Research Article - Journal of Finance and Marketing (2019) Volume 3, Issue 1
Financial soundness of deposit money banks in Nigeria: The camels model approach.
David Ayebare1*, Aloysius Rukundo2*, Edgar Mugema Mulogo3, Moses Ntaro3, Imelda K3 and Gad Ndaruhutse Ruzaaza31Interdisciplinary Research and Development Center (IRDC) LTD, Uganda
2Department of Educational Foundations and Psychology, Mbarara University of Science and Technology, Uganda
3Department of Community Health, Mbarara University of Science and Technology, Uganda
- *Corresponding Author:
- David Ayebare Santson
Interdisciplinary Research and Development Center (IRDC) LTD, Uganda
Tel: +256776949207
E-mail: ayebaredavid@gmail.com
Aloysius Rukundo
Department of Educational Foundations and Psychology
Mbarara University of Science and Technology, Uganda
E-mail: arukundo@must.ac.ug
Received date: December 04, 2018; Accepted date: January 24, 2019; Published date: January 29, 2019
Citation: Ayebare D, Rukundo A, Mulogo EM, Ntaro M, Imelda K, et al. (2019) Prediction of Risky Alcohol Use among Ugandan Youth: A Case Study of at Marie Stopes and Youth Reproductive Health Clinics. J Alcohol Drug Depend 7: 322. doi:10.4172/2329-6488.1000322
Copyright: © 2019 Ayebare D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The objective of this paper is to analyze the performance of 10 selected deposit money banks in Nigeria using the simple random sampling technique over a period of fifteen years (2000-2015). The data were sourced from the audited annual reports from the Nigerian Stock Exchange. For this purpose, CAMELS model was used. The CAMELS model established that six of the banks namely; Banks A, B, C, D, E and G were graded as satisfactory (scale point 2) in their general performances based on the 5 point likert scale where 1 is the highest and 5 is the lowest whereas 4 banks; Banks F, H, I and J were graded as fair (scale point 3) indicating that their performances are less than satisfactory. The study went further to test the significant relationship among the variables in the CAMELS model using the Friedman rank test, the result showed that there are significant relationships in capital adequacy, asset quality, management quality, earnings, liquidity ratio and sensitivity among the banks, indicating that the banks are operating at different levels of investment. Based on the findings the following recommendations were made; bank managers should focus on ensuring that their banks are well capitalized, minimize levels of non-performing loans, maintain sound management and ensure adequate liquidity so as to sustain banks’ financial soundness and mitigate vulnerability of banks.
Keywords:
Alcohol use; Alcohol misuse and youth; Marie Stopes clinic; Youth reproductive health clinic; Uganda
Background
Alcohol use remains a global burden of disease [1]. The level of alcohol use among the youth is a public health problem in Sub-Saharan Africa, is high and increasing among youth [2]. In the Global Schoolbased (GSBHS) survey in Uganda, 64% of youth in schools reported alcohol use [3]. In the recent years, the age of alcohol use has changed, such that slightly more young people (ages 15-24 years) report higher alcohol use than older ages. Moreover, youth who use alcohol experience social problems such as school dropout [4], economic and mental health problems. Further, they are more likely to have fatal accidents. A study conducted in Mbarara Regional Referral Hospital revealed that more than 14% deaths were attributed to alcohol-related accidents.
It is reported that more than 64.5% of the patients in Kampala health facilities attributed their illness to alcohol use [5]. Furthermore, 13.5% of the road accidents in Uganda are a result of alcohol use [6]. However, some health settings have little data on alcohol use among the youth.. Despite the high level of alcohol use among the youth, few studies have explored the level and risk factors of alcohol use, especially among the youth that attend youth-friendly health care centres in Sub-Saharan Africa [7]. Although alcohol use is generally low among the youth in school settings, it remains unacceptably high among out-of-school youth. In Kenya, the rates of alcohol use among the youth have been reported at 20.6% [8]. A study by [3] conducted in Uganda revealed the prevalence of alcohol use among the youth in schools to be 64%. These studies, among others identified alcohol use by peers, other substance use and family misuse as risk factors for alcohol use among the youth. In addition, socio- cultural influences justify alcohol use among the youth in Uganda.
As regards socio-cultural factors, sports galas and marriage ceremonies for instance expose the youth to alcohol use. Such influences make alcohol to be indiscriminately accessible to the youth in almost all places [9-11]. Worse still, a number of acts such as the Enguli Act (1964) that were put in place to regulate alcohol use are not only old but rarely enforced [10]. Enguli act (1964) was enacted to regulate use of illicit home-distilled alcohol in Uganda.
