Case Report - Journal of Advanced Surgical Research (2017) Volume 1, Issue 1
Frequency of stroke with relation to modifiable risk factors with an emphasis on hypertension; in a Karachi based tertiary care hospital
Sumera Nawaz1*, Farzeen Tanwir2, Mubashir Riaz3, Faisal Ziauddin4, Umer Jahangir5, Nael Alvi5, Fahad Bawani6
1Medicine dr Ziauddin Hospital, Canada
2Department of Periodontology, University of Toronto, Canada
3Department of Gio Information, University of Toronto, Canada
4Department of Medicine, University of Toronto, Canada
5Department of Analyst, University of Toronto, Canada
6Department of English, University of Toronto, Canada
- *Corresponding Author:
- Sumera Nawaz
Medicine University of Toronto
Canada
Tel: 92 3362092118
E-mail: sumeraqabulio@gmail.com
Accepted date: May 16, 2017
Abstract
Stroke is the main sources of mortality and grimness around the world. The accepted range for circulating blood pressure is currently systolic 120-130 mmHg and diastolic 80-90 mmHg In China, hypertension is the second greatest driving factor for cardiovascular accidents.
Keywords
Hypertension, disease, blood pressure, diastolic, diabetes.
Introduction
Stroke is the main sources of mortality and grimness around the world. The accepted range for circulating blood pressure is currently systolic 120-130 mmHg and diastolic 80-90 mmHg [1]. Pre hypertension is an independent chance variable for cardiovascular accidents [2-5]. Increased Blood pressure was suggestive for the danger of cardiovascular sickness [6]. As indicated by American Heart Association systolic circulatory strain of 140 mmHg in patients under 80 years and 140 to 150 mmHg in patients over 80 years of age is a significant risk factor for cardiovascular disease. In China, hypertension is the second greatest driving factor for cardiovascular accidents.
Stroke is one of the leading causes of lifelong disability with significant risk factors including: serious illness by noncommunicable disease such as hypertension, male gender, smoking, obesity, increased lipid levels, diabetes, and increased Uric Acid. In one review it was found that among all strokes patients, around 2/3rd of the cases were found to be hypertensive and almost 50% of all patients were found to have high systolic blood pressure (SBP); more than 115 mmHg [7]. The expanded in SBP and diastolic blood pressure (DBP) both are imperative hazard components for having stroke. A portion of the current reviews shows; hypertensive patients have a seven times greater risk for stroke than normotensive patients [8,9]. Around 45 overall forthcoming accomplices have demonstrated a significant relationship of stroke with raised diastolic blood pressure. A rise in SBP by 10 mmHg shown to lead to an 80% increased risk of stroke [10]. Both of DBP and SBP have been hazard variables for stroke [11]. High blood pressure prompting stroke is thought to be a movable reason for stroke [12]. In creating nations the quantity of stroke patient is high when contrasted with that created countries [15]. The prevalence of hypertension for all intents and purposes was found to be as high as 20% of the population in Iran [13-16]. Generally, strokes can be ascribed worldwide to high BP values regardless of gender or age [17] with hypertensive patients being found to be three to four times more prone to having a stroke as compared to normotensive patients [18].
Similarly, as with hypertensive patients, patients with diabetes were found to have a significant increased risk of stroke. Generally it is accepted that Fasting hyperglycaemia, that is glucose that is higher than 130 mg/dL (milligrams per decilitre) after not eating or drinking for a minimum of 8 hours or Postprandial (after meal) hyperglycaemia that is glucose that is higher than 180 mg/dL 2 hours after eating on more than one occasion is indicative of diabetes. It was found that patients who have suffered a previous stroke were found to be more likely to be suffering from hyperlipidaemia than those without diabetes (16 versus 8%, freely, P<0.0001 in the GCNKSS) [19]. Although stroke has a higher incidence among diabetic patients, most reviews, report for the most part a decreased rate of transient ischemic attacks (TIAs) in diabetic patients as compared to no diabetic patients [20]. Diabetic patients are most likely to present with ischemic cerebral infarcts, with a decreased rate of reversal as compared to non-diabetic patients [21].
Hyperlipidemia is the leading factor for atherosclerotic changes in blood vessels [22,23] which in turn may, most significantly lead to an increase in incidence of both myocardial infarctions and strokes.
Study design
Prospective single blind Cohort Study.
Test: ANOVA for different variables was used.
Sample size: 154 patients were chosen for the enlistment of the review
Entry: The SPSS of VERSION 20 utilized for the information for section of the member.
Location: Dr. Ziauddin hospital (Kemari), Karachi, Pakistan grounds was chosen for the review.
Inclusion criteria
1. Hypertensive patient.
2. Known diabetes mellitus type 2.
3. Known instance of Ischemic coronary illness.
4. Known instance of Hyperlipidaemia.
5. Patient presented with neurological deficient.
6. Age more than 16 to75years old.
Exclusion criteria
1. History of stroke in past.
2. Stroke older than 48 hours.
Duration of study: January 2016- January 2017.
