Case Report - Journal of Pregnancy and Neonatal Medicine (2024) Volume 8, Issue 4
Fetal Cardiac Rhabdomyoma: Case Report and Literature Review
Gabriel E. Villagómez-Martínez*, Paola B. Ploneda -Espinosa de los Monteros, Jessica Gabriela Arias Molina, Adriana Cisneros-Martinez, Juan A. Soria-López, Abel Guzmán-López, Luis Abel Guzman Ochoa, Clara del C. Flores-AcostaDr. Jose Eleuterio Gonzalez University Hospital, Mexico
- *Corresponding Author:
- Gabriel E. Villagómez-Martínez
Dr. Jose Eleuterio Gonzalez University Hospital
Mexico
E-mail: paolabespinosa@gmail.com
Received: 03-Aug-2024, Manuscript No. AAPNM-24-146855; Editor assigned: 05-Aug-2024, PreQC No. AAPNM-24-146855 (PQ); Reviewed: 19-Aug-2024, QC No. AAPNM-24-146855; Revised: 24-Aug-2024, Manuscript No. AAPNM-24-146855(R); Published: 31-Aug-2024, DOI: 10.35841/aapnm-8.4.211
Citation: Gabriel E. Villagómez-Martínez. Fetal cardiac rhabdomyoma: Case report and literature review. J Preg Neonatal Med. 2024;8(4):211
Introduction
Rhabdomyomas are rare benign cardiac tumors that mainly occur in infancy and can be detected prenatally through fetal ultrasound. We present a case of fetal cardiac rhabdomyoma diagnosed during prenatal ultrasound examination.
Case
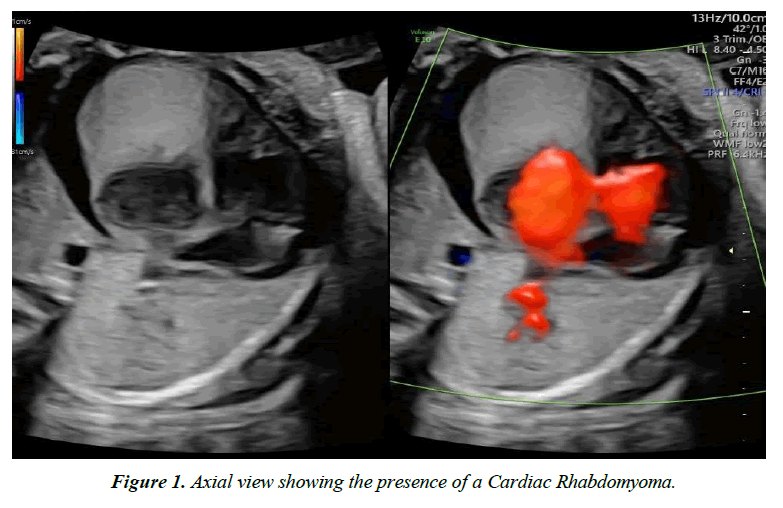
A 19-year-old gravid patient underwent routine obstetric ultrasound at 29.4 weeks of gestation, revealing the presence of a hypoechoic intracardiac mass measuring 26x26 mm with pericardial effusion in the fetus (Figure 1). She was referred to our institution, where the presence of an intracardiac mass was confirmed by fetal echocardiography, adding the diagnoses of cardiac rhabdomyoma, severe cardiomegaly, and mild tricuspid regurgitation. Fetal magnetic resonance imaging was requested, confirming the diagnosis of cardiac rhabdomyoma, and genetic evaluation was sought [1]. Clinical History: During prenatal follow-up, the patient remained asymptomatic. However, progressive growth of the rhabdomyoma was observed in subsequent ultrasound examinations, with dimensions of 31x23x36 mm and severe pericardial effusion. A neurosonography revealed multiple hyperechoic images in the cerebral parenchyma compatible with tuberous sclerosis, a genetic disease commonly associated with cardiac rhabdomyomas. Given the risk of hemodynamic complications for the fetus due to the size and location of the tumor, the possibility of fetal intervention was discussed with the multidisciplinary team [2].
Treatment
It was decided to initiate treatment with Sirolimus, an mTOR inhibitor known for its effectiveness in the treatment of cardiac rhabdomyomas. Controlled doses of Sirolimus were administered under the supervision of a neonatologist specialized in pediatric cardiology, with serial serum evaluations of Sirolimus levels [3].
