Research Article - Biomedical Research (2017) Volume 28, Issue 6
Free bone retention plus iliac bone grafting under phase I vacuum sealing drainage lavage for treatment of Gustilo type I, II, and IIIA open bone defects
Leigang Yang1, Yungang Yang2*, Xiuming Yang2, Tianxu Yang2, Yuxuan Yang2 and Junjie Xie11Department of Orthopaedics, Xianyang Centre Hospital, Xianyang, China
2Department of Pain, Xianyang Yangsa Hospital, Xianyang, China
Accepted on November 1, 2016
Abstract
This study aimed to investigate the treatment efficacy of free bone retention plus iliac bone grafting under phase I Vacuum Sealing Drainage (VAS) lavage for treatment of open bone defects. Thirty-six bone fractures were classified according to the Gustilo classification between January 2008 and April 2016. This study included 16 type I cases, 12 type II cases, and 8 type IIIA cases. Length of the longitudinal section of the damaged free crushed bone was 0.5 to 7.1 cm. There were 7 cases with sections ≤ l cm, 12 with sections 2 to 3 cm, 11 with sections 3 to 5 cm, and 6 with sections>5 cm. The rinse protocol comprised 3000 ml/d of saline for 3 days for Gustilo type I fractures, 6000 ml/day of saline for 5 days for Gustilo type II fractures, and 9000 ml/d of saline for 7 days for Gustilo type IIIA fractures. Fifty ml of Anerdian (type III, diluted 10 fold) was added by VSD treatment (closed negative-pressure lavage). Callus formation was seen within 3.5 months after surgery, with osseous union at an average of 6.5 months. The wound healed well in 35 cases. In l case, the patient developed superficial cellulitis near the screw path, which resolved after removing the external fixation device. There was no internal fixation loosening, breakage, or exposure. Non-union and osteomyelitis were not seen. This method could be effective to prevent infection, osteomyelitis, delayed union, and non-union.
Keywords
Bone grafting, Open fracture, Bone defect, Treatment.
Introduction
High-energy, trauma-induced bone and soft tissue injuries often include multiple complex injuries, which can be severe, have longer treatment periods, and involve complex tissue remodeling. Early and repeated debridement may result in deep infection after wound closure. It also may lead to development of delayed chronic osteomyelitis [1-3], which is one of the difficulties of clinical treatment. Exfoliation of bone and loss of soft tissue attachments could result in lack of blood supply. Contamination of the wound could lead to infection, resulting in secondary traumatic osteomyelitis, sequestrum, and lack of complete sinus healing over the long term. This often requires removal of the contaminants and a 3 month waiting period before surgical bone grafting, which greatly increases risk of bone defects from debridement and fixation [4]. Emergency free flap transfer, which involves partially transferring or freeing the skin or muscle flap, is difficult to utilize for soft tissue injuries, which require a more complex surgery when using deferred wound closure. Traditional drainage pipes have a small negative pressure, and, as such, often become plugged. Plugging results in incomplete rinsing, poor drainage, and serious leakage, making traditional drainage pipes unsuitable for soft tissue defects. They also can increase patients’ pain, prolong hospital stays, and increase medical burdens. There are many flushing methods to control infection [5-8], each with their own advantages and disadvantages. Hydrogen peroxide (3%) has been proved to be cytotoxic, and long-term application affects wound healing. Benzalkonium bromide (0.1%) is a weak disinfectant, and is no longer used. Iodophors may maintain sterile conditions for only 1 hour, and may result in serious tissue death, making them unsuitable for surgeries requiring visual distinction. Topical application of antibiotics is controversial, while iodine tincture and iodophors require deiodination. Additionally, iodine tincture is a strong irritant, and can be used for skin disinfection only. Povidone-iodine (5%) can be toxic, and may result in significant damage to epithelial tissue. Therefore, there are still many problems to solve in the treatment of open fracture bone injuries. Many current treatments have unsatisfactory effects, making them unsuitable for open fracture bone defects. In addition, some of the treatment cycles are long and easily complicated by osteomyelitis and non-union, resulting in increased duration of infection, long operating times, and high costs. Additionally, the rates of disability and amputation are high [9,10]. In order to increase the efficacy of treatment, we applied a method using free bone retention plus iliac bone grafting under phase I Vacuum Sealing Drainage (VSD) lavage for treatment of 36 Gustilo types I, II, and IIIA open bone injuries between January 2008 and April 2016 [11-13]. The current study demonstrates that this method can produce sufficient drainage and effective infection control, as well as rapid bone union and convenient care, resulting in positive clinical outcomes.