Limitations
This study was limited to Dr. Zaiuddin Hospital Karachi and its various branches with a sample pool of 154 patients.
Result
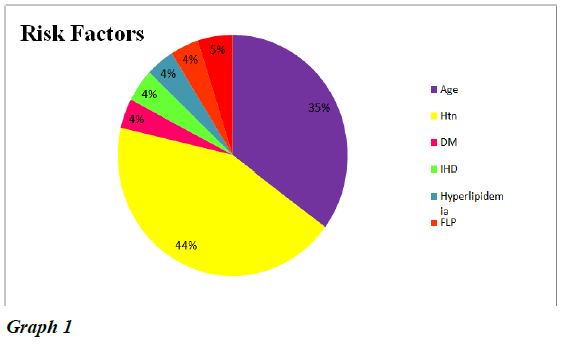
The occurrence of ischemic stroke and intra cranial drain were hazard components Diabetes, hypertension age, hyperlipidemia and ischemic coronary illness. A sum of 154 was enlisted in the review. In our review we found that the Hypertension is seen 44 percent of the cases. The second most critical hazard variable was Age with the rate of 35 percent and DM and Hyperlipidemia were 5 percent and 4 percent separately as appeared in Graph 1.
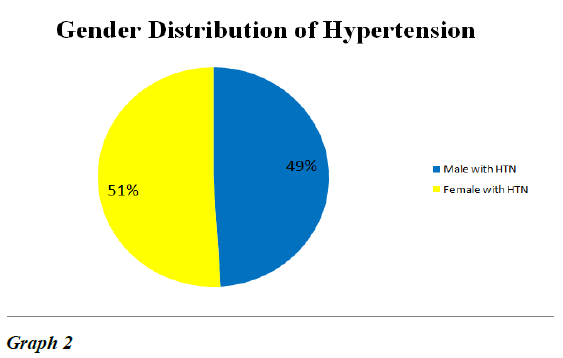
Hypertension is found to one of the main source in the cerebrovascular accident. 51 patient were observed to be hypertension and 49 patients were female. No such sexual orientation relationship with hypertension found as appeared in chart 2.
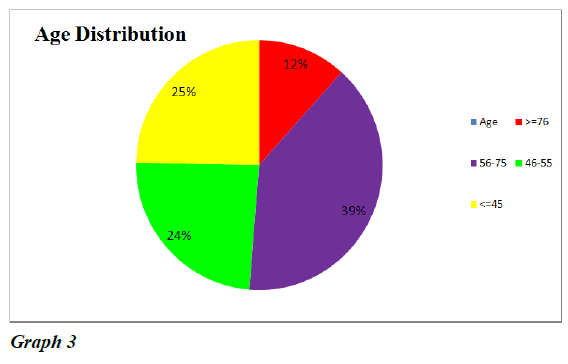
Mortality because of stroke is influenced by age, with more noteworthy age related with higher rates of mortality Graph 2.The crest in total number of passing’s was seen in those matured 56 to 75 years with a most elevated rate of 39 percent As the age advance danger of the danger of cerebrovascular mischance’s increases. The odds of cerebrovascular accident lesser found in age under 45 and over 75 years as appeared in Graph 3.
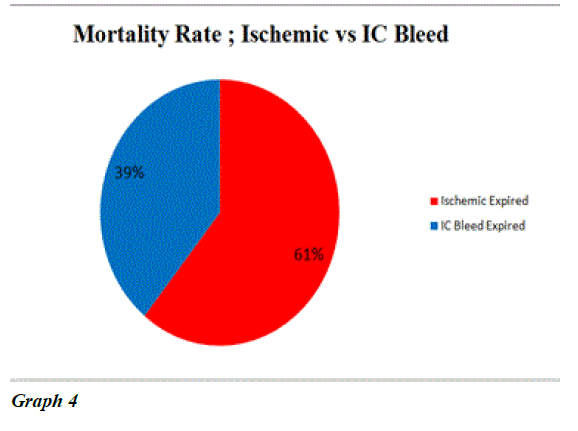
The ratio of mortality in stroke patients are given below in the Graphs 4 and 5. 25 expiries seen in the result of the study The ratio was double than ischemic infarct seen in the study and its association more found in hypertension patients.
In our study we have concluded that hypertension is the leading cause of stroke of both ischemic and intra cranial bleed than other known risk factors. The hypertension in ischemic infarct patients were 98 out of 151. In term of percentage it was 44 percent. Second most variables was age more than 55years with percentage of 35 percent .and no such gender association However Hypertension can be corrected with proper medications timely and DASH Diet.
