Research Article - Biomedical Research (2017) Volume 28, Issue 11
Fetal anomalies detection in China by screening with ultrasound
Shuang Liu1, Qingqing Wu1 and Zhaojuan Chen2*
1Department of Ultrasound, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing, PR China
2Department of Obstetrics, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing, PR China
- *Corresponding Author:
- Zhaojuan Chen
Department of Obstetrics
Beijing Obstetrics and Gynecology Hospital
Capital Medical University, Beijing, PR China
Accepted date: March 27, 2017
Abstract
Purpose: To correlate sonographic findings of fetal developmental abnormalities resulting from chromosomal aberrations and structural anomalies in 2nd trimester. Design: Cross-sectional study. Setting: Tertiary care centre.
Patients and Methods: Amid the reporting period from August 2007 to July 2014, prenatal fetal anomaly diagnosis in 9524 fetuses/babies were inspected and contrasted with post-natal diagnosis.
Results: Overall, 233 fetuses/babies had affirmed anomalies, prevalence 2.45%. Out of those fetuses/ babies, 22.31% (52/233) had chromosomal anomalies, prevalence 0.55%, and 78% (181/233) had ordinary chromosomes along with structural anomalies (major (43.64%; 79/181) and minor (56.35%; 102/181)), prevalence 1.9%. The affirmed anomalies distinguished prenatally were 102, giving a total sensitivity for prenatal fetal anomaly detection of 43.78% (102/233; 95% Confidence Interval (CI) 37.31-49.98), specificity of 99.95%, PPV of 95.33% and NPV of 98.61%. The aggregate detection rate prior to 22 gestation weeks was 40.34% (94/233; 95% CI 33.99-46.95). The pre-natal detection rate of chromosomal anomalies was 61.5% (32/52) and for structural anomalies, 38.7% (70/181).
Conclusion: In a routine clinical setting at a hospital, half of major structural anomalies in fetuses with normal chromosomes are identified by standard ultrasound exam in 2nd trimester. Chromosomal anomalies have the greatest probability for prenatal detection; the greater part is diagnosed by amniocentesis prior to standard ultrasound exam in high-risk women.
Keywords
Congenital malformations, Fetal anomalies, Pregnancy, Prenatal diagnosis, Ultrasound
Introduction
Screening with ultrasound on routine basis during second trimester was a segment of maternity healthcare in various developing countries. In China, pregnant women undergo maternal-fetal medicine ultrasound screening ahead of schedule in the second trimester, and it will be conducted by radiologists and obstetricians and infrequently by midwives, who received special training [1-4]. The efficacy of ultrasound test for fetal anomalies depends on various factors, like gestational age, experience and skillset of operators, equipment, and possibility of repeat scan [3,5,6]. At first, the fundamental explanations behind routine ultrasound test were evaluating age at gestation, assessing the viable fetus number and research of placenta. At present, fetal anomalies screening, utilizing a checklist has turned into a vital part of the test at the greater part of obstetrical offices.
Pre-birth identification of fetal anomalies varies from 17% to 85% [7,8]. Greater contrasts in study setting crucially affect sensitivity. Most of the studies were conducted in tertiary care centers [3,7-10], that might give distinctive rates of identification than small healthcare centers with respect to prevalence, resources, and competency in detection of anomalies. The Helsinki Ultrasound Trial demonstrated huge contrasts in prenatal identification rates of major abnormalities at tertiary care center in comparison with city local hospital [11], whereas other studies demonstrated that individual clinics can accomplish identification rates comparably with that of tertiary centers [12,13]. A large portion of these studies were publicized or based upon information gathered over 10 years prior. Notwithstanding information in the field, the specialized equipment and conceivable outcomes for distinguishing chromosomal anomalies have enhanced throughout the years, so consequent studies might demonstrate high recognition rates.
The major goal of the present study was to correlate sonographic findings of fetal developmental abnormalities resulting from chromosomal aberrations and structural anomalies in a tertiary hospital in China.
Methods
This single-center retrospective cross-sectional study was performed at a tertiary hospital, China over a period of seven years from August 2007 to July 2014, and incorporated all delivered babies at the hospital, and those delivered at different hospitals as a result of a prenatal fetal anomaly diagnosis in our hospital. Also included were lost fetus by pregnancy termination, miscarriage, or intrauterine death with fetal anomalies detected through ultrasound in our hospital. All the fetuses incorporated in present study have gone through ultrasound test at the hospital prior to 22 gestation weeks. The overall study population included 9524 fetuses as well as newborns. The Institutional ethics committee approval was acquired for the present study, and patient confidentiality was strictly maintained.