In addition, there is paucity of empirical evidence regarding the factors associated with alcohol use among the youth seeking health services. Consequently, there are no specific efforts for interventions to regulate alcohol use among the youth in Uganda. This study bridges the gap by assessing alcohol use among youth seeking health services from RHU and MSU clinics. Due to the numerous and greater than before consequences associated with alcohol use, it is imperative to understand the prevalence of and risk factors associated with alcohol use among the youth in Uganda. This understanding could inform new policies and interventions to mitigate the negative consequences of alcohol use among the youth. Therefore, the objective of this study was to determine the level and risk factors of alcohol use among the youth seeking health services at Marie Stopes Uganda (MSU) and Reproductive Health Uganda (RHU) clinics in Mbarara Municipality, Southwestern Uganda.
Methods
Study design
This was a descriptive, cross sectional study conducted at Marie Stopes Uganda (MSU) and Reproductive Health Uganda (RHU) Clinics in Mbarara Municipality, southwestern Uganda.
Study population and ethics
All the youth presenting to the MSU and RHU clinics for health care services between August 1, 2012 and September 1, 2012 were eligible for inclusion in the study. This study was approved by the Mbarara University of Science and Technology Review Ethics Committee of (MUST-REC). Written consent was sought after receiving health care services.
Study site
The study was conducted at MSU and RHU Clinics in Mbarara Municipality, southwestern Uganda. The two clinics are situated in the centre of Mbarara Municipality and are ‘drop-in’ centres offering cheap reproductive health services (RHS). Drop-in centres are areas designated for provision of specialized healthcare and social care services to at-risk populations such as the youth. The services provided by these centres purposively attract and support young people who do not attend school. The young people in this case include boda boda riders (commercial motorcyclists), mobile artists and shoe shiners among others. Some members of these groups are then trained as peer educators on sexual Reproductive Services and then commissioned to pass on their learning to the local community of origin.
Eligibility
The youth of ages 15-24 years, seeking sexual reproductive health services were consecutively recruited from the outpatient register in MSU and RHU clinics. Youth were excluded if they were too sick, as they were not able to give sound informed consent. Alternate visits were made until the sample size was obtained.
Procedure
Following consent and reception of respondents, a pretested questionnaire was administered to the consenting youth. The questionnaire was administered to elicit demographic characteristics and risks of alcohol use among the youth. Use of alcohol one year prior to the study was assessed. Participants Youth received the, previously validated screening tool (audit) for alcohol use [13]. A standard drink was eight grams of alcohol per drink [12]. The scale consists of 10 items scored on 0-40 points, with total AUDIT score categories as follows: non-drinkers (0), social drinkers (1-7) and alcohol abusers/ dependence (8-40) as defined by WHO-ICD 10.
Outcome
The primary outcome of this study was the proportion of study participants in each level of alcohol use as defined by AUDIT, to at least one standard drink as determined by self-report.
Sample size
There is no data reporting the prevalence of alcohol use among the youth seeking SRH services in Mbarara Municipality, thus precise estimates of the sample size for this study was not possible. However, a total of 336 youth were recruited.
Analysis
Descriptive statistics were used for reporting the primary study outcomes. To test for associations, predictor factors were crosstabulated with dichotomized alcohol use (alcohol drinkers and alcohol non-drinkers) through bivariate logistic regression. Independent variables with p ≤ 0.05 were entered into the multivariate logistic regression. Odds ratios, p values and confidence intervals are reported. l The analyses were conducted using stata 12.0.
Results
Subjective characteristics
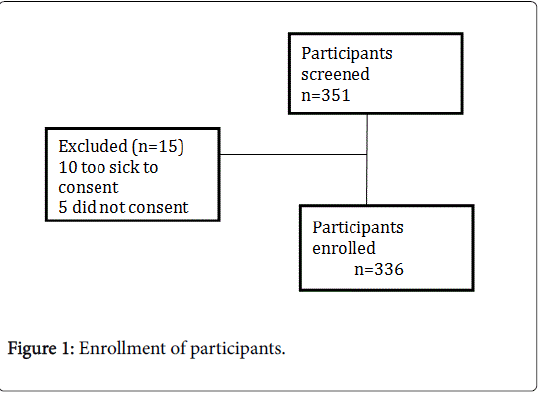
During the study period, 351 youth were screened for enrolment. Ten youth were excluded as they were too sick to consent. Five youth did not consent and were also excluded (Figure 1). Overall, 336 youth were enrolled in the study with a mean of 19 years (Table 1). Out-ofschool youth (n=250, 74%) with at least secondary education (n=270, 80%) were more represented, but comparably youth with almost equal gender (n=171, 51% females) was enrolled (Table 1).