Conclusion
Past reviews from Pakistan demonstrate these hazard figures, that are predictable/conflicting with our outcomes. Hypertension is an intense sickness, prompting stroke trouble in a group. Distinctive factors utilized including: age, sex, diabetes and hyperlipidemia. Consequently regard the cause as though not fittingly treated prompting extreme harm. In the event that we treat the underlining chance variables, we may significantly reduce the chance cerebrovascular accidents. Hypertension can be modified with anti-hypertensive medications, diet such as the DASH diet, regular exercise and leading a non-sedentary lifestyle. Threat factor amendment remains the most significant point in prevention of stroke. Expertise of threat elements has superior and several alternatives at the moment are available to treat modifiable chance factors. However, powerful treatment stays a tough mission in clinical practice. Prevention starts with attention to the danger elements with the aid of both doctors and patients. All stroke patients should undergo threat component assessment along with the usual stroke danger estimation on the bases of clinical judgment. In this assessment we must address the effect modifiable risk factors on ischemic stroke, the relevant intervention for said risk factors for stroke prevention. Emphasis must be placed on public education in regards to risk factors and prevention with specific targeted education towards certain jobs. All future studies in the fields of genetic determinacy vascular stroke risk factors will lead increase our understanding of the underlying mechanisms said cerebrovascular disorders and will most likely result in the development of newer more effective therapies for stroke prevention.
References
- Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee: The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003, 289: 2560-72.
- 2.SadeghiM,AghababaeiE, Talaei M,et al. Do hypertension and prehypertension count as cardiovascular risk factors among women in an Iranian society. Int J Cardiol 2012; 155.
- 3.Erbel R, Lehmann N, Möhlenkamp S, Heinz Nixdorf Recall Study Investigators: Subclinical coronary atherosclerosis predicts cardiovascular risk in different stages of hypertension: result of the Heinz Nixdorf Recall Study. Hypertension 2012; 59: 44-53.
- Suri MF, Qureshi AI. Prehypertension as a risk factor for cardiovascular diseases.J CardiovascNurs 2006; 21: 478-82.
- 5.Gupta P, Nagaraju SP, Gupta A, et al.Prehypertension - time to act. SaudiJ Kidney Dis Transpl.2012;23:223-33.
- 6.Lee M, Saver JL, Chang B, et al. Presence of baseline prehypertension and risk of incident stroke: a meta-analysis. Neurology 2011; 77: 1330-37.
- Lawes CM, Vander Hoorn S, Law MR, et al. Comparative quantification of health risks: global andregional burden of disease attributable to selected major risk factors. Geneva: World Health Organization. 2004;281-390.
- Victor M, Ropper A. Adams and victor s principles ofneurology. 7th edition New York: McGraw Hill; 2001.
- Michael J, Aminoff MJ, David A, et al. Clinical neurology. 5th edition New York: McGraw Hill;2002:123-40.
- APCSC.Cholesterol, diastolic blood pressure, and stroke 13,000 strokes in 450,000 people in 45 prospective cohorts.Prospective studies collaboration. Lancet 1995;346:8991-153.
- Steyn K, Jooste PL, Bourne L, et al.Risk factors for coronary heart disease in the black population of the Cape Peninsula.The BRISK study. SAfr Med J1991;79:480-5.
- Law MR, Wald NJ. Risk factor thresholds: their existence under scrutiny. BMJ 2002;324:1570- 6.
- Walker RW, McLarty DG, Kitange HM, et al. Stroke mortality in urban and rural Tanzania. Adult morbidity and mortality project. Lancet2000;355:1684-7.
- 14.Sadeghi M, Roohafza H, Sadry G, et al. Prevalence of high blood pressure and its relation with cardiovascular risk factors. J Qazvin Univ Med Sci2003;26:46-52.
- 15.Sharifi F, Azizi F. Prevalence of hyper lipidemia, overweightand hypertension in diabetic and IGT patients and control groups in rural of Zanjan province. J Fac Med ShahidBeheshtiUniv Med Sci1997;4:41-50.
- Pour Abdolahi P, Ghaemaghami S, EbrahimiMamghani M.Survey of abdominal obesity and hypertension in Tabrizianwomen (25?26 old years). BehdashtSalamat 2004;1:23-4.
- Lawes CM, Vander Hoorn S, Rodgers A. International Society of Hypertension. Global burden of blood-pressure-related disease, 2001 Lancet 2008;371:1513-8.
- Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;14:1903-13.
- GorelickPB. New horizons for stroke prevention: PROGRESS and HOPE. Lancet Neurol. 2002;1:149-56.
- Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;14:1903-13.
- Onder G, Volpato S, Liperoti R, et al. Total serum cholesterol and recovery from disability among hospitalized older adults. J Gerontol A Biol Med Sci. 2006;61:736-42.
- Wouters K, Shiri-Sverdlov R, van Gorp PJ, et al. Understanding hyperlipidemia and atherosclerosis: lessons from genetically modified apoe and ldlr mice.Clin Chem Lab Med: CCLM/FESCC. 2005;43:470-9.
- Ross R, Harker L. Hyperlipidemia and atherosclerosis. Science1976;193:1094-100.