Around 95% of pregnant women residents of area eventually give birth at our hospital. The standard ultrasound exams were conducted by midwives who received special training and infrequently by obstetricians. Two obstetricians and five midwives with skill in ultrasound examination of fetus and with vast experiences were involved during study timeframe. All tests were conducted trans-abdominally. Ultrasound scanners utilized were Antares and Acuson X300 (Siemens Acuson Inc., CA, USA) with 3.5 to 5 MHz multi frequency curvilinear transducers. The allotted exam time was 30 min. Fetal bi parietal diameter as well as femur length were used for calculation of gestational age [14]. The test consisted of fetal anomaly screening utilizing a checklist. The structures that were examined were as follows: fetal brain as well as skull (mid-line echo, shape, cavum septum pellucidi, ventricles, cerebellomedullaris cistern, and cerebellum), spine (3 planes), neck, face, diaphragm, heart, thorax, stomach, umbilical cord insertion and bladder, abdominal wall, kidneys, hands, legs, feet, arms, and skeleton. Extra ultrasound exams were just conducted considering medical indications.
At the point when an anomaly was suspected amid standard scan, the pregnant women were referred to obstetricians with skills in fetal ultrasound exam, for further analysis. Whenever the suspected anomaly was not affirmed by obstetricians or referral center, the fetus was deemed to have ordinary anatomy at standard ultrasound exam.
All the pregnant women>34 years of age, those having riskfactors apart from advanced maternal age, and those with ultrasound tests showing chromosomal abnormalities were provided chromosomal analysis post 15 gestational weeks apart from the standard ultrasound exam in second trimester. From 2007 until May 2010, all pregnant women>34 years of age were principally provided amniocenteses. Beginning May 2010, these pregnant women were at first given first trimester ultrasound test screening for 21, 18, and 13 trisomies, respectively along with nuchal translucency thickness, pregnancy associated plasma protein A and serum free β human chorionic-gonadotropin assessments at 11 to 13 gestation weeks for evaluation of chromosomal abnormality probability. Further chromosomal analysis was done with greater probability (>1/200).
Post birth, all the new-borns were routinely analysed by doctors and were followed-up with respect to congenital anomalies until their discharge from post-natal care or till last diagnosis.
Data on babies getting congenital anomaly diagnosis at postpartum as well as neonatal wards were continually sent to ultrasound unit. Information on all the pre- and post-natal anomaly diagnosis was in prospective storage at ultrasound unit. Comparison was made with those data with that of the congenital anomaly diagnosis specified prior to discharge from post-natal care in hospital databases as per International Classification of Diseases 10th Revision. In the situations of pregnancy termination, miscarriage, or intrauterine death due to fetal anomaly diagnosis prior to ievent, results were recovered from chromosomal analysis as well as pathology/ anatomy exams.
All fetuses/babies were allocated just a single anomaly diagnosis though multiple abnormalities were presented, unless it doesn’t come under multiple malformations sequence/ syndrome. In case of multiple abnormalities, the fetuses/babies were allocated primary diagnosis of the anomaly, considered by authors to be of clinical significant. Chromosomal anomalies were constantly viewed as superior to the structural malformations in babies with irregular chromosomes, aside from balanced chromosomal variations, that were considered to be normal chromosomally. Minor structural anomalies that were not under consideration in present study were hip instability & luxation, hemangioma and non-neoplastic nevus, hydronephrosis (<5 mm), inguinal hernia, preauricular appendage, persistent ductus arteriosus, polydactyly, persistent foramenovale (with spontaneous regression), retention testis, and syndactyly.
An anomaly was deemed to have been identified by ultrasound during pregnancy, when the anomaly was initially suspected when the ultrasound diagnosis was in sensible agreement with that of definitive diagnosis, regardless of the possibility that the last analysis was not made until some other time. A chromosomal anomaly was deemed to be diagnosed only post performance of fluorescence in situ hybridization or fetal karyotyping and confirmation of abnormal chromosomes. The speculated anomalies were deemed to be false +ve if they couldn’t be affirmed post birth, pregnancy termination or miscarriage, even during anomaly regression cases like pleural effusion/hydronephrosis. The structural anomalies in fetuses/ babies with normal chromosomes were categorized as per organ systems and as major/minor with regards to clinical significance. The contrast of minor as well as major was done as a team, with pediatric doctor with direction from proposition by Royal College of Obstetrics and Gynecology in 1997 [15].