Materials and Methods
Subjects
Thirty-six patients with open bone limb fractures were selected from 52 patients with severe soft tissue injuries who were admitted to the First Department of Orthopaedics, Xianyang Centre Hospital, Shaanxi Province, between January 2008 and April 2016. The patient group included 23 men and 13 women aged 23 to 68 years, with a mean age of 39 years. Fracture types were classified according to the Gustilo classification, and included type I (16 cases), type II (12 cases), and type IIIA (8 cases) fractures. Bone fractures occurred in the humerus (8 cases), tibial shaft (13 cases), femoral shaft (8 cases), ulnar shaft (4 cases), and radial shaft (3 cases). Length of the longitudinal section of the injured free crushed bone was 0.5 to 7.1 cm, and included section lengths of ≤ 1 cm (7 cases), 2 to 3 cm (12 cases), 3 to 5 cm (11 cases), and>5 cm (6 cases). Fixation types include external stent fixation in all 36 cases. Time from injury to surgery ranged from 8 to 38 hours, with an average of 11.2 hours. Causes of injury were traffic accidents (29 cases) and falls (7 cases). This study was conducted in accordance with the Declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Xianyang Centre Hospital. Written informed consent was obtained from all participants.
Inclusion criteria
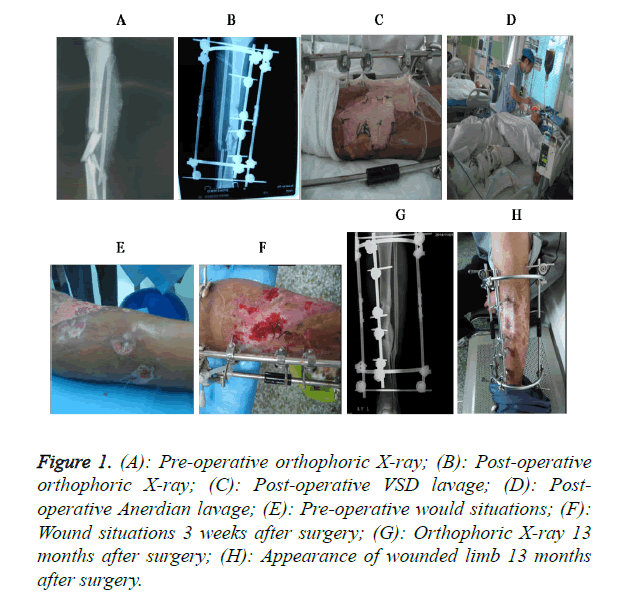
Patients were included in the study based on the following criteria: (1) the injury was confirmed as a limb fracture by imaging studies, (2) the injury was an open fracture accompanied by bone damage and severe soft tissue injury, (3) the wound could not automatically heal or be sutured directly, and (4) the patients and their families were informed and provided informed consent (Figure 1A).
Figure 1. (A): Pre-operative orthophoric X-ray; (B): Post-operative orthophoric X-ray; (C): Post-operative VSD lavage; (D): Postoperative Anerdian lavage; (E): Pre-operative would situations; (F): Wound situations 3 weeks after surgery; (G): Orthophoric X-ray 13 months after surgery; (H): Appearance of wounded limb 13 months after surgery.
