Research Article - Current Pediatric Research (2024) Volume 28, Issue 1
Evaluation of prescribing pattern of anti-epileptics in seizures for pediatrics at aster CMI hospital, Bengaluru-92.
Harisshri Kumar Vasani, M Lakshmi Gayathri*, Sharon Mariam Philip, Deepika Guntu, Kshiteej Dahal
1Department of Pharmacy, A Constituent unit of KAHER, Belagavi, Karnataka, India
- Corresponding Author:
- M Lakshmi Gayathri
Department of Pharmacy, A Constituent unit of KAHER, Belagavi, Karnataka, India
E-mail: gayathri.microbiologist14@gmail.com
Received: 25 December, 2023, Manuscript No. AAJCP-24-125456; Editor assigned: 27 December, 2023, Pre QC No. AAJCP-24-125456 (PQ); Reviewed: 10 January, 2024, QC No. AAJCP-24-125456; Revised: 17 January, 2024, Manuscript No. AAJCP-24-125456 (R); Published: 24 January, 2024, DOI:10.35841/0971-9032.28.01.1185-1189.
Abstract
Background: A seizure refers to a sudden change in neurological function caused by excessive, synchronized neuronal discharges in the brain. Epilepsy is characterized by recurrent, unprovoked seizures. Various factors can trigger seizures, such as electrolyte imbalances, toxic effects, withdrawal syndromes, medication irregularities, infections, fever, and sleep deprivation. Common types of seizures in children include absence epilepsy, juvenile myoclonic epilepsy, febrile seizures, and infantile spasms. Ensuring the appropriate and rational utilization of Anti-Epileptic Drugs (AEDs) is of utmost importance in the management of epilepsy.
Objectives: The objective of this study is to analyze the prescribing patterns of anti-epileptic medications for pediatric patients experiencing seizures, while also evaluating the effectiveness, compliance, and safety profile of these AEDs. Additionally, the study aims to determine the prevalent seizure types observed in the pediatric population.
Methods: The prospective study was carried out at Aster CMI hospital, Bengaluru, involving a total of 113 patients from the Neuro OPD, over a span of 6 months.
Results: Our findings revealed a higher prevalence of seizures among male patients (54.87%) compared to female patients (45.13%). Seizure occurrences were highest among children aged 0-5 years and lowest among those aged 15-18 years. The most observed type of epilepsy was idiopathic epilepsy, followed by febrile seizures. Levetiracetam emerged as the most frequently prescribed medication, with sodium valproate ranking second. Monotherapy was the predominant treatment strategy. Notably, only a single patient encountered an Adverse Drug Reaction (ADR) when administered levetiracetam.
Conclusion: Clinical pharmacists play a crucial role in evaluating prescribing patterns, which aids in comparing ongoing treatments with standard guidelines and promoting rational drug use while minimizing adverse drug reactions. Our study demonstrated that the prescribed medications were effective (97.35%) and safe (99.12%), with a patient compliance rate of 99.12%.
Keywords
Seizures, Levetiracetam, Paediatric, Juvenile myoclonic epilepsy, Idiopathic epilepsy.
Introduction
A seizure refers to a sudden and temporary disruption of neurological function caused by excessive and synchronized neuronal discharges in the brain epilepsy is a medical condition characterized by the occurrence of repetitive seizures, which can be either unprovoked or provoked, and can stem from various underlying dysfunctions in the brain. It is a prevalent neurological disorder, affecting approximately 50 new cases per 100,000 populations each year [1].
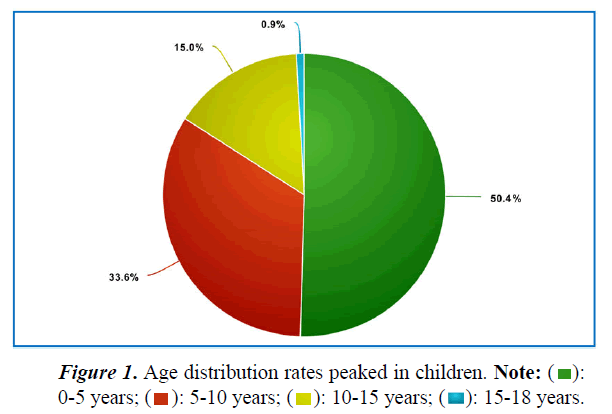
The International League Against Epilepsy (ILAE) categorized the etiology of epilepsy into three main groups in 1989: Idiopathic, Cryptogenic, and Symptomatic. Idiopathic epilepsies are believed to have a genetic origin, while cryptogenic epilepsies involve causes that remain unknown or undetermined. Symptomatic epilepsies, on the other hand, have an identifiable underlying cause (Table 1) (Figure 1) [2].
| Age group | No of patients |
|---|---|
| 0-5 years | 57 |
| 5-10 years | 38 |
| 10-15 years | 17 |
| 15-18 years | 1 |
Table 1. Age distribution rates peaked in children.