The specificity, sensitivity, prevalence, Positive (PPV) as well as Negative Predictive Values (NPV) and False Positive Rate (FPR) with respect to chromosomal and structural anomalies were computed. The computations were conducted per baby, not as per anomaly. Prevalence was described as the no. of fetuses/babies with affirmed diagnosis of anomalies divide by aggregate number. The sensitivity was described as the no. of fetal anomalies identified prior to delivery and affirmed post birth divide by aggregate number of affirmed irregular fetuses. To measure the sensitivity for identification of fetal anomalies using standard ultrasound exam, we utilized the no. of affirmed anomalies identified prior to 22 gestation weeks, except for anomalies identified by 1st trimester ultrasound exam, divide by aggregate of affirmed irregular fetuses. A FPR was characterized as no. of fetuses getting prenatal anomaly diagnosis that couldn’t be affirmed post birth divide by aggregate of fetuses getting prenatal anomaly diagnosis. Statistical analysis was conducted using Microsoft Excel Professional Plus 2010.
Results
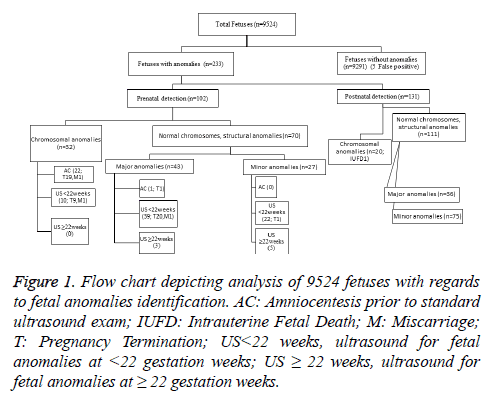
Amid the reporting period, 9466 babies were delivered at our hospital, and 16 babies were delivered at different hospitals in light of anomaly detection amid pregnancy through ultrasound test conducted in our hospital. Additionally, incorporated into the review were 39 fetuses having anomalies diagnosed at our hospital even though these pregnancies were ended later. Two babies were miscarried yet were determined to have expanded nuchal translucency thickness prior to miscarriage. Those two fetuses got anomaly diagnosis post-mortem. Furthermore, one fetus likewise incorporated into the review had an ordinary standard ultrasound examine yet died in utero and was determined to have a chromosomal anomaly post-mortem. An aggregate of 9524 fetuses composed of study population. The Figure 1 depicts the analysis of 9524 fetuses with regards to fetal anomalies identification. The mean age of the pregnant women was 31.5 years (range: 16 to 51 years).
Figure 1: Flow chart depicting analysis of 9524 fetuses with regards to fetal anomalies identification. AC: Amniocentesis prior to standard ultrasound exam; IUFD: Intrauterine Fetal Death; M: Miscarriage; T: Pregnancy Termination; US<22 weeks, ultrasound for fetal anomalies at <22 gestation weeks; US ≥ 22 weeks, ultrasound for fetal anomalies at ≥ 22 gestation weeks.
There were 233 fetuses/babies having affirmed anomalies, prevalence 2.45% (233/9524). Out of those fetuses/babies, 22.31% (52/233) had chromosomal anomalies, prevalence 0.55% (52/9524), and 78% (181/233) had ordinary chromosomes along with structural anomalies, prevalence 1.9% (181/9524). The affirmed anomalies distinguished prenatally were 102, giving a total sensitivity for prenatal fetal anomaly detection of 43.78% (102/233; 95% confidence interval (CI) 37.31-49.98), specificity of 99.95%, PPV of 95.33%, and NPV of 98.61%. The immense greater part, 94 anomalies, were identified prior to 22 gestation weeks, giving an aggregate detection rate prior to 22 gestation weeks of 40.34% (94/233; 95% CI 33.99-46.95). Among the diagnoses, 23 anomalies (22 chromosomal anomalies and one major anomaly) were identified via amniocentesis basically or post the 1st trimester ultrasound screen for trisomies, prior to standard ultrasound exam in 2nd trimester. The rest 71 anomalies (10 chromosomal anomalies and 61 structural anomalies) were identified by standard ultrasound exam, giving sensitivity for prenatal anomaly detection by standard ultrasound exam alone of 30.47 % (71/233). Eight affirmed structural anomalies were identified prenatally yet post 22 gestation weeks.
