Case Report - Journal of Trauma and Critical Care (2017) Volume 1, Issue 1
Extravasation: there could be more than meets the eye!
Fatimah Lateef1,2*1Department of Emergency Medicine, Singapore General Hospital, Singapore
2Dukes-NUS Graduate Medical School and Yong Loo Lin School of Medicine, National University of Singapore, Singapore
- *Corresponding Author:
- Fatimah Lateef
Department of Emergency Medicine
Singapore General Hospital
Singapore
Tel: 65 63214972/3558
Fax: 65 63214873
E-mail: fatimah.abd.lateef@singhealth.com.sg
Accepted Date: February 15, 2017
Citation: Lateef F. Extravasation: there could be more than meets the eye! J Trauma Crit Care. 2017;1:1-4
Abstract
Intravenous catheter insertion is one of the commonest procedures in hospitals. It may sound like a simple intervention, but it is certainly critical in resuscitation and the administration of infusion and medications. However, the insertion of peripheral venous catheters or intravenous plugs can be associated with complications such as pain, bleeding, thrombophlebitis, failure of proper cannulation thus leading to extravasation and infection.
The incidence of extravasation is increased in the population prone to complications, e.g. extremes of age groups, intravenous drug users, diabetics. In published reports, the mechanism of damage is postulated to be due to factors such as direct cellular toxicity, vasoconstriction leading to ischaemia, osmotic damage or even extrinsic mechanical compression of large volumes of extravasation. The morbidity can be reduced with early detection and vigilance. Of course, prevention is better than cure.
Keywords
Extravasation, Infiltration, Intravenous, Ischaemia, Escharotomy.
Introduction
Intravenous catheter insertion is one of the commonest procedures in hospitals. It may sound like a simple intervention, but it is certainly critical in resuscitation and the administration of infusion and medications. However, the insertion of peripheral venous catheters or intravenous plugs can be associated with complications such as pain, bleeding, thrombophlebitis, failure of proper cannulation thus leading to extravasation and infection [1].
This is a case report of a patient with an emergency situation and difficult intravenous access, which led to extravasation causing pressure symptoms, which required escharotomy. We also discuss briefly the etiology, pathogenesis and management.
Case Report
Madam Y presented to the Department of Emergency medicine with symptoms of fluid overload and cardiogenic shock. She has a long history of diabetes mellitus, hypertension, coronary artery heart disease as well as end stage renal failure on haemodialysis. On arrival, she was tachypnoeic, with her oxygen saturation being at 88% on pulse oximetry and her first blood pressure reading was 90/58 mmHg. She was managed in the resuscitation room and one of the first things was to set an intravenous (IV) line and collect her blood tests. As her arterio-venous (AV) fistula for haemodialysis was on her right arm, the intravenous access attempts were made on her left hand and arm.
The IV access was challenging and multiple attempts were made over the dorsum of her left hand and then, higher up the arm as well. Two of these attempts were successful, but the veins were noted to be small and fragile. The infusions were not sustainable as after some minutes the extravasation was noted, and the IV plugs were removed appropriately. In both cases, medication such as morphine, and infusion of nitroglycerine and dopamine were commenced. After some 15 to 20 min, these infusions had to be stopped when the extravasation was noted.
As there was quite a significant extravasation, her distal neurovascular status was monitored and after the removal of the last IV plug and infusion, it was found that her radial pulse was weak and the left hand slightly dusky.