Exclusion criteria
Patients were excluded if they met any of the following conditions: (1) malignant cancer, (2) obvious vascular occlusive disease, (3) unmanaged diabetes, (4) intolerance to treatment, or (5) adverse reaction to treatment (allergy to polyvinyl alcohol-hydrated seaweed salt foam dressing, or intolerance to pain caused by closed negative-pressure therapy).
Debridement and exploration
After successful anaesthesia, samples were collected from the wound and sent for bacterial culturing and sensitivity testing. The wound was dressed with sterile dressing, and the wounded limb was brushed twice. Subsequently, the wound was rinsed with hydrogen peroxide followed by Anerdian (Shanghai LiKang Disinfectant High Tech Co., Ltd.) and saline. The wound was sterilized and a sterile surgical towel was paved, and the fascia tissue was cut away from the contused skin edge. The areas contaminated by the contusion and the inside of the wound were cleared of visible foreign bodies and dirt particles. The surgeon then explored the wound to verify the condition of the tendons, muscles, blood vessels, nerves, skin, and fracture injuries to determine the surgical plan and method of fixation. This was followed by rerinsing with hydrogen peroxide followed by Anerdian and saline (Figures 1B-1D).
Bone grafting
Wounds with bone debris or that were heavily contaminated by foreign material were scraped or bit partial bone with a size 1 bone curette. Autologous free bone collected for the graft was washed repeatedly, soaked in hydrogen peroxide and diluted Anerdian/saline solution, and then reduced and fixed to the bone. The graft site was filled with autologous iliac cancellous bone, with the graft exceeding the upper and lower extent of the fracture by approximately 1 cm. The joint capsule, muscles, and tendons were then sutured in turn. Finally, the skin was sutured relaxationally, and the wound was narrowed and closed to cover the bone graft.
VSD lavage
Several side holes were cut in 1 silicone drainage tube, which was then implanted beside the wound and placed to lie vertically for the holes to point towards the soft tissue bed and the damaged bone segment near the bottom of the wound. This tube was used for alternate rinsing with saline and Anerdian, and for VSD (Wuhan VSD Medical Instrument Co., Ltd.). VSD was conducted by trimming the VSD dressing and performing an overlapping suture, which covered the exposed wound, and was interruptedly sutured to healthy skin. The wound was then enclosed with biofilm and connected to negative-pressure suction to perform perfusion-flushing.
Post-treatment processing
VSD was performed with central negative-pressure suction of 0.02 to 0.04 kpa. This was followed by rinsing with 3000 ml/d of saline over 3 days for Gustilo type I fractures, 6000 ml/d of saline over 5 days for Gustilo type II fractures, and 9000 ml/d of saline over 7 days for Gustilo type IIIA fractures. Fifty ml of Anerdian (type III, diluted 10 fold) was added through the abovementioned silicone tube once per day. During this procedure, the VSD negative pressure was properly controlled so that the Anerdian could be drained away following a 3 min rinse and soak of the wound. If the wound bacterial culture and drug sensitivity test were positive, the sensitive drugs were selected for infection treatment. During the procedure, we observed the amount of drainage, looked for leakage around the wound, and examined whether or not the drainage tube was smooth. The suction device was changed after 1 week. The wound was observed for growth of granulation tissue following changing of the tube. If granulation tissue had not completely covered the wound, we replaced the negative-pressure suction device again. If granulation tissue had completely covered the wound, and the granulation tissue was fresh, we performed “stamp” free skin-flap grafting or full-thickness skin grafting followed by compression dressing, or metastatic flap grafting to cover the wound. Radiography was performed 1 month after surgery to observe the growth and condition of the bone graft (Figures 1E-1H).
Observation indicators
We recorded the total time between debridement and bone grafting procedures, time required for granulation tissue to cover the bone graft, time for complete wound and bone healing, duration of hospitalization, and number of debridement procedures.