Notwithstanding the 102 prenatal identified fetuses, other five fetuses got prenatal fetal anomaly diagnosis which couldn’t be affirmed post birth and were characterized as false positives, with FPR of 4.67% (5/107).
Out of prenatal anomalies, 68.63 % (70/102) were structural anomalies (normal chromosomes), and 31.37% (32/102) were chromosomal anomalies. In fetuses/babies with structural anomalies, 43.64% (79/181) were categorized as major with prevalence 0.83% (79/9524). The rest 56.35% (102/181) were categorized as minor with prevalence 1.1% (102/9524). In the study, the pre-natal identification rate for major structural anomalies was nearly double compared to minor, at 54.4% and 26.5%, respectively. The chromosomal and structural anomaly detection rates in 233 abnormal fetuses/babies were demonstrated in Table 1. Based on organ systems, prenatal detection rates diversified significantly. The greater detection rates were acquired for pulmonary (83.3 %) and central nervous systems (80%) followed by chromosomal anomalies (61.5%), urinary tract (52.8%), gastrointestinal (38.9%), others (38.1%), skeletal (32.3%), and cardiac systems (9.5%), respectively. Structural anomaly detection rate as per organ system are depicted in Table 2. In this study, atria septum defect (n=8), ventricle septum defect (n=18) as well as hypospadias (n=23) record for a greater part of minor structural anomalies that weren’t identified prenatal. For additional data in regards to categorization as well as anomaly detection rates per each category see Supplementary material (Table S1).
| Anomalies | Total (N) | Prenatal (<22 weeks) | Total prenatal | Postnatal | ||
|---|---|---|---|---|---|---|
| n | % | n | n | % | ||
| Chromosomal | 52 | 32 | 61.5 | 32 | 20 | 38.5 |
| Structural | ||||||
| Total | 181 | 63 | 34.8 | 70 | 111 | 61.3 |
| Major | 79 | 40 | 50.6 | 43 | 36 | 45.6 |
| Minor | 102 | 23 | 22.5 | 27 | 75 | 73.5 |
| Total | 233 | 98 | 42.1 | 102 | 131 | 56.2 |
Table 1. Chromosomal and structural anomaly detection rate in 233 abnormal fetuses/babies.
| Organ system | AC (%) | Detection at <22 weeks (%) | Detection at ≥ 22 weeks (%) | Detection at birth (%) | Prenatal detection rate (%) |
|---|---|---|---|---|---|
| Cardiac | 0 | 7.1 | 2.4 | 90.5 | 9.5 |
| Central Nervous | 0 | 80 | 0 | 20 | 80 |
| Gastrointestinal | 0 | 38.9 | 0 | 61.1 | 38.9 |
| Pulmonary | 0 | 50 | 33.3 | 16.7 | 83.3 |
| Skeletal | 0 | 32.3 | 0 | 67.7 | 32.3 |
| Urinary | 0 | 45.3 | 7.6 | 47.2 | 52.8 |
| Other structural anomalies | 4.8 | 28.6 | 4.8 | 61.9 | 38.1 |
Table 2. Structural anomaly detection rate as per organ system.
Overall, 49.02% (50/102) of prenatal detected anomalies caused in pregnancy termination. In fetuses having chromosomal anomalies that identified prenatally, there were 87.5% (28/32) of pregnancy terminations; with extra two fetuses lost via miscarriage, and one death in utero. In case of structural anomalies in normal chromosome fetuses, 31.43% (22/70) of pregnancies were ended, with extra one fetus lost via miscarriage.
Discussion
Our study demonstrated fetal anomaly identification rate of 40.34%, when recognized prior to 22 gestation weeks, and an extra 3.44%, when distinguished between 22 weeks and birth. Huge contrasts in study centers with following huge contrasts in pre-natal detection rates of 17% to 85% ranges [6,16], at times make general detection rate comparisons between studies hard. Elements like operational skills, gestational age, aggregate of standard exams rendered, specialized equipment utilized, the post-natal follow-up, and the choice and interpretation of anomalies incorporated, all crucially affect the prevalence as well as pre-natal detection rates.
The strength of present study is nonselected pregnant women population from an all-around characterized region where around 95% of pregnant women residents of area eventually give birth at our hospital. Our hospital is the main centre in the region with ultrasound setup as well as delivery department, allowing close follow-up of all babies. This quality is upheld by the predominance of congenital anomalies in present study. Certain inherent limitations need to be considered during interpretation of the results, as the study being a retrospective one.