There are several common triggers for seizures, including electrolyte imbalances (such as hypoglycemia, hyponatremia, hypernatremia, and hypocalcemia), acute toxic effects of certain substances (like antidepressants and sympathomimetics), withdrawal syndromes (such as ethanol and benzodiazepines), irregularities with prescribed antiepileptic medications, sepsis, central nervous system infections, fever, sleep deprivation, traumatic brain injury, stroke (ischemic or hemorrhagic), hypoxic brain injury ,neoplasms, and inflammatory conditions such as anti- NMDA receptor encephalitis, lupus cerebritis etc. [3].
The ILAE guidelines classify seizures into three categories: generalized onset, focal onset, and unknown onset. Generalized seizures originate from distributed neuronal networks in both hemispheres and can be further categorized as absence seizures, generalized tonic-clonic seizures, myoclonic seizures, and atonic seizures. Focal seizures originate in a specific part of one cerebral hemisphere, while the origin of seizures with an unknown onset remains uncertain (Table 2) (Figure 2) [4].
| Gender | Male | Female |
|---|---|---|
| No. of patients | 62 | 51 |
Table 2. Gender distribution among male and female.
Common types of seizures observed in children include
• Absence seizures (previously known as petit mal) characterized by staring and unresponsiveness, sometimes accompanied by eye blinking or head nodding.
• Juvenile myoclonic seizures involve sudden, brief movements without obvious disturbance of consciousness, often occurring in the early morning after waking up from sleep.
• Seizure spasms manifest as sudden extension or flexion of extremities (such as the arm or leg) for several seconds, recurring in clusters. Epileptic spasms can occur anytime and any age, but when they begin usually for the first year of the child age, they are associated with a syndrome known as infantile spasms (West syndrome).
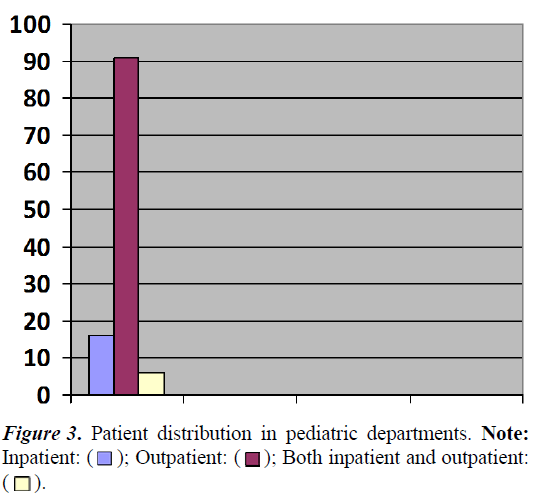
• SELECTS (Self-Limited Epilepsy with the Centrotemporal Spikes), also referred to as Rolandic epilepsy, which is a prevalent epilepsy syndrome among children, comprising approximately 15% of epilepsy cases in individuals below the age of 15. The seizures in SELECTS typically occur during sleep and often involve focal seizures with hypersalivation, altered sensory-motor function of the face, and unilateral arm or facial clonic movements (Table 3) (Figure 3).
| Departments | Inpatient | Outpatient | Both in and outpatient |
|---|---|---|---|
| No. of patients | 16 | 91 | 6 |
Table 3. Patient distribution in pediatric departments.
These medications can be prescribed as monotherapy or in combination with other anti-epileptic drugs in severe cases. Early initiation of antiepileptic medication is crucial for effective management of epilepsy [5].
