982. J Med Vet Mycol. 1986;24(6):433-36.
- Carmona EM, Limper AH. Overview of treatment approaches for fungal infections. Clin Chest Med. 2017;38(3):393-402.
- Wiederhold NP. Antifungal resistance: Current trends and future strategies to combat. Infect Drug Resist. 2017;10:249-59.