Criteria of fracture healing
Fractures were considered healed based on the following criteria: (1) no local tenderness or longitudinal percussion pain at the fracture site, or unusual similar joint activity, and (2) continuous bone callus at the small fracture and blurred fracture line on radiography.
Diagnostic criteria of non-union
Non-union was considered to have occurred based on the following criteria: (1) unusual similar joint activity between fracture fragments, (2) radiography findings of separation between fracture segments, with smooth shrinking and less bone callus, and the bone marrow cavity closed with dense sclerotic bone, and (3) non-healing of the fracture within the standard healing time of 9 months post-fracture [14].
Results
Wound healing time
Wound healing time was 5.5 to 10 weeks, with an average of 7.5 weeks. In 20 cases, the VSD tube was replaced once, in 10 cases, it was replaced twice, and in 6 cases, it was replaced 3 times. Time from final debridement to bone grafting was 0 to 5 days, with an average of 4.3 days. Time needed for granulation tissue to completely cover the exposed surface of the bone graft was 3 to 7 weeks, with an average of 3.2 weeks. In 4 cases, we performed skin-flap transferring, and in 12 cases, we performed “stamp” free skin-flap grafting. Patients required 2 to 4 debridement procedures, with an average of 2 procedures per patient. Total hospitalization time was 5 to 12 weeks, with an average of 6.4 weeks.
Bone healing time
Follow-up lasted 5 to 24 months, with an average of 13 months. Bone callus formation started at an average of 3.5 months after surgery. Full bone healing was observed in 26 cases within 3 to 6 months, in 6 cases within 6 to 8 months, in 2 cases within 8 to 12 months, in 1 case at 14 months, and in 1 case at 16 months, with an average of 6.5 months.
Postoperative complications
Thirty-five cases exhibited phase I healing. Pathogens isolated from the wounds of 4 patients were identified and their drug sensitivity determined; these patients were cured by these sensitive drugs. One case exhibited skin necrosis and superficial infection, which was treated by redressing the wound. No internal fixation was exposed, broken, or became loose. Nine cases exhibited infection in the nail tract of the external fixation device, which was controlled by ethanol flushing. One case exhibited superficial cellulitis near the nail tract, which healed when the external fixation device was removed following healing of the fracture. Non-union and osteomyelitis did not occur.
Discussion
Treatment of open bone damage may involve multiple surgeries, long-term hospitalization, significant instability, complicated infection, delayed union, non-union, chronic pain, posttraumatic arthritis, refracture, and additional complications. Because of this, conclusive evidence for proper selection of treatment method is lacking. Controversy also exists regarding whether autologous bone grafting or free bone retention should be performed in phase I to prevent non-union because these procedures might increase risk of infection. To address this problem, we applied VSD and Anerdian type III lavage with free bone retention and iliac bone grafting for treatment of 36 cases of Gustilo types I, III, and IIIA open bone fractures. We achieved positive outcomes, suggesting that this method could be effective to prevent infection, osteomyelitis, delayed union, and non-union. Overall, the effects of this procedure were ideal, with a high union rate and rare occurrence of complications.
Bone grafting is seldom used in the first surgery for open fractures, and is mainly performed in cases with delayed union or non-union [15]. This study advocated bone grafting in the first surgery, using autogenous iliac bone, and obtained satisfactory curative effects. The method used in this study to fill the damaged area of the bone effectively prevented and controlled infection. This eliminated bone collapse and stabilized the end of the fracture. It also allowed the grafted cancellous bone to biologically induce ossification, resulting in positive promotion of fracture healing, which could shorten treatment times, reduce risk and suffering in the patient, and decrease the economic and psychological burdens of this type of injury. Overall, this method could enable early exercise and maximal recovery of limb function and length, and reduce incidence of teratogenicity and mutilation. Early thorough coverage of the wound increased resistance to infection, and may have provided adequate blood supply for bone grafting and promotion of bone healing. A large free bone segment reserved at the grafting site could play an important role towards post-operative fracture healing and functional recovery [16,17].