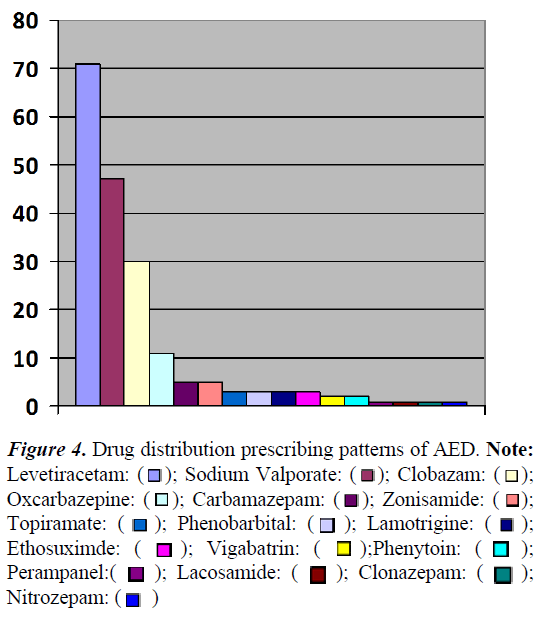
The study is needed to evaluate the appropriate use of antiepileptic drugs. Analyzing factors such as drug dosage, frequency of use, and dose management is essential for better clinical care and to ensure the rational use of AEDs. Evaluating the prescribing patterns of AEDs helps align treatments with established guidelines, identify areas for improvement, and promote evidence-based practices to enhance patient outcomes in epilepsy management (Table 4) (Figure 4) [6].
| Name of drugs | No. of patients |
|---|---|
| Levetiracetam (lev) | 71 |
| Sodium valproate (val) | 47 |
| Clobazam (clb) | 30 |
| Oxcarbazepine (oxz) | 11 |
| Carbamazepam (cbz) | 5 |
| Zonisamide (zns) | 5 |
| Topiramate (tpm) | 3 |
| Phenobarbital (phb) | 3 |
| Lamotrigine (lam) | 3 |
| Ethosuximde (esm) | 3 |
| Vigabatrin (vgb) | 2 |
| Phenytoin (pht) | 2 |
| Perampanel (pmp) | 1 |
| Lacosamide (lcs) | 1 |
| Clonazepam (clz) | 1 |
| Nitrozepam (ntz) | 1 |
Table 4. Drug distribution prescribing patterns of AED.
Figure 4: Drug distribution prescribing patterns of AED. Note: Levetiracetam: ( ); Sodium Valporate: (
); Sodium Valporate: ( ); Clobazam: (
); Clobazam: ( );
Oxcarbazepine: (
);
Oxcarbazepine: ( ); Carbamazepam: (
); Carbamazepam: ( ); Zonisamide: (
); Zonisamide: ( );
Topiramate: (
);
Topiramate: ( ); Phenobarbital: (
); Phenobarbital: ( ); Lamotrigine: (
); Lamotrigine: ( );
Ethosuximde: (
);
Ethosuximde: ( ); Vigabatrin: (
); Vigabatrin: ( );Phenytoin: (
);Phenytoin: ( );
Perampanel:(
);
Perampanel:( ); Lacosamide: (
); Lacosamide: ( ); Clonazepam: (
); Clonazepam: ( );
Nitrozepam: (
);
Nitrozepam: ( )
)
Materials and Methods
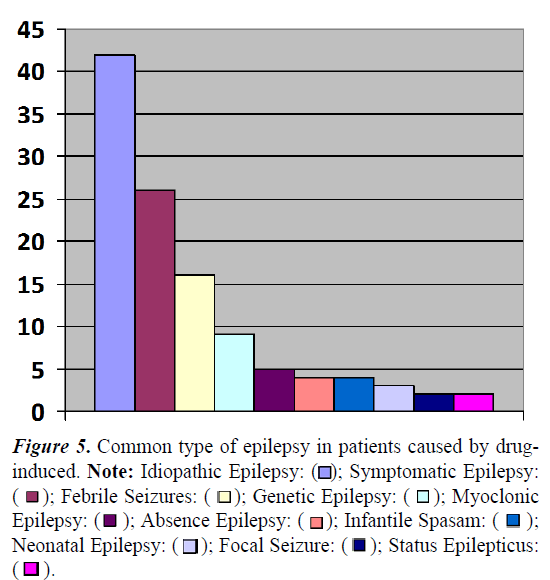
The prospective observational study was carried out in the paediatrics department of Aster CMI hospital, Bengaluru for duration of six months; the sample size was calculated for 113 patients. All in-patients and out-patients who were under 18 years of age with epileptic seizures, prescribed with antiseizure medications for long term management were included in the study and patients above 18 years of age. Individuals with any unrelated medical conditions. Patients with seizures caused by drug-induced, trauma-induced, or metabolic disorders. Patients with psychiatric conditions and subjects who decline to participate in the study were excluded (Table 5) (Figure 5) [7-10].