In the study, the pre-natal identification rate for major structural anomalies was nearly double compared to minor, at 54.4% and 26.5%, respectively. The immense greater part of major structural anomalies, were identified prenatal at standard ultrasound exam. Detecting a major structural anomaly is of higher clinical interest in offering parents, a chance to choose whether to proceed with the pregnancy and to plan for the best baby care. Two studies by Saltvedt et al. and Rydberg et al. with comparable review settings and characterization of major anomalies, published major anomaly detection rates of 47% and 55%, respectively [17,18].
The rationale for distinction of detection rates for major as well as minor structural anomalies is that great predominance of minor anomalies of low clinical significance can considerably influence overall identification rate. In this study, atria septum defect (n=8), ventricle septum defect (n=18) as well as hypospadias (n=23) record for a greater part of minor structural anomalies that weren’t identified prenatal. To distinguish prenally an open foramen-ovale in a normal fetus from genuine pathological atria septum defect or detection of ventricle septum defect is exceptionally troublesome, and hypospadias are probably not going to be distinguished on the grounds that sex was not routinely inspected in singleton pregnancies in present study. A few reviews do exclude one or a few of these anomalies, which might give a greater pre-natal detection rates [3,5-7,10]. In different reviews, the quantities of these abnormalities are not pronounced, or it is impractical to figure out if they are incorporated [13,19]. The revealed prevalence of these anomalies was likewise significantly higher in present study than in numerous different reviews [6,9,10,12,20]. With those anomalies excluded, the aggregate sensitivity for prenatal identification of fetal anomalies raises from 43.64 to 56.35% in present study.
As per many reviews, we exhibited great identification rates for structural anomalies in pulmonary as well as central nervous systems [3,5,6,8-10,12,13,18,20], with lower rates in cardiac system [3,6,10,12,13,18]. The identification rates in pulmonary system are regularly influenced by the low quantities of anomalies in this system. The lower identification rate for cardiac anomalies in present study could partially be clarified by the way that chromosomal anomalies were viewed as better than structural anomalies. Numerous fetuses with chromosomal anomalies had cardiac anomalies, yet were just enrolled as per chromosomal anomaly. The approach where fetuses with irregular chromosomes are enlisted or included at all contrasts among studies. Huge contrasts in pre-natal identification rates could likewise be seen inside a similar organ framework. In case of gastrointestinal system, the prenatal identification rate for anomalies effecting abdominal wall was 100 % (7/7), however just 9.1 % (1/11) for fetus having any kind of atresia.
Fetuses/babies having chromosomal anomalies had greater odds of pre-natal identification than normal chromosome fetuses/babies with structural anomalies, at 61.5 % and 38.7 %, respectively. The larger part of chromosomal anomalies, that were discovered prenatally were analysed prior to the standard ultrasound exam via amniocentesis in high risk pregnant women. Three studies with comparable settings additionally indicated greater pre-natal identification rates for chromosomal anomalies than structural anomalies in normal chromosome fetuses [8,13,18]. Romosan et al. [6] and Rydberg et al. [18] demonstrate practically indistinguishable aggregate pre-natal identification rates of 62% and 61% for chromosomal anomalies and 40% and 39% for structural anomalies in normal chromosome fetuses at a tertiary center, respectively. Eminently, in their review, all pregnant women were provided on routine basis 2 ultrasound tests in 2nd and 3rd trimesters. Fadda et al. study [9] likewise reported pre-natal identification rate of 61% for chromosomal anomalies, however in this review, all pregnant women were provided 3 ultrasound tests amid pregnancy. A study by Nakling et al. from hospital [12] showed a pre-natal identification rate for chromosomal anomalies 26% least, however this review depends on information gathered near 1989 and 1999, and both the specialized equipment utilized and the conceivable outcomes of early fetus diagnosis for identification of chromosomal anomalies vary from those in this review.
Conclusion
In a routine clinical setting at a hospital, half of major structural abnormalities in fetuses with normal chromosomes are identified by standard ultrasound exam. Advancement in identification of cardiac anomalies is required. Chromosomal anomalies have the greatest probability for prenatal detection than structural anomalies in normal chromosome fetuses. Now a days, the greater part of chromosomal anomalies identified prenatally are diagnosed by amniocentesis prior to standard ultrasound exam in 2nd trimester in high risk women.