Gopal et al. reported that the wound infection rate was 6% within 72 hours after closure, and 30% after 72 hours [18]. The method used in this study could significantly reduce the rates of infection and necrosis in a wounded limb, significantly reducing the healing time in the early stages of fracture trauma. Other scholars have proposed a classification method for open fractures [19-21]. Types I, II, and III open fractures use 1 L, 3 L, and 9 L of flushing liquid, respectively. Our results suggest that the Anerdian flushing tube implanted inside the wound prevented clogging of the VSD lumen, thus, achieving all 3 components of the process in 1 treatment, namely, closure, continuous drainage, and controllable negative pressure. This would allow the cavity wall to retract, keeping even pressure on the wound, and closely attaching the tissues to each other. This would result in elimination of dead space and removal of necrotic tissue, inflammatory reactants, and hematomas, thus, achieving adequate drainage and preventing residual fluid-caused infection. The toxins also could be diluted, and the topical antiseptic fluid could be maintained within the lesion at a high concentration for effective antibiotic activity. Meanwhile, mechanical dragging and the neuroendocrine system could promote rapid and healthy growth of granulation tissue, prevent swelling of new granulation tissue, and help to resist bacterial growth, thereby, removing the hindrances to fracture healing, and stimulating and promoting local ossification. This method also could avoid cross-contamination caused by repeated postoperative dressing, reduce the pain caused by medication, reduce the workload of nursing staff, and shorten the treatment time of soft tissue coverage, thus, reducing the length of hospitalization as well as the cost of treatment [11,22-26].
Anerdian (type III) is an alcohol-free mucosal disinfectant that does not irritate the wound. It can be used to wash areas for surgical debridement, oral cavities, the perineum, and the vagina. It has strong antibacterial properties, is fast-acting, and has long-lasting effects. Additionally, its use on topical wounds shows no cytotoxicity. Presently, no Anerdian (type III)- resistant bacterial strains have been found. Most wound infections are caused by a variety of bacteria, and Anerdian (type III) can block this pathologic process, and provide antibacterial effects for 6 hours [27-29]. Through flushing, Anerdian (type III) not only came in direct contact with the bacteria inside the contaminated wound, but also entered the tissue around the incision, thereby, quickly reaching a concentration inside the local tissue that was much higher than the minimal inhibitory concentration. This means it could quickly kill bacteria remaining inside the wound and effectively achieve maximal sterilization.
Application of VSD technology can reduce the use of skin flaps. Parrett et al. showed that during 1992 through 1995, 20% of open fracture cases used a free skin flap to cover the wound [30]. During 1996 through 1999, approximately 11% of open fracture cases used a free skin flap. During 2000 through 2003, the rate of free skin flap use deceased to 5%. Dedmond et al. also showed similar results. This study performed debridement and fixation as quickly as possible for treatment of Gustilo types I, II, and IIIA fractures, as well as phase I wound closure [31]. We then utilized VSD for Anerdian (type III) flushing. Stabilization of the fracture end can avoid movement, thereby, decreasing injury to soft tissue, blood vessels, and nerves. It also can reduce the infection rate, which is favourable for fracture healing and early rehabilitation. However, the choice of fixation remains controversial [32-34]. In a previous study, for Gustilo type III fractures, thin-needle half-ring external fixation was performed after debridement [35]. Due to the greater degree of soft tissue damage, the wound could not be closed directly, thus, the surrounding muscle flap was stretched and sutured to cover the fracture. This was accompanied by VSD with Anerdian (type III) flushing. When the open bone fracture wound became infected, followed by bone exposure and non-union, post-debridement fine-needle half-ring external fixation could be performed, and direct relaxation suturing of the soft tissue was possible along with local skin/muscle flap coverage. This was followed by VSD tube installation for Anerdian (type III) flushing. This process could avoid certain shortcomings, such as phase I fracture infection, long phase II treatment course, and poor function following recovery, and could promote wound healing and increase resistance to infection.