| Common type of epilepsy | No of patients |
|---|---|
| Idiopathic epilepsy | 42 |
| Symptomatic epilepsy | 26 |
| Febrile seizures | 16 |
| Genetic epilepsy | 9 |
| Myoclonic epilepsy | 5 |
| Absence epilepsy | 4 |
| Infantile spasam | 4 |
| Neonatal epilepsy | 3 |
| Focal seizure | 2 |
| Status epilepticus | 2 |
Table 5. Common type of epilepsy in patients caused by drug-induced.
Figure 5: Common type of epilepsy in patients caused by druginduced. Note: Idiopathic Epilepsy: ( ); Symptomatic Epilepsy:(
); Symptomatic Epilepsy:( ); Febrile Seizures: (
); Febrile Seizures: (  ); Genetic Epilepsy: (
); Genetic Epilepsy: ( ); Myoclonic Epilepsy: (
); Myoclonic Epilepsy: ( ); Absence Epilepsy: (
); Absence Epilepsy: ( ); Infantile Spasam: (
); Infantile Spasam: ( ); Neonatal Epilepsy: (
); Neonatal Epilepsy: ( ); Focal Seizure: (
); Focal Seizure: ( ); Status Epilepticus:(
); Status Epilepticus:( ).
).
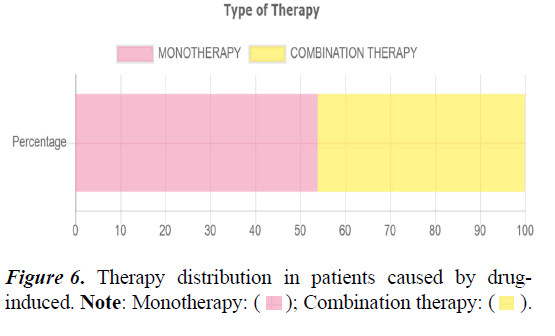
With approval from the Aster CMI hospital human ethical committee in Hebbal, Bengaluru. The eligible patients from the pediatric department were enrolled in the study based on predefined criteria. A comprehensive data collection form is completed, including the patient's demographic information, diagnosis, and details of their medication regimen. Each prescription is thoroughly reviewed and assessed. The appropriateness of the prescribed therapy is carefully analyzed, taking into consideration factors such as the patient's condition, recommended guidelines, and potential drug interactions or contraindications. The collected data is subjected to appropriate statistical analysis methods to derive meaningful insights and draw conclusions from the study (Table 6) (Figure 6) [11-13].
| Monotherapy | Combination therapy |
|---|---|
| 61 (53.9%) | 52 (46.1%) |
Table 6. Therapy distribution in patients caused by drug-induced.
Results
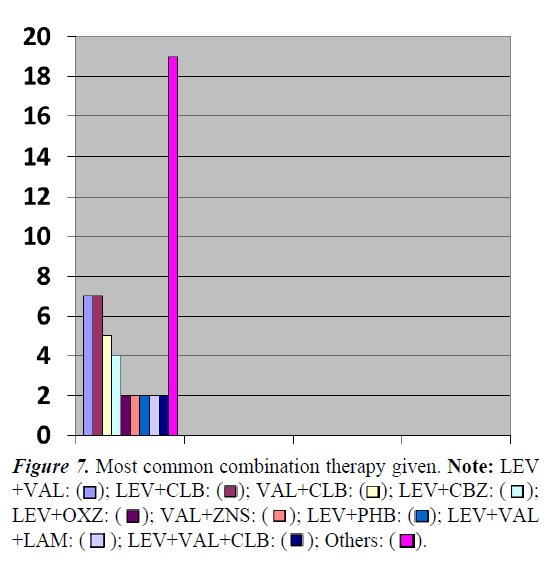
The study analysis revealed higher seizure prevalence in males (54.87%) vs. females (45.13%). Seizure rates peaked in children aged 0-5 years and were lowest in those aged 15-18 years (Table 7) (Figure 7).
| Combination therapy given | No of patients |
|---|---|
| LEV+VAL | 7 |
| LEV+CLB | 7 |
| VAL+CLB | 5 |
| LEV+CBZ | 4 |
| LEV+OXZ | 2 |
| VAL+ZNS | 2 |
| LEV+PHB | 2 |
| LEV+VAL+LAM | 2 |
| LEV+VAL+CLB | 2 |
| OTHERS | 19 |
Table 7. Most common combination therapy given.