| Participant characteristics | Mean ± SD or N (%) |
|---|---|
| Gender | |
| Females | 171 (50.9) |
| Age (years) | 19.2 (± 2.9) |
| Marital status | |
| Married | 18 (5.4) |
| Cohabiting | 113 (33.6) |
| Single | 194 (3.3) |
| Family structure | |
| Father only | 33 (9.8) |
| Mother only | 26 (7.7) |
| Both parents | 182 (71.7) |
| Neither parent | 95 (10.8) |
| Highest level of education | |
| P1-P4 | 11 (3.3) |
| P5- P7 | 55 (16.6) |
| At least Secondary | 270 (80.4) |
| Schooling status | |
| Non-student | 250 (74.4) |
| Employment status | |
| Not employed | 163 (48.5) |
Table 1: Baseline characteristics of youth enrolled in the study (n=336).
Level of alcohol use by questionnaire
Among the 336 youth enrolled in the study, the proportion of youth who reported any alcohol use was 80% (n=270). 57.4 % (n=193) of the youth reported alcohol use to at least one standard drink per sitting on average (as defined by AUDIT) in the 12 months prior to the study.
Alcohol abuse/dependence (Total AUDIT score 8-40) was less common, reported by 4.5% (n=15) of the study participants (Table 2).
| Level of alcohol Use | Non-drinkers, n (%) | Social Drinkers, n (%) | Alcohol Abusers, n (%) | Total |
|---|---|---|---|---|
| Gender | ||||
| Female | 63 (38.2) | 94 (57.0) | 8 (4.9) | 171 |
| Male | 80 (46.6) | 84 (49.1) | 7 (4.1) | 165 |
| Age (years) | ||||
| 15-17 | 60 (50.0) | 55 (45.8) | 5 (4.2) | 120 |
| 18-24 | 83 (38.4) | 123 (57.0) | 10 (4.6) | 216 |
| Total | 143 (42.6%) | 178 (53%) | 15 (4.5%) | 336 |
Table 2: Level of alcohol use among youth enrolled in the study (n=336).
Of the 193 youth who reported alcohol abuse/dependence, 4.9% (n=8) were females compared to 4.1% (n=7) males. In total, 53% (n=178) youth were social drinkers.
Predictors of alcohol use
Residing closer to the source of alcohol in the past fortnight was the strongest risk factor of alcohol use among the youth (Table 3). Youth reporting source of alcohol in less than half a kilometer had a higher odds of alcohol use (OR: 8.0, 95%CI: 2.5-11.4, p<0.01). In addition, history of familial alcohol misuse was statistically associated with alcohol use; parents (OR: 3.3, 95%CI: 1.2-5.0) and aunt/uncle (OR: 3.9, 95%CI: 1.1-10.2, p<0.01, p <0.01) and siblings (OR: 1.3, 95%CI: 0.5-1.9). Other substance use by the youth was also statistically associated with alcohol use (OR: 3.0, 95%CI: 1.1-5.9, p<0.04). More so employed youth had a higher odds of alcohol use (OR: 1.8, 95%CI: 1.3-3.3, p<0.01). Though statistically significant at bivariate analysis, sadness and having peers involved in alcohol use were insignificant risk factors of alcohol use in the multivariate analysis.
| Variable | Alcohol Drinkers | UOR (95%CI) | p | AOR (95%CI) | p |
|---|---|---|---|---|---|
| Schooling Status | Student | Reference | 0.05 | Reference | 0.6 |
| Non-student | 1.7 (1.1-3.3) | 1.3 (0.4-2.5) | |||
| Employment Status | Not employed | Reference | |||
| Employed | 2.0 (1.3-3.4) | 0.001 | 1.8 (1.3-3.3) | 0.01* | |
| Sadness | Yes | 2.4 (1.2-5.0) | 0.02 | 2.7 (0.4-2.1) | 0.66 |
| Alcoholic Peers | Yes | 2.9 (1.7-4.7) | 0.001 | 2.9 (0.3-10.2) | 0.26 |
| Substance Use | Yes | 2.8 (1.4-6.4) | 0.03 | 3.0 (1.1-5.9) | 0.04 |
| Alcohol Misuse in Family | None | Reference | 0.04 | Reference | 0.01* |
| Parent (F/M) | 2.9 (1.4-4.8) | 3.3 (1.2-5.0) | |||
| Siblings | 2.1 (1.0-5.0) | 1.3 (0.5-1.9) | |||
| Aunt/Uncle | 3.5 (1.4-10.1) | 3.9 (1.1-10.2) | |||
| Proximity to the source of alcohol | >1 Km | Reference | 0.004 | Reference | 0.001* |
| <½ Km | 7.8 (5.1-10.2) | 8.0 (2.5-11.4) | |||
| ½ Km-1 Km | 7.3 (5.0-9.9) | 6.5 (4.6-8.9) |
Table 3: Risk factors of alcohol use among youth enrolled in the study (n=336). N=336; *p<0.01; **p<0.001.