In summary, free bone retention plus iliac bone grafting under phase I VSD lavage for treatment of Gustilo types I, II, and IIIA open bone defects achieved good clinical results. This method could effectively prevent infection and incidence of osteomyelitis, delayed union, and non-union, with a short treatment course, low cost, and convenient procedures. Limitations to this study are its small sample size and lack of a multi-center clinical study group. Additionally, the follow-up time was short. Thus, prospective and large-scale multi-center experiments are necessary. The long-term effects of this treatment also need to be studied further.
References
- Klein S, Hage JJ, Woerdeman LA. Donor-site necrosis following fibula free-flap transplantation: a report of three cases. Microsurgery 2005; 25: 538-542.
- Timmers MS, Graafland N, Bernards AT, Nelissen RG, van Dissel JT, Jukema GN. Negative pressure wound treatment with polyvinyl alcohol foam and polyhexanide antiseptic solution instillation in posttraumatic osteomyelitis. Wound Repair Regen 2009; 17: 278-286.
- Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of themtibia: Current management concepts. J Am Acad Orthop Surg 2005; 13: 417-427.
- Pape HC, Evans A, Kobbe P. Autologous bone graft: properties and techniques. J Orthop Trauma 2010; 24: 36-40.
- Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmol 2002; 109: 13-24.
- Barkana Y, Almer Z, Segal O, Lazarovitch Z, Avni I, Zadok D. Reduction of conjunctival bacterial flora by povidone-iodine, ofloxacin and chlorhexidine In an outpatient setting. Acta Ophthalmol Scand 2005; 83: 360-363.
- Montan PG, Setterquist H, Marcusson E, Rylander M, Ransjo U. Preoperative gentamicin eye drops and chlorhexidine solution in cataract surgery. Experimental and clinical results. Eur J Ophthalmo1 2000; 10: 286-292.
- Wu PC, Li M, Chang SJ, Teng MC, Yow SG, Shin SJ, Kuo HK. Risk of endophthalmitis after cataract surgery using different protocols for povidone-iodine preoperative disinfection. J Ocul Pharmacol Ther 2006; 22: 54-61.
- Freeland AE, Mutz SB. Posterior bone-grafting for infected un-united fracture of the tibia. J Bone Joint Surg Am 1976; 58: 653-657.
- Tropet Y, Garbuio P, Obert L, Jeunet L, Elias B. One-stage emergency treatment of open grade IIIB tibial shaft fractures with bone loss. Ann Plast Surg 2001; 46: 113-119.
- Lavery LA, La Fontaine J, Thakral G, Kim PJ, Bhavan K, Davis KE. Randomized clinical trial to compare negative-pressure wound therapy approaches with low and high pressure, silicone-coated dressing, and polyurethane foam dressing. Plast Reconstr Surg 2014; 133: 722-726.
- Zhang WK, Zhang WK, Wang HB, Mao GL, Li J. Vacuum sealing drainage and free coupling chain-link posterior tibial artery flap in the reconstruction of degloving injury of propodium. Zhonghua Zheng Xing Wai Ke Za Zhi 2013; 29: 258-260.
- Qu J, Yan R, Wang L, Wu J, Cao L, Zhao G, Sun K, Zhang L, DU X, Peng Y, Li S, Ma H, Gao J, Liu H. Free dermatoplasty combined with vacuum sealing drainage for the treatment of large-area soft tissue defects accompanied by bone exposure in the lower leg. Exp Ther Med 2013; 5: 1375-1380.
- Volpin G, Shtarker H. Management of delayed union, non-union and mal-union of long bone fractures. Eur Surg Orthop Traumatol 2014; 241-266.
- Browner BD, Jupiter JB, Trafton PG. Skektal trauma. Beijing Sci Press (2nd edn.) 2001; 2295.