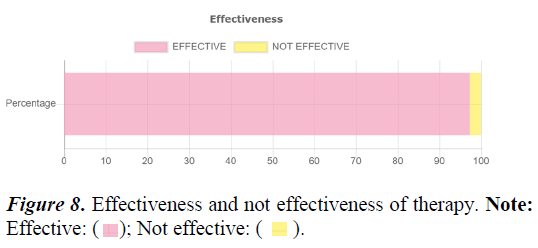
Idiopathic epilepsy was the most common type, followed by febrile seizures. Levetiracetam was the most prescribed medication, with sodium valproate second. Monotherapy was predominant. Notably, only one patient experienced an adverse drug reaction to levetiracetam; see Tables 8 and Figures 8 for details [14-16].
| Effective | Not effective |
|---|---|
| 110 (97.35) | 3 (2.65%) |
Table 8. Effectiveness and not effectiveness of therapy.
Discussion
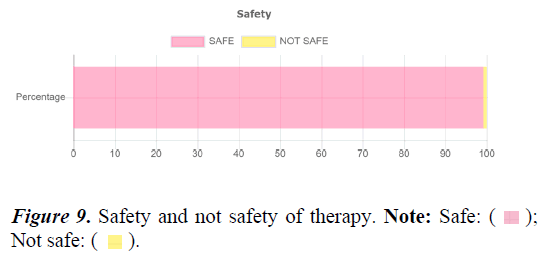
The present prospective observational study was conducted over a period of 6 months, including a total of 113 subjects. Among the participants, male patients accounted for 54.87% of the study population, while female patients represented 45.13%. Although significant gender variation has been observed in various studies, the underlying reasons for this difference remain unclear. The prevalence of seizures was found to be highest among children aged 0-5 years (50.44%) and lowest among those aged 15-18 years (0.88%) [17-21]. According to the American academy of neurology guidelines for epilepsy, EEG is recommended as a routine neurodiagnostic evaluation for diagnosing and classifying different types of epilepsy. However, it is important to note that neither a normal nor an abnormal EEG alone can confirm or exclude the diagnosis of epilepsy (Table 9) (Figure 9) [22].
| Safe | Not safe |
|---|---|
| 112 (99.12%) | 1 (0.88%) |
Table 9. Safety and not safety of therapy.
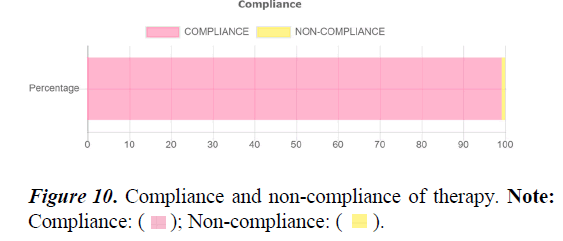
The guidelines also suggest the diagnostic use of MRI and CT scans. In the study group of 113 patients, all participants underwent EEG, while 32 patients (28.31%) required MRI scans. The classification of epilepsy and Seizure syndromes by the International League Against Epilepsy (ILAE) provided a framework for the diagnosis, management and treatment of epilepsy [23]. The observed classification of epilepsy in this study included idiopathic epilepsy (37.17%), symptomatic epilepsy (23.01%), febrile seizures (14.16%), genetic epilepsy (7.96%), myoclonic epilepsy (4.42%), absence epilepsy (3.54%), infantile spasm (3.54%), neonatal epilepsy (2.63%), focal seizure (1.77%), and status epilepticus (1.77%). Among these, tonic-clonic seizures were the most common type. Based on etiology, idiopathic causes accounted for the majority of cases, followed by fever, infection, trauma, and other factors (Table 10) (Figure 10) [24,25].
| Compliance | Non-compliance |
|---|---|
| 112 (99.12%) | 1 (0.88%) |
Table 10. Compliance and non-compliance of therapy.