References
- Crane JP, LeFevre ML, Winborn RC, Evans JK, Ewigman BG, Bain RP. A randomized trial of prenatal ultrasonographic screening: impact on the detection, management, and outcome of anomalous fetuses. The RADIUS Study Group. Am J Obstet Gynecol 1994; 171: 392-399.
- Levi S. Mass screening for fetal malformations: the Eurofetus study. Ultrasound Obstet Gynecol 2003; 22: 555-558.
- Eurenius K, Axelsson O, Cnattingius S, Eriksson L, Norsted T. Second trimester ultrasound screening performed by midwives; sensitivity for detection of fetal anomalies. Acta Obstet Gynecol Scand 1999; 78: 98-104.
- Levi S. Routine ultrasound screening of congenital anomalies. An overview of the European experience. Ann N Y Acad Sci 1998; 847: 86-98.
- Chitty LS, Hunt GH, Moore J, Lobb MO. Effectiveness of routine ultrasonography in detecting fetal structural abnormalities in a low risk population. BMJ 1991; 303: 1165-1169.
- Luck CA. Value of routine ultrasound scanning at 19 weeks: a four year study of 8849 deliveries. BMJ 1992; 304: 1474-1478.
- Taipale P, Ammala M, Salonen R, Hiilesmaa V. Two-stage ultrasonography in screening for fetal anomalies at 13-14 and 18-22 weeks of gestation. Acta Obstet Gynecol Scand 2004; 83: 1141-1146.
- Romosan G, Henriksson E, Rylander A, Valentin L. Diagnostic performance of routine ultrasound screening for fetal abnormalities in an unselected Swedish population in 2000–2005. Ultrasound Obstet Gynecol 2009; 34: 526-533.
- Fadda GM, Capobianco G, Balata A, Litta P, Ambrosini G, Dantona D. Routine second trimester ultrasound screening for prenatal detection of fetal malformations in Sassari University Hospital, Italy: 23 years of experience in 42,256 pregnancies. Eur J Obstet Gynecol Reprod Biol 2009; 144: 110-114.
- Stefos T, Plachouras N, Sotiriadis A, Papadimitriou D, Almoussa N. Routine obstetrical ultrasound at 18-22 weeks: our experience on 7,236 fetuses. J Matern Fetal Med 1999; 8: 64-69.
- Saari-Kemppainen A, Karjalainen O, Yleostalo P, Heinonen OP. Ultrasound screening and perinatal mortality: controlled trail of systematic one-stage screening in pregnancy. Lancet 1990; 336: 387-391.
- Nakling J, Backe B. Routine ultrasound screening and detection of congenital anomalies outside a university setting. Acta Obstet Gynecol Scand 2005; 84: 1042-1048.
- Hildebrand E, Selbing A, Blomberg M. Comparison of first and second trimester ultrasound screening for fetal anomalies in the southeast region of Sweden. Acta Obstet Gynecol Scand 2010; 89: 1412-1419.
- Persson PH, Weldner BM. Reliability of ultrasound fetometry in estimating gestational age in the second trimester. Acta Obstet Gynecol Scand 1986; 65: 481-483.
- Royal College of Obstetricians and Gynaecologists. Ultrasound Screening for Fetal Abnormalities: Report of the RCOG working party. London: RCOG 1997.
- Ewigman BG, Crane JP, Frigoletto FD, Lefevre ML, Bain RP. Effect of prenatal ultrasound screening on perinatal outcome. RADIUS Study Group. N Engl J Med 1993; 329: 821-827.
- Saltvedt S, Almstreom H, Kublickas M, Valentin L, Grunewald C. Detection of malformations in chromosomally normal fetuses by routine ultrasound at 12 or 18 weeks of gestation-a randomised controlled trail in 39572 pregnancies. BJOG 2006; 113: 664-674.
- Rydberg C, Tunon K. Detection of fetal abnormalities by second trimester ultrasound screening in a nonselected population. Acta Obstet Gynecol Scand 2016.
- Boyd PA, Chamberlain P, Hicks NR. 6-year experience of prenatal diagnosis in an unselected population in Oxford, UK. Lancet 1998; 352: 1577-1581.
- Chen M, Leung TY, Sahota DS, Fung TY, Chan LW, Law LW. Ultrasound screening for fetal structural abnormalities performed by trained midwives in the second trimester in a low-risk population-an appraisal. Acta Obstet Gynecol Scand 2009; 88: 713-719.