Discussion
We performed a descriptive study to investigate the level of alcohol use among the youth seeking health services at MSU and RHU clinics in southwestern Uganda. The proportion of ‘any alcohol use’ in our study was high, and over half of the youth were social drinkers. Interestingly, the prevalence of alcohol use was higher than that reported by the UDHS, (2011).
A previous study performed in Uganda among the youth of ages 13-15 examining the prevalence of alcohol use in schools reported that the rate of alcohol use was 64% [13]. Therefore the prevalence of alcohol use reported in the present study differs from the results recorded by [13]. The differences in socio-demographic characteristics of the youth, however, may explain this discrepancy as subjects in our study represented out-of- school youth. Furthermore, in contrast to [13], the present study considered youth seeking health services from clinics.
Earlier studies in Uganda though in different settings revealed similar findings regarding factors influencing alcohol use among the youth [10,11]. As regards the factors influencing alcohol use, we found that residing closer to the source of alcohol; familial alcohol misuse; other substance use and being employed were the strongest risk factors for alcohol use among the youth. While age, sadness and having peers involved in alcohol use had higher non-significant odds, these factors are considered a risk for alcohol use [9,11]. These factors are reflected by the Theory of Reasoned Action, which proposes that one’s subjective norms and attitudes about alcohol use determine behavioral intention and behavioral action [13]. Moreover, youth with uninhibited subjective norms may have higher odds of alcohol use. Our findings imply that improved understanding of the association between alcohol use and health service seeking behavior is needed to sufficiently appreciate youth health issues.
Limitation
The main limitation was the cross sectional nature of the study. However, this was minimized by use of a standard AUDIT tool already validated for use in Uganda.
Conclusion
The prevalence of alcohol use among the youth was high. This high prevalence could be mainly due to socio-cultural activities the youth engage in. The main risk factors for alcohol use were other substance use, proximity, familial alcohol misuse, and being employed.
Recommendation
Clinic-based prevention of alcohol use in youth friendly clinics needed in Mbarara Municipality and beyond.
Competing Interests
The authors hereby declare that they have no competing interests.
Funding
No funding was received from the external source. The corresponding author used his meager resources.
References
- Uganda Youth Development Link (UYDEL) State of alcohol abuse in Uganda. Kampala: UYDEL, 2008.
- Kabiru CW, Beguy D, Ndugwa RP, Zulu EM, Jessor R (2017) Successful adolescence in the slums of Nairobi, Kenya. Problem Behavior Theory and the Social Context: The Collected Works of Richard Jessor 3: 117.
- Ministry of Health (2004) Global school based student health survey 2003-Uganda Country Report. Kampala: Ministry of Health.
- Mukama E (2010) Peer group influence, alcohol consumption, and secondary school students?attitudes towards School. Kampala: Makerere University.
- Kullgren G, Alibusa S, Birabwa-Oketcho H (2009) Problem drinking among patients attending primary health care units in Kampala, Uganda. Afr J Psychiatry (Johannesbg) 12: 52-58
- Masaba S (2013) Only half of traffic offenders actually pay express penalties. nature of accidents. New Vision. 2013 Saturday, 3rd August.
- Livingstone S, Nandi A, Banaji S, Stoilova M (2017) Young adolescents and digital media: uses, risks and opportunities in low-and middle-income countries: a rapid evidence review.
- Olumide OS (2017) Access barriers to Campus Health Services among University of Venda students.
- Kafuko A, Butuluki P (2008) Qualitative Research in Uganda on Knowledge, Attitudes and Practices Concerning Alcohol.
- Tumwesigye N, Kasirye R, Nansubuga E (2009) Is social interaction associated with alcohol consumption in Uganda? Drug Alcohol Dependence 103: 9-15.
- Karamagi C, Tumwine J (2006) Intimate partner violence against women in eastern Uganda: implications for hiv prevention. BMC Public Health 20: 284-296.
- Babor F, Biddle-Higgins C, Saunders B, Monterio G (2005) The alcohol use disorders identification test (audit): guidelines for use in primary care. 2nd ed. Geneva: WHO.
- Madden TJ, Ellen PS, Ajzen I (1992) A comparison of the theory of planned behavior and the theory of reasoned action. Pers Soc Psychol Bull 18: 3-9.