The study revealed that Levetiracetam (62.8%), sodium valproate (41.59%), clobazam (26.54%), and oxcarbazepine (9.7%) constituted more than 90% of the total anti-epileptic drugs prescribed [26,27]. They are followed by, other antiepileptic drugs, such as Carbazepam (4.42%), Zonisamide (4.42%), Topiramate (2.65%), Phenobarbital (2.65%), Lamotrigine (2.65%), Ethosuximide (2.65%), Vigabatrin (1.76%), Phenytoin (1.76%), Perampanel (0.88%), Lacosamide (0.88%), Clonezepam (0.88%), and Nitrozepam (0.88%), were also prescribed. Monotherapy was observed in 53.98% of patients, while combination therapy was observed in 46.01% of patients. Levetiracetam was the drug of choice, followed by sodium valproate and carbamazepine, for the majority of patients [28]. In terms of specific seizure types, levetiracetam (anticonvulsant) was the most common drug prescribed for generalized seizures, while sodium valproate was commonly prescribed for focal epilepsy. Most commonly given combination therapy of drugs are levetiracetam and valproate, levetiracetam and clobazam followed by valproate and clobazam. The incidence of Adverse Drug Reactions (ADRs) in the study group was low, with only one patient (0.88%) experiencing an ADR related to levetiracetam, manifesting as behavioral changes. Additionally, one patient (0.88%) demonstrated drug non-compliance due to a medication default [29].
Conclusion
This study highlighted a high prevalence of seizures among children aged 0-5 years, with idiopathic epilepsy being the most commonly observed type. Levetiracetam (anticonvulsant) was the most widely prescribed drug, followed by sodium valproate. The incidence of ADRs was minimal, and monotherapy was found to be effective with good patient compliance. Regardless of the therapy type, regular monitoring and follow-up are necessary to achieve seizure control. In some cases, when desired outcomes were not achieved with prescribed anti-epileptic drugs, broad-spectrum anti-epileptics such as sodium valproate were used as effective alternatives.
It is crucial to emphasize the importance of medication adherence and provide patient counseling to optimize treatment outcomes. Clinical pharmacists play a pivotal role in evaluating prescribing patterns, comparing ongoing drug therapies with standard treatment guidelines, and promoting the rational use of drugs while minimizing the incidence of ADRs.
References
- Shorvon SD, Andermann F, Guerrini R, et al. The causes of epilepsy: Common and uncommon causes in adults and children. Cambridge University Press 2011; 14.
- Hauser WA. Epilepsy: Frequency, causes and consequences. Epilepsy foundation of America. 1990; 49(4): 342.
- Commission on classification and terminology of the international league against epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia 1989; 30(4): 389-99.
- Lowenstein DH, Bleck T, Macdonald RL. It's time to revise the definition of status epilepticus. Epilepsia. 1999; 40(1): 120-2.
- Berg AT, Berkovic SF, Brodie MJ, et al. Revised terminology and concepts for organization of seizures and epilepsies: Report of the ILAE commission on classification and terminology, 2005–2009. 2010; 51(4): 676-85.
- Strug LJ, Clarke T, Chiang T, et al. Centrotemporal sharp wave EEG trait in rolandic epilepsy maps to Elongator Protein Complex 4 (ELP4). Eur J Hum Genet 2009; 17(9): 1171-81.
- Lal D, Reinthaler EM, Altmüller J, et al. RBFOX1 and RBFOX3 mutations in rolandic epilepsy. PloS One 2013; 8(9): e73323.
- Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 2012; 17(1): 3-23.
- Ramya A, Sravya P, Kumar V, et al. Pediatric seizures-A prospective study on drug utilization pattern and its outcome in a teritiary care hospital. World J Pharmaceutical Res 2015; 4: 1561-1572. [Crossref]
[Google Scholar][Indexed]
- Dholakia HJ, Singh A. An analysis of prescription pattern of antiepileptic drugs in a pediatric population of tertiary care teaching hospital. Int J Toxicol Pharm Res 2022; 12 (6); 158-165.
- Raphel J, John NN. Drug utilisation pattern of anti-epileptic agents among paediatric patients with epilepsy. Int J Pharma Res Health Sci 2019; 7(4): 3043-3046.
- Hasan SS, Bahari MB, Babar ZU, et al. Antiepileptic drug utilisation and seizure outcome among paediatric patients in a Malaysian public hospital. Singapore Med J 2010; 51(1): 21–27.