- Kanakaris NK, Paliobeis C, Nlanidakis N, Giannoudis PV. Biological enhancement of tibial diaphyseal aseptic non-unions: the efficacy of autologous bone grafting, BMPs and reaming by-products. Injury 2007; 38: 65-75.
- Khan SN, Cammisa FP Jr, Sandhu HS, Diwan AD, Girardi FP. The biology of bone grafting. J Am Acad Orthop Surg 2005; 13: 77-86.
- Weitz-Marshall AD, Bosse MJ. Timing of closure of open fractures. J Am Acad Orthop Surg 2002; 10: 379-384.
- Anglen JO. Wound irrigation in musculoskeletal injury. J Am Acad Orthop Surg 2001; 9: 219-226.
- Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg (Am) 1976; 58: 453-458.
- Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 1984; 24: 742-746.
- Li RG, Yu B, Wang G, Chen B, Qin CH, Guo G, Jin D, Ren GH. Sequential therapy of vacuum sealing drainage and free-flap transplantation for children with extensive soft-tissue defects below the knee in the extremities. Injury 2012; 43: 822-828.
- Korkmaz MF, Erdem MN, Disli Z, Selcuk EB, Karakaplan M, Gogus A. Outcomes of trochanteric femoral fractures treated with proximal femoral nail: an analysis of 100 consecutive cases. Clin Interv Aging 2014; 9: 569-574.
- Gavaskar AS, Subramanian M, Tummala NC. Results of proximal femur nail antirotation for low velocity trochanteric fractures in elderly. Indian J Orthop 2012; 46: 556-560.
- Li RG, Ren GH, Tan XJ, Yu B, Hu JJ. Free flap transplantation combined with skin grafting and vacuum sealing drainage for repair of circumferential or sub-circumferential soft-tissue wounds of the lower leg. Med Sci Monit 2013; 19: 510-517.
- Ferguson PJ, Sandu M. Current understanding of the pathogenesis and management of chronic recurrent multifocal osteomyelitis. Curr Rheumatol Rep 2012; 14: 130-141.
- Winter GD. Formation of the scab and the rate of epithelisation of superficial wounds in the skin of the young domestic pig. J Wound Care 1995; 4: 366-367.
- Huang HC, Lin SB, Li GH, Zhang SB. Sterilizing effects of 5% Anerdian type 3 disinfectant dilution used in conjunctival sac before cataract surgery. Chinese J Pract Ophthalmol 2009; 6: 616-619.
- Zamora JL. Chemical and microbiologic characteristics and toxicity of povidone-iodine solutions. Am J Surg 1986; 151: 400-406.
- Parrett BM, Matros E, Pribaz JJ, Orgill DP. Lower extremity trauma: trends in the management of soft-tissue reconstruction of open tibia-fibula fractures. Plast Reconstr Surg 2006; 117: 1315-1322.
- Dedmond BT, Kortesis B, Punger K, Simpson J, Argenta J, Kulp B, Morykwas M, Webb LX. The use of negative-pressure wound therapy (NPWT) in the temporary treatment of soft-tissue injuries associated with high-energy open tibial shaft fractures. J Orthop Trauma 2007; 21: 11-17.
- Menon DK, Dougall TW, Pool RD, Simonis RB. Augmentative Ilizarov external fixation after failure of diaphyseal union with intramedullary nailing. J Orthop Trauma 2002; 16: 491-497.
- El-Karef E, Sadek HI, Nairn DS, Aldam CH, Allen PW. Triplane fracture of the distal tibia. Injury 2000; 31: 729-736.
- Beaty JH. Operative treatment of femoral shaft fractures in children and adolescents. Clin Orthop Relat Res 2005; 114-122.
- Emara KM, Ghafar KA, Al Kersh MA. Methods to shorten the duration of an external fixator in the management of tibial infections. World J Orthop 2011; 2: 85-92.