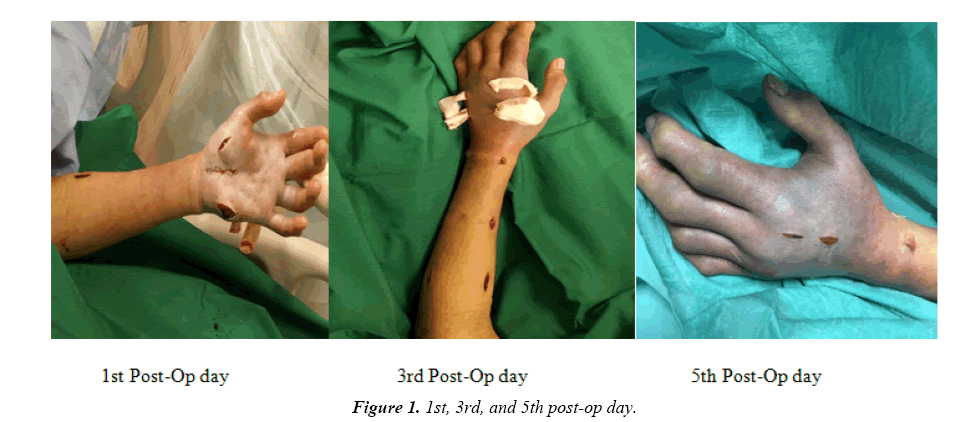
The plastic surgeon was activated to review the patient. Despite non-invasive intervention, with close monitoring of the neurovascular status, she did not improve and had to have escharotomy to her swollen arm (Figure 1).
The circulation improved and the swelling subsided gradually and she was discharged on the sixth post-operative day.
Discussion
Extravasation (Ex) is the inadvertent leakage of fluid or solution from its intended vascular pathway into the surrounding tissue plane and spaces. In the most serious of cases, the injury can extend to affect tendons, nerves and joints and may even continue for weeks. There are reports of the most serious cases needing skin grafting and even, amputation [1,2].
Infiltration, on the other hand, refers to the same process, usually involving a non-vesicant solution (not likely to cause blisters, tissue injury or necrosis) and is increasingly seen as benign, as compared to Ex. It often does not cause significant tissue injury or necrosis, except on the rare occasion when a very large volume of infiltrate causes physical compression of structures such as nerves and vessels as in a compartment syndrome [1-4].
Etiology
The common sites implicated for Ex injuries include the dorsum of the hands, wrists, feet and ankles. The ante-cubital fossae and areas near joints are also very prone. These are often sites with very minimal soft tissue for the protection of the underlying structures [5,6].
Not all infiltration and Ex injuries are due to faulty technique of cannulation by healthcare staff. There are certain groups of people who are at higher risk of getting an Ex injury. Limbs with vascular problems and edema which have reduced blood flow and stasis are more prone. Peripheral veins are also more likely to be involved. Patients with fragile and challenging venous access such as those on regular chemotherapy, with renal failure and diabetic patients are also more prone to Ex events, as are patients who have had radical mastectomy, axillary surgery and lymph node dissection. For intravenous (IV) drug abusers, as their peripheral veins are often thrombosed and getting a good venous access can be challenging. This puts them at risk. For diabetic patients with peripheral neuropathy, they may not feel the pain of Ex till very late and this makes their limbs more vulnerable. The other factors which put a person at higher risk for Ex are, being on anticogulation and antiplatelet drugs, vasodilator and hormonal therapy which causes vasodilation, prolonged intravenous antibiotics therapy and Raynaud’s phenomenon [6-8]. Extremely young children, uncooperative and agitated patients are also at risk, just as are those who have prolonged hospitalization and need repeated cannulation.
The risk of Ex is also higher when a large gauge cannula is utilized relative to the size of the vein, when the cannula is not adequately secured after insertion or when the placement is at a less desirable site (e.g. over the wrist, joints and ante-cubital fossae where a lot of movements such as flexion and extension occurs). Therefore, instructions and supervision of patients on IV is also important. The skills and capabilities as well as experience of the personnel also play a part. It is important for staff to pay attention to the slightest symptoms from patients related to their cannulae as this could mean the first indication of something being amiss. Symptoms such as discomfort, pain, swelling, bleeding, induration or discolouration must be reviewed. Recognition and a high index of suspicion is also needed when checking and monitoring these patients with limb observations such as colour, swelling, capillary return and pain score.
Pathogenesis
Many factors have been postulated and put forth to explain the tissue damage that follows extravasation. Many of these are related to the physico-chemical nature of the drugs or solutions that leaked.
Some of the factors are: [2,7,8]
1. Ability to bind to DNA directly, causing cellular toxicity.
2. Ability to kill replicating cells that it comes in contact with.
3. Ability to cause vascular dilation.
4. pH not within the range of 5.5 to 8.5.
5. Solutions or infusate with osmolarity >290 mosmol/L.
Thus, factors like volume, concentration, osmolarity and dissociability of the drug or solution are important considerations for healthcare personnel and pharmacy staff assisting in certain preparations for patients. A vesicant solution, when extravasated, is more likely to cause blisters, soft tissue injury and necrosis, in such cases, both the concentration and volume are important considerations. Some examples of common drug infusions with vesicant effects are vancomycin, amphotericin, phenytoin, gentamicin and cefotaxime [7-9].
Other groups of drugs where caution is needed when in use and especially when used for longer term are [2,3,5]:
Vasocompressive drugs: dopamine, dobutamine, epinephrine.
Concentrated electrolyte solutions: calcium chloride, calcium gluconate 10%, potassium chloride 7.45% and 10% sodium chloride.
Cytoxic agents: doxorubicin, mitomycin, Actnomycin-D, vincristine, vinblastine.
Hyperosmolar Solution: >10% dextrose, 15% mannitol.
Others: radiographic contrast solution.
Management
As in most incidents, prevention is better than cure. Initial and early pick up or recognition is critical. It is also important to have staff be able to distinguish extravasation from other local reactions. Familiarity, experience and a high index of suspicion is important. The local reactions that can mimick Ex include: [2,9-11].
− Flare reaction: which usually is itchy, has blotches or hives and not associated with pain.
− Vessel irritation: This presents with tightness over the skin.
− Vessel shock: whereby the muscular wall of the vessel goes into spasm, usually from cold drugs or too rapid administration.
− Hypersensitivity: This usually is like an allergic reaction with hives or urticarial lesions.
There can also be differences in time of onset, extent and the degree of swelling between these reactions and Ex.
The immediate course of action with the suspicion or diagnosis is to stop the infusion or administration, press over the site to express exudate and mark out the area affected by the Ex. The time of injury with the drug/infusate, its concentration and the amount that has been delivered, should be recorded. The importance of clear documentation cannot be over-emphasized. Pain relief or analgesia can be given as required. The hand or limb affected should be kept elevated with close monitoring, especially of the neurovascular status, area affected and demarcated, degree of swelling as well as symptoms such as pain or numbness. Antibiotic can be used in selected patients and the referral for surgical intervention is also to be considered on a case by case basis, in particular if there is worsening pain and swelling, ulceration and necrosis. With early surgical intervention, such as in the case of our patient, Madam Y, the extravasated drug is cleared by subcutaneous area washing and flushing with saline (“flush-out”). Some may add local anaesthetic to the saline used for this purpose. Much of the management is done by nursing staff and this is one of the competencies for nurses to master [9-13].
In some Ex, local application of antidotes can be utilized. This may be for example, the use of sodium thiosulphate for mechlorethamine, hyaluronidase for vinca alkaloids Ex and dimethylsulfoxide (DMSO), which can help prevent and reduce tissue necrosis. DMSO also reduces inflammation, relief pain and help in scavenging free radicals in the area. If utilized, it should be started within 10-20 minutes from the time the diagnosis is made. Procedures such as liposuction and saline flush have been reported but does not have widespread, nor evidence based application. For vesicant solution Ex, once the infusion is halted and aspiration of as much a possible of the extravasated drug through the intact catheter has been carried out, cold packs applications may be helpful for symptom relief. This however, should not be used in vinca alkaloids Ex, as the vasoconstriction can worsen the injury [3,10,12-15].
The bottom line with managing Ex is high vigilance and alertness, especially with high risk patients receiving high risk drugs and infusions. Many departments and institutions already have their standard operational steps to handle these. It is necessary to have these action algorithms, made familiar to the staff and to have them be as user-friendly as well, so that these Ex can be handled appropriately. This way staff will find them less cumbersome and readily apply them at work as relevant. Handing over patients with IV lines at every shift should also become standard practice and in some institutions, they have incorporated an IV line round to review and assess all the lines, infusions and medication in progress. In some institutions the use of care managers is utilized. They are trained personnel and one of their job descriptors is to assist in execution and communication of the care rendered by the doctors, nurses and healthcare team to the patients and their families. The care managers can interphase between members of the healthcare team and help to strengthen the partnership between patients, their families and the healthcare teams. Assessing and observing IV lines can be one responsibility that is important. They can also help in patients with IV medications, transitioning between the hospitals and primary health care as well as home care [16].
Conclusion
The reported incidence of Ex in general, ranges between 10- 30% and in cancer therapy, it accounts for up to 6% of all adverse events [17,18]. In every department and institution where catheters are being inserted as a procedure regularly, it is necessary to have an adequate and comprehensive protocol as well as training for the staff. This must include detection, monitoring and also management steps. Some departments have prepared “Extravasation kits” equipped with the necessary instructions, paperwork documentation and even some of the commonly used antidotes solution. Up to date theoretical knowledge and systematic stepwise interventions can help provide the safety needs for our patients and avoid the development of Ex and reduce the severe complications, if it does happen.
References
- Garden AL, Laussen PC. An unending supply of unusual complications from central venous catheters. Paeds Anaesthesia. 2004;14:905-9.
- Al-Benna S, O’Boyle C, Holley J. Extravasation injuries in adults. ISRN Dermatol. 2013.
- Kassner E. Evaluation and treatment of chemotherapy extravasation injuries. J Paeds Oncology Nurs. 2000;17:135-48.
- Sauerland C, Engelking C, Wickhem R, et al. Vesicant extravasation. Part 1. Mechanism, pathogenesis and nursing care to reduce risk. Oncol Nurs Forum. 2006;33:134-41.
- Jones LP. Extravasation. Oncol Nursing. 2004;8:355-8.
- Hadaway LC, Millam DA. On the road to successful IV starts. Nursing. 2005;35:1-14.
- Coyle C, Griffie J, Czaplewski L. Eliminating extravasation events: A multidisciplinary approach. Infusion Nurses Society. 2014;37:157-64.
- Gault DT. Extravasation injuries. Br J Plastic Surg. 1993;46:91-6.
- Hadaway L. Preventing and managing peripheral extravasation. Am J Nurs. 2007;107:64-72.
- Schulmeister L. Vesicant chemotherapy extravasation management. British J Nurs. 2011;20:6-12.
- Wengstrom Y, Margulies A. European Oncology Nursing Society extravasation guidelines. Eur J Oncol Nurs. 2008;12:357-61.
- Bertelli G, Forno GB. Hyaluronidase as an antidote to extravasation of vinca alkaloids: Clinical results. J Cancer Res Clin Oncol. 1994;120:505-6.
- Firat C, Erbatur S, Aytekun AH. Management of extravasation injuries: a retrospective study. J Plastic Surg Hand Surg. 2013;47:60-5.
- Thakur JS, Chauhan CG, Diwanna VK, et al. Extravasational side effects of cytoxic drugs: A preventable catastrophe. Ind J Plastic Surg. 2008;41:145-50.
- Piko B, Laczo C, Szatmari K, et al. Overview of extravasation management and possibilities for risk reduction based on literature data. J Nurs Educ Pract. 2013;3:93-105.
- Ciccone MM, Aquilino A, Cortese F. Project Lepnardo to improve health outcomes and promote better care utilization. Vasc Health Risk Manag. 2010;6: 297-305.
- Rose REC, Felix R, Crawford-Sykes A, et al. Extravasation injuries. West Indian Med J. 2008;57:40-7.
- Groutos I, Cogwell LK, Giele H. Extravasation injuries: A review. Eur J Hand Surg. 2014;39:808-18.