- Joshi R, Tripathi M, Gupta P, et al. Prescription pattern of antiepileptic drugs in a tertiary care center of India. Indian J Pharmacol 2020; 52(4): 283–289.
- Egunsola O, Choonara I, Sammons HM, et al. Safety of antiepileptic drugs in children and young people: A prospective cohort study. Seizure 2018; 56: 20-25.
- Kwong KL, Tsui KW, Wu SP, et al. Utilization of antiepileptic drugs in Hong Kong children. Pediatric Neurology 2012; 46(5): 281-6.
- Albsoul-Younes A, Gharaibeh L, Murtaja AA, et al. Patterns of antiepileptic drugs use in epileptic pediatric patients in Jordan. Neurosciences Journal 2016; 21(3): 264-7.
- Bourgeois FT, Olson KL, Poduri A, et al. Comparison of drug utilization patterns in observational data: Antiepileptic drugs in pediatric patients. Pediatric Drugs 2015; 17: 401-10.
- Tan WW, Kong ST, Chan DW, et al. A retrospective study on the usage of antiepileptic drugs in Asian children from 2000 to 2009 in the largest pediatric hospital in Singapore. Pharmacoepidemiology Drug Saf 2012; 21(10): 1074-80.
- Maity N, Gangadhar N. Trends in utilization of antiepileptic drugs among pediatric patients in a tertiary care hospital. Curr Neurobiol 2011; 2: 117-23.
- Suman A. Study of adverse drug effects of antiepileptic drugs used in pediatric patients in a tertiary care rural hospital-A pharmacovigilance study. Journal of Young Pharmacists. 2017; 9(1): 60.
- Putignano D, Clavenna A, Campi R, et al. Antiepileptic drug use in Italian children over a decade. Eur J Clin Pharmacol 2017; 73: 241-8.
- Kousalya K, Swathi Cherukuri DP, Padmasani LN, et al. Drug utilization pattern of antiepileptics and their adverse effects in pediatrics. World J Pharmaceutical Res 2014; 3(9): 504-13.
- Christian P, Patel J, Deshapande S, et al. Study use of antiepileptic drugs in pediatric ward at GMERS hospital, Gandhinagar, India. Indian J Pharm Pract 2020; 13(2): 174-179.
- Mattsson P, Tomson T, Edebol Eeg‐Olofsson K, et al. Association between sociodemographic status and antiepileptic drug prescriptions in children with epilepsy. Epilepsia 2012; 53(12): 2149-55.
- Wang Z, Cramer J, Li X, et al. Antiepileptic drug use patterns in the pediatric and adult medicaid population (P06. 110). 2012; 78(1_supplement): 110.
- Dwajani S, Meghana KS, Krithika S, et al. Treatment pattern of antiepileptic drugs in pediatric with epilepsy. Pharm Clin Pharm Res 2021; 6(3): 141-8.
- Khan PM, Jha A, Pathak S, et al. Antiepileptic drug utilization in pediatric patients at a tertiary care rural teaching hospital of central India. Res J Pharm Pharmacodyn 2015; 7(1): 5-10.
- Nalluri KK. Drug utilization evaluation of antiepileptic drugs in pediatric population at a secondary care hospital. Value in Health 2016; 19(3): A68.
- Dave HH, Trivedi NA. Drug utilization pattern of antiepileptic agents among pediatric epilepsy at tertiary care teaching hospital of Gujarat: A cross sectional study. 2018; 7(8): 59-63.
 ):
0-5 years; (
):
0-5 years; ( ): 5-10 years; (
): 5-10 years; ( ): 10-15 years; (
): 10-15 years; ( ): 15-18 years.
): 15-18 years.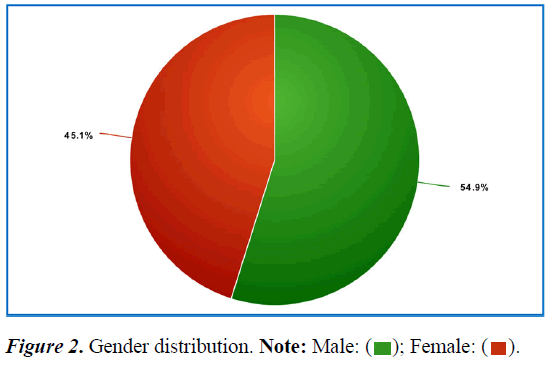
 ); Combination therapy: (
); Combination therapy: ( ).
).