Results
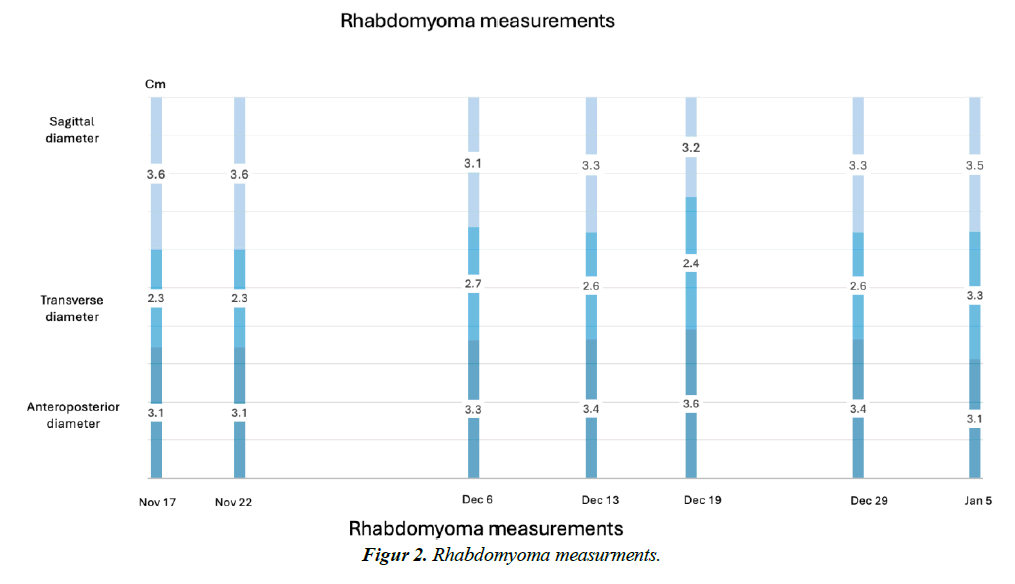
Sirolimus therapy was successful, as the tumor showed no signs of growth during follow-up (Figure 2). This resulted in a significant improvement in fetal cardiac function and a reduction in the risk of hemodynamic complications for the fetus. However, the fetus continued to have severe pericardial effusion, prompting an uncomplicated pericardiocentesis with drainage of 25 mL [4]. The effusion remained absent for the remainder of the gestation. One week later, the Sirolimus dose was increased, contributing to the maintenance of tumor dimensions and overall treatment success. The patient delivered a term neonate via abdominal delivery without complications. The neonate underwent postnatal cardiac and neurological evaluation, confirming the previously described findings, showing normal cardiac function and the absence of complications related to the rhabdomyoma [5].
Conclusion
Fetal cardiac rhabdomyoma is a rare but important entity that should be considered in the prenatal diagnosis of intracardiac masses. The association with tuberous sclerosis highlights the importance of a multidisciplinary approach in managing these cases. Sirolimus treatment may be an effective therapeutic option for reducing tumor size and improving perinatal outcomes.
What's known/what's new statements
What's already known about this topic?
Sirolimus has been used effectively in treating cardiac rhabdomyomas in fetuses, offering a non-surgical therapeutic option that can lead to the reduction or stabilization of tumor size, thereby improving fetal cardiac function and outcomes.
What does this study add?
This study provides further evidence of sirolimus's efficacy and
safety in managing fetal cardiac rhabdomyomas, highlighting its potential as a standard treatment option for this rare and challenging condition.
References
- Cavalcante CT, Pinto Junior VC, Pompeu RG, et al. Perinatal unusual rhabdomyoma location–case report and systematic reviews of the literature. J Matern Fetal Neonatal Med. 2021;34(1):137-51.
- Pruksanusak N, Suntharasaj T, Suwanrath C, et al. Fetal cardiac rhabdomyoma with hydrops fetalis: report of 2 cases and literature review. J Ultrasound Med. 2012;31(11):1821-4.
- Chao AS, Chao A, Wang TH, et al. Outcome of antenatally diagnosed cardiac rhabdomyoma: case series and a meta‐analysis. Ultrasound Obstet Gynecol. 2008;31(3):289-95.
- Walsh SN, Hurt MA. Cutaneous fetal rhabdomyoma: a case report and historical review of the literature. Am J Surg Pathol. 2008;32(3):485-91.
- Li HF, Wang D, Li JQ, et al. Tuberous sclerosis complex secondary to the presence of fetal cardiac rhabdomyoma: a case report and literature review. MFM. 2020;2(04):240-3.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref