Research Article - Biomedical Research (2017) Volume 28, Issue 22
Expressions of PS-2, CA153 and VEGF and clinical significance in patients with breast cancer
Li Zhixiang, Qian Jun*, Li Jing, Zhu Chao
Department of Tumor Surgery, The 1st Affiliated Hospital of Bengbu Medical College, China
- *Corresponding Author:
- Qian Jun
Department of Tumor Surgery
The 1st Affiliated Hospital of Bengbu Medical College, China
Accepted date: October 17, 2017
Abstract
Objective: To observe the expression of Presenilin 2 (PS-2), CA153, and Vascular Endothelial Growth Factor (VEGF) of the patients with breast cancer and discuss the clinical implication.
Methods: The expression of PS-2 and VEGF were measured by immunohistochemistry; and the serum level of CA153 was measured by enzyme linked immune sorbent assay. Meanwhile, the associations between PS-2, CA153, VEGF and clinical pathologic features were evaluated.
Results: The positive expression rates of PS-2, CA153 and VEGF were 45.19%, 86.54%, 76.92% respectively. As a result of 0-4 level classification, the expressions of PS-2 and VEGF in the breast cancer tissues were statistically different with these in the normal tissue, p<0.05. There was positive correlation between the expressions of CA153 and VEGF in the breast cancer patients, which were higher than the expressions in the normal group, p<0.05. Besides, the expressions of CA153 and VEGF in the breast cancer patients with axillary lymph node metastasis were higher than the patients without metastasis, p=0.0027<0.05.
Conclusion: There are significant evidences that PS-2, CA153 and VEGF would be the independent risk factors, so as to be contributed to the predictions of the malignancy degree and metastasis of breast cancer.
Keywords
Presenilin 2, CA153, Vascular endothelial growth factor, Breast cancer, Metastasis
Introduction
Breast cancer is one of the higher-incidence malignant tumors among women. In recent years, more and more women especially young women have suffered from this disease, so, it more and more seriously endangered the women’s lives. Its pathogenesis hasn’t been clearly known [1], and curative effects and survival rate are not satisfactory. So, early diagnosis and treatment are especially important for improving the prognosis of breast cancer patients. Since this century, continuous in-depth study has been made on biological behaviors of breast cancer and its pathogenesis, thus, detection on some indexes about pathology and molecular biology has become an important method for breast cancer diagnosis and treatment selection and prognosis judgment [2]. In this study, we detected the estrogen-regulated protein (PS-2) and Vascular Endothelial Growth Factor (VEGF) by immunohistochemistry and CA153 change in serum of breast cancer tissue by Enzyme Linked Immunosorbent Assay (ELISA), and discussed the correlation of clinicopathological features of breast cancer patients.
Clinical Data and Methods
Clinical data of patients
Ethical approval was given by the medical ethics committee of the 1st Affiliated Hospital of Bengbu Medical College with the following reference number: 2010010. In this study, 104 patients diagnosed with breast cancer by pathology section in our hospital from January of 2011 to March of 2017 were included, with complete postoperative clinical data and wellpreserved breast cancer tissue paraffin specimens; the patients aged 25-76, with average age of 51.33 ± 13.24 and median age of 51. Additionally, 30 normal breast tissue specimens and blood specimens were selected as negative controls.
Inclusion criteria
(1) patients hospitalized in our hospital, with complete medical records; (2) all patients were attacked by primary breast cancer; (3) those who didn’t accept radiotherapy, chemotherapy and surgery before blood and tissue specimens were sampled; (4) those who had no diabetes, hypertension, coronary heart disease, kidney disease, liver disease, lung disease and other serious primary lesions; (5) those who had no history of other malignant tumors.
Sampling and index detection
Sample collection of cases: According to the pathological number, the paraffin embedded tissue sections stored in our pathology department were taken out, after deparaffinated and hydrated, then placed on the glass slide, baked for 48 h for later use.
Blood sampling: 5 ml of venous blood was drawn from fasting patient, centrifuged, and then the serum was stored in -78°C.
Immunohistochemical method (S-P)
PS-2 antibody and VEGF antibody were provided by Shanghai Tiyo Biotechnology Co, Ltd. The breast cancer specimens were used as negative controls, while normal breast tissue specimens were used as negative controls. Immunohistochemical method followed the experimental procedures indicated on the instructions of the kits.
CA153 kits were purchased from Shanghai Keshun Biological Technology Co., Ltd., the experimental procedures indicated on the instructions of the kits were followed.
Judgment of Results
The stained pathology sections were observed under 400- magnification microscope, then 10 fields were randomly selected to calculate the percentage of stained positive cells.
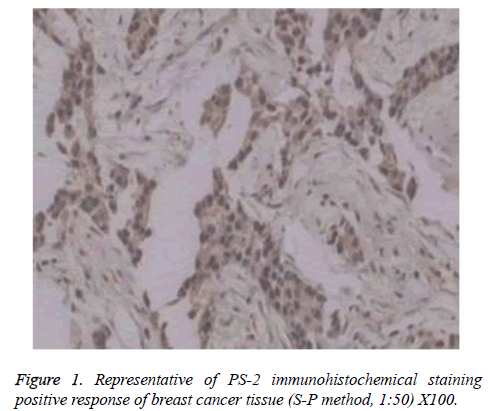
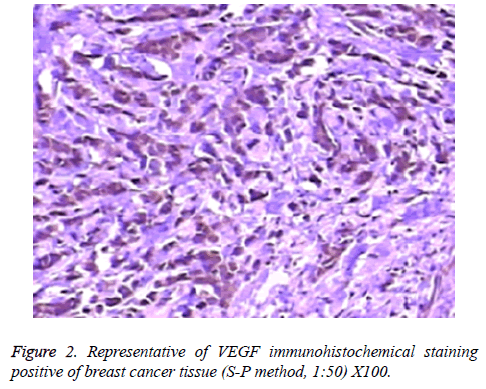
PS-2 and VEGF immunohistochemical positive results: cell nucleus or cytoplasm stained with brown indicated positive response; grade 0=negative, showed no cell staining; grade 1=5%-20%, showed tumor cell nuclear was dyed light brown; grade 2=20%-50%, showed tumor cell nuclear was dyed brown; grade 3=50%-75%, showed tumor cell nuclear was dyed brown; grade 4=above 75%, showed above tumor cell nucleus was dyed brown.
CA153 measured result reference was 0-35 μ/ml, >35 μ/ml indicates positive response.
Statistical processing
The data were processed by SPSS19.0 statistical software; differences were tested by chi-square test, comparison among measuring data were made with unpaired t-test; p<0.05 indicated the differences were of statistical significance.
Results
Analysis of positive results
As shown in immunohistochemical test results, among 104 patients, positive responses occurred in expression of PS-2 and VEGF for 47 (45.19%) and 80 (76.92%) patients respectively (Figures 1 and 2).
ELISA test results showed that, CA153 expression in 90 patients (86.54%) was positive, namely >35 U/ml, average value was (59.69 ± 31.86 U/ml).
Relationship of PS-2 expression in breast cancer tissue and clinicopathological features
PS-2 positive expression was localized in breast cancer cytoplasm and shaped in brown granules, a little expressed in nucleus, as shown in Figure 1. Less expressed in normal tissue, its staining strength was weaker than cancer tissue. Taking whether positive response occurred in PS-2 as the outcomes, the expression rates of PS-2 in normal breast tissue and breast cancer tissue were 23.33% and 45.19% respectively, the positive rate of breast cancer tissue was higher than that of normal breast tissue, but showing no statistical difference, p>0.05; correlation analysis showed no statistical difference (Table 1). PS-2 was dependent on grade 0-4 classification, so, expression of normal breast tissue and breast cancer tissue showed statistical difference, as shown in Table 2, which indicated that the higher the PS-2 expression, the higher the breast cancer incidence. PS-2 positive expression rate was not related to age, tumor size, axillary lymphatic metastasis and menstrual conditions (Table 3).
| Group | PS-2 | Total (cases) | |
|---|---|---|---|
| (+) | (-) | ||
| Normal breast tissue group | 7 (23.33) | 23 (76.67) | 30 |
| Breast cancer tissue group | 47 (45.19) | 57 (54.81) | 104 |
Table 1. Expression of PS-2 in breast tissue (n, %). Note: Spearman rank correlation analysis: r=0.1836, χ2=2.7932, p=0.1077.
| Group | PS-2 | Total (case) | |||
|---|---|---|---|---|---|
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | ||
| Normal breast tissue group | 23 (76.67) | 7 (23.33) | 0 | 0 | 30 |
| Breast cancer tissue group | 57 (54.81) | 14 (13.46) | 19 (18.27) | 14 (13.46) | 104 |
Table 2. Expression of PS-2 in breast tissue (n, %). Note: Fisher test: p<0.05
| Item | Number of patients (Cases) | PS-2 positive expression | χ2 | P |
|---|---|---|---|---|
| Age (y old) | ||||
| 21 | 8 (38.10) | 2.49 | 0.2656 | |
| 38 | 18 (47.37) | |||
| 45 | 21 (46.67) | |||
| Tumor diameter (cm) | ||||
| 58 | 23 (39.66) | 2.01 | 0.3774 | |
| 36 | 18 (50.0) | |||
| 10 | 6 (60.0) | |||
| Axillary lymphatic metastasis | ||||
| metastasis | 69 | 30 (43.48) | 0.40 | 0.6982 |
| No metastasis | 35 | 17 (48.57) | ||
| Menstrual conditions | ||||
| Premenopausal | 56 | 22 (39.29) | 0.23 | 0.4235 |
| Postmenopausal | 48 | 25 (52.08) |
Table 3. Relation of PS-2 expression and clinicopathological factors (n, %).
Relation of VEGF expression in breast cancer tissue and clinicopathological features
VEGF positive expression was localized in breast cancer cytoplasm and cell membrane and shaped in brown granules, and a little expressed in nucleus, as shown in Figure 2. Less expressed in normal breast tissues, its staining strength was weaker than cancer tissue. Taking whether positive response occurred in VEGF as the results, the expression rate of VEGF in normal breast tissue and breast cancer tissue was 40.0% and 76.92% respectively, the positive rate of breast cancer tissue was higher than that of normal breast tissue, showing statistical difference, p<0.05; correlation analysis showed statistical difference, p<0.05 (Table 4). VEGF was dependent on grades 0-4 classification, so, expression of normal breast tissue and breast cancer tissue showed statistical difference, p<0.05, as shown in Table 5, which indicated that the higher the VEGF expression, the higher the breast cancer incidence. VEGF positive expression rate was related to axillary lymphatic metastasis, but not related to age, tumor size and menstrual conditions (Table 6).
| Group | VEGF | Total (Cases) | |
|---|---|---|---|
| (+) | (-) | ||
| Normal breast tissue group | 12 (40.0) | 18 (60.0) | 30 |
| Breast cancer tissue group | 80 (76.92) | 24 (20.08) | 104 |
Table 4. Expression of VEGF in breast tissue (n, %). Note: Spearman rank correlation analysis: r=0.3082, χ2=7.4516, p=0.01319.
| Group | VEGF | Total (Cases) | |||
|---|---|---|---|---|---|
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | ||
| Normal breast tissue group | 18 (60.0) | 9 (30.0) | 3 (10.0) | 0 | 30 |
| Breast cancer tissue group | 24 (20.08) | 24 (23.08) | 37 (35.58) | 19 (18.27) | 104 |
Table 5. Expression of VEGF in breast tissue (n, %). Note: Fisher test: p<0.05.
| Item | Number of patients (Cases) | VEGF positive expression | χ2 | P |
|---|---|---|---|---|
| Age (y old) | ||||
| 21 | 14 (66.67) | 2.42 | 0.3157 | |
| 38 | 29 (76.32) | |||
| 45 | 37 (82.22) | |||
| Tumor diameter (cm) | ||||
| 58 | 42 (72.41) | 3.07 | 0.3546 | |
| 36 | 29 (80.56) | |||
| 10 | 9 (90.0) | |||
| Axillary lymphatic metastasis | ||||
| metastasis | 69 | 61 (88.41) | 7.22 | 0.0143 |
| No metastasis | 35 | 19 (54.29) | ||
| Menstrual conditions | ||||
| Premenopausal | 56 | 41 (73.21) | 1.96 | 0.5667 |
| Postmenopausal | 48 | 39 (81.25) |
Table 6. Relation of VEGF expression and clinicopathological factors (n, %).
Relation of CA153 in serum of breast cancer patients and clinicopathological features
The test results showed that CA153 in serum of breast cancer patients was apparently higher than that of normal healthy group, showing statistical differences, p<0.05, as shown in Table 7. In addition, the positive rate of CA153 in serum (>35 U/ml) was related to the existence of axillary lymphatic metastasis, but not related to age, tumor size and menstrual conditions (Table 8).
| Group | Number of patients (Cases) | CA153 (U/ml) |
|---|---|---|
| Normal control group | 30 | 12.37 ± 6.44 |
| Breast cancer group | 104 | 59.69 ± 31.86* |
Table 7. Expression of CA153 in breast tissue (U/ml). Note: *comparison with CA153 in normal breast tissue, p<0.05.
| Item | Number of patients (Cases) | CA153>35 U/ml | χ2 | P |
|---|---|---|---|---|
| Age (y old) | ||||
| 21 | 18 (85.71) | 1.59 | 0.4688 | |
| 38 | 34 (89.47) | |||
| 45 | 38 (84.44) | |||
| Tumor diameter (cm) | ||||
| 58 | 46 (79.31) | 2.96 | 0.1983 | |
| 36 | 34 (94.44) | |||
| 10 | 10 (100.0) | |||
| Axillary lymphatic metastasis | ||||
| metastasis | 69 | 69 (100.0) | 11.47 | 0.0052 |
| No metastasis | 35 | 21 (60.0) | ||
| Menstrual conditions | ||||
| Premenopausal | 56 | 50 (89.29) | 2.18 | 0.4132 |
| Postmenopausal | 48 | 40 (83.33) |
Table 8. Relation of CA153 expression and clinicopathological factors (n, %).
Relation among PS-2, CA153 and VEGF
Spearman correlation analysis on PS-2, CA153 and VEGF showed that PS-2 was not correlated to CA153 and VEGF, p>0.05; but CA153 was positively correlated to VEGF, p<0.05 (Table 9).
| PS-2 | CA153 | VEGF | |
|---|---|---|---|
| PS-2 | - | 0.3742 | 0.5541 |
| CA153 | 0.3742 | - | 0.0027* |
| VEGF | 0.5541 | 0.0027* | - |
Table 9. Relation among PS-2, CA153 and VEGF.
Discussion
Breast cancer is a kind of highly heterogeneous gynecologic malignancy. The serum and tissue biomarkers have been discovered and widely applied in breast cancer diagnosis and treatment [3], in recent years, its death rate in developing countries has declined year by year [4]; but, in the developing countries, study and medical level concerning tumor biomarkers are relatively weaker than the developed countries. So, breast cancer is still one of the malignant diseases endangering women’s lives in China [5].
Since discovered in 1982, the estrogen-regulated protein PS-2 has been a hot issue in gynecology field [6]. The occurrence and development of breast cancer is closely related to the estrogen, although biological function and action mechanism of PS-2 haven’t been clearly known [7], many overseas studies have verified that PS-2 is of certain specificity on breast cancer and closely related to tumor differentiation [8]. PS-2 gene is also called breast cancer estrogen-induced gene, with stable protein expression, and it can be detected by immunohistochemical method. This study has verified that among 104 breast cancer patients, PS-2 positive expression rate was 45.19%, higher than normal breast tissue, but there existed no statistical difference (p>0.05). Dependent on grades 0-4 classification, the expression of normal breast cancer tissue was statistically different from breast cancer tissue expression (p<0.05), suggesting that the higher the PS-2 expression, the higher the breast cancer incidence. PS-2 positive expression rate was not related to age, tumor size and axillary lymphatic metastasis. Number of specimens shall be increased and study time shall be prolonged to assess the relation between PS-2 and prognosis and survival of breast cancer patients.
VEGF is a kind of specific multi-functional factor acting on vascular endothelial cells [9], and its relation with tumor angiogenesis has been studied for many years. The anti-cancer drugs with VEGF and its receptor as target have been gradually applied in clinic [10]. This study showed that the expression of VEGF in normal breast tissue and breast cancer tissue was 40.0% and 76.92% respectively if using VEGF positive expression as outcomes, positive rate of breast cancer was higher than normal breast tissue (p<0.05). The expression of normal breast tissue was statistically different from that of breast cancer tissue (p<0.05) if using grades 0-4 classification as outcomes, suggesting that the higher the VEGF expression, the bigger the breast cancer incidence. VEGF positive expression rate is related to existence of axillary lymphatic metastasis, but not related to age, tumor size and menstrual conditions. Although VEGF is not a specific biomarker of breast cancer, it is closely related to tumor occurrence and development [11] and highly expressed in tumor tissue, while nearly not expressed or a little expressed in normal tissues; VEGF can act as one of reference indexes in assessing malignant degree of breast cancer, infiltration, metastasis and biological behaviors [12].
CA153 is a kind of antigen related to breast cancer [13,14], currently, it has been considered as a tumor marker of breast cancer and one of the effective indexes of breast cancer metastasis and prognosis [15-18]. In this study, ELISA test result showed that CA153 was positively expressed in 90 patients (86.54%), namely >35 U/ml, the average value was (59.69 ± 31.86 U/ml), so, the CA153 level was apparently higher than normal healthy populations in the control group (p<0.05). Additionally, the positive expression rate of CA153 in serum (>35 U/ml) was correlated to the axillary lymphatic metastasis, but not correlated to the age, tumor size and menstrual conditions. The correlation analysis showed that CA153 was positively correlated to VEGF, indicating the combined detection of CA153 and VEGF can enhance the specificity and accuracy of breast cancer diagnosis and has important significance to tumor metastasis and prognostic predication.
In conclusion, the expressions of PS-2, CA153 and VEGF in breast cancer tissue are respectively higher than those in normal breast tissues, and they are independent risk factors for breast cancer attack; especially, the positive expression rates of CA153 and VEGF are closely correlated to the axillary lymphatic metastasis of breast cancer, therefore, they can act as effective reference indexes for predicating tumor malignant degree, infiltration and metastasis.
References
- Kanbayashi C, Iwata H. Current approach and future perspective for ductal carcinoma in situ of the breast. Jpn J Clin Oncol 2017; 47: 671-677.
- Hq X, Jr H. Expression of Ki-67, EGFR, HER-2 and P53 protein in human breast cancer and their corrletion. Chinese Clin Oncol 2011; 16: 139-143.
- Sokolenko A, Imyanitov E. Multigene testing for breast cancer risk assessment: an illusion of added clinical value. Chin Clin Oncol 2017; 6: 15.
- Bogh SB, Falstie-Jensen AM, Hollnagel E. Predictors of the effectiveness of accreditation on hospital performance: A nationwide stepped-wedge study. Int J Qual Health Care 2017; 1-7.
- Tang S, Wei L, Sun Y.CA153 in breast secretions as a potential molecular marker for diagnosing breast cancer: a meta-analysis. PLoS One 2016; 11: 0163030.
- Jang EH, Jang SY, Cho IH. Hispolon inhibits the growth of estrogen receptor positive human breast cancer cells through modulation of estrogen receptor alpha. Biochem Biophys Res Commun 2015; 463: 917-922.
- Fabian CJ, Kimler BF, Zalles CM, Phillips TA, Metheny T. Clinical trial of acolbifene in premenopausal women at high risk for breast cancer. Cancer Prev Res (Phila) 2015; 8: 1146-1155.
- Lillo MA, Nichols C, Perry C. Methylparaben stimulates tumor initiating cells in ER+ breast cancer models. J Appl Toxicol 2017; 37: 417-425.
- Feng Q, Zhang C, Lum D. A class of extracellular vesicles from breast cancer cells activates VEGF receptors and tumour angiogenesis. Nat Commun 2017; 8: 14450.
- Jahanban-Esfahlan R, Seidi K, Monfaredan A.The herbal medicine Melissa officinalis extract effects on gene expression of p53, Bcl-2, Her2, VEGF-A and hTERT in human lung, breast and prostate cancer cell lines. Gene 2017; 613: 14-19.
- Luo M, Huang H, Hou L. Construction and expression of a lentivirus expression vector carrying the VEGF165-EGFP fusion gene in breast cancer MCF-7 cells. Oncol Lett 2017; 13: 1745-1752.
- XH Xia, WJ Yin, JC Gu. Clinical significance of coexpression of leptin and VEGF in breast cancer tissues. Chin J Cancer Prev Treat 2014; 21: 1807-1811.
- Wang Y, Li PZ, Huang LS. Significance of combining expression of serum HE4 and CA153 in predicting lymph node metastasis of early stage breast cancer. Mod Oncol 2017; 25: 390-392.
- Zhuang Z. The significance for expression of CA153 in nipple discharge and serum of the breast cancer. Chinese J Clin Oncol 2005.
- Huang F. The relationship between the expression of VEGF and CA153 and the progression of breast cancer. Int J Lab Med 2013; 34: 147-148.
- Zhu HY, Chen LQ, Pin XU. Study on the relationship between DCE-MRI findings and expression levels of VEGF and Her-2 in breast cancer. Chinese J CT MRI 2017.
- Payandeh M, Sadeghi M, Sadeghi E, Madani SH. Expression of p53 breast cancer in kurdish women in the west of iran: a reverse correlation with lymph node metastasis. Asian Pac J Cancer Prev 2016; 17: 1261-1264.
- XJ Zhou, JM Shen, ZZ Wan. Clinical significance of determination of changes on serum IGF-I, CA153, VEGF levels after chemotherapy in patients with breast cancer. Jilin Med 2015; 36: 2985-2987.