- Biomedical Research (2012) Volume 23, Issue 2
Evaluation of non-pharmacological method-transcervical foley catheter to intravaginal misoprostol and Prostaglandin E2 gel for preinduction cervical ripening
Sujata1*, Iqbal B2, Das V1, Agarwal A1, Singh R1
1Department of Obstetrics and Gynaecology, CSM Medical University, Lucknow, India
2Department of Physiology, CSM Medical University, Lucknow, India.
- *Corresponding Author:
- Sujata Deo
Department of Obstetrics and Gynaecology.
CSM Medical University
Lucknow
India.
Accepted date: February 17 2012
Abstract
The efficacy of intracervical Foley catheter with misoprostol (PGE1) and dinoprostone (PGE2) for preinduction cervical ripening, induction of labour, mode of delivery, induction to delivery interval and maternal complications has been compared.. Women who were admitted to hospital and met criteria for entrance in the trial were counseled and enrolled after informed consent. Inclusion criteria included full term singleton gestation, cephalic presentation, with one or more of the common indication for induction of labour including post-term pregnancy, preeclampsia, oligohydramnios etc. Bishop score <6 was necessary criteria for entry. Exclusion criteria included rupture of membranes, antepartum bleeding, placenta praevia, previous induction or preinduction agent during the pregnancy. Each woman was assigned to receive cervical ripening with a transcervical Foley catheter or misoprostol or dinoprostone, by selection of the next consecutive envelope. The group assigned misoprostol had 25 ?g of misoprostol placed intravaginally in post fornix, every 4 hours for a maximum 8 doses.The women assigned to the disoprostone group, received a maximum of 3 doses of vaginal gel, each containing 2 mg of dinoprostone in their post fornix once every 6 hours.In both these groups subsequent doses were withhold if regular uterine contraction was established (at least 1 in 10 minutes regularly), tachysystole (6 contraction in 10 minutes), uterine hyperstimulation or nonreassuring FHR or rupture of membranes occurred. Oxytocin was begun 4 hours after the last dose of misoprostol or dinoprostone in women who did not have spontaneous labour (regular contraction with continued cervical change). All the women underwent cardiotocography 20 minutes after administration of the medication or insertion of the catheter. Primary outcomes included change in Bishop score. Secondary outcome measures included total time for induction, delivery route, uterine tachysystole, uterine hypertonus, subject comfort. A total of 160 women were enrolled in the study. Two were excluded because of deviation from entry criteria. So of the 156 subjects, 50 were assigned to treatment with Foley Catheter, 54 with Misoprostol and 52 with Dinoprostone. The shortest mean induction to delivery was obtained with catheter (19.18h) as compared to Dinoprostone (20.12hr) and Misoprostol (21.04hr). The cervical Ripening with Foley catheter is the safe method for labour induction. Induction with Misoprostol and Dinoprostone is equally effective and safe.
Introduction
Labour is commonly induced in response to a number of fetal and maternal situations, including post term pregnancy, preeclampsia and rupture of membranes without the onset of spontaneous contraction. Induction rates between 10% and 25% are common in industrialized countries. A potential effect of induction is an increased risk of caesarean delivery and its complications [1-8].
When the cervix is unfavourable, cervical ripening is recommended to increase the likelihood of successful induction [1-5].
Ripening of cervix may be achieved by both pharmacological and non-pharmacological (mechanical method) methods.
The pharmacological preparation includes the prostaglandins. Two different preparations of Prostaglandins (A) Prostaglandin E2 (PGE2) or dinoprostone which is unstable at room temperature and requires refrigeration, is most commonly used; (B) Prostaglandin E (PGE1) analogue misoprostol, FDA approved for treatment of gastric ulcers, has also been evaluated for possible use in cervical ripening and induction of labour since 1992 [9] and it has been seen that misoprostol is actually more effective than PGE2. With the use of this analogue (PGE1) there are more chances of uterine hyperstimulation resulting in change in fetal heart rate (FHR) pattern and staining of the amniotic fluid with meconium but without any apparent deleterious effect on the outcome. In women, with previous attempting VBAC (Vaginal birth after C- section) caesarean section, there are increased chances of uterine rupture due to this uterine hyperstimulation.
Non-pharmacological method includes the transcervical use of foley catheter for cervical ripening and induction of labour. Embrey and Mollison [10] first described using a transcervical Foley catheter for cervical ripening. Obed and Adewele [11] documented its effectiveness by increasing Bishop scores in women with unripe cervix. Catheter appears to induce labour not only through direct mechanical dilatation of cervix but also by stimulating endogenous release of Prostaglandin but no study has compared the efficacy of the above three approaches for cervical ripening and induction of labour.
The objective of this study to compare the efficacy of intracervical foley catheter with misoprostol (PGE2) and dinoprostone (PGE1) for preinduction cervical ripening, induction of labour, mode of delivery, induction to delivery interval and maternal complications.
Material and Method
This prospective randomized study was approved by the Ethics Research Committee at the CSM Medical University (India) where it was conducted for 1 year duration.
Women who were admitted to hospital and met criteria for entrance in the trial were counseled and enrolled after informed consent. Inclusion criteria included full term singleton gestation, cephalic presentation, with one or more of the common indication for induction of labour including post-term pregnancy, preeclampsia, oligohydramnios etc. Bishop score <6 was necessary criteria for entry. Exclusion criteria included rupture of membranes, antepartum bleeding, placenta praevia, previous induction or preinduction agent during the pregnancy.
Using computer-generated random allocation numbers, methods of preinduction cervical ripening were placed consecutively in opaque envelopes. Each woman was assigned to receive cervical ripening with a transcervical foleycatheter or misoprostol or dinoprost, by selection of the next consecutive envelope.
In women assigned to transcervical foley catheter, a 16 F Foley catheter with 30 mL balloon was inserted into the endocervical canal under direct vision by doing a perspeculum examination. The catheter was advanced into the endocervical canal. Once past the internal os, the balloon was filled with 30 ml of sterile water and the catheter taped to the inner-thigh to maintain traction. The catheter was checked for extrusion of the balloon from the cervix every 6 hours by cervical examination. If the balloon had not been extruded, the catheter was adjusted to continue gentle traction. Each subject underwent cardiotocography for 20 min after Foley catheter placement. Then she was allowed to ambulate with intermittent fetal heart rate (FHR) test assessment every 30 minutes. The position and traction of the balloon were checked once or twice each hours and the catheter remained in place until the balloon was expelled spontaneously.
Immediate following such expulsion, or alternatively when the Bishop score attained a value of >6, for acceleration of labour the membrane were ruptured artificially or oxytocin was begun if necessary.
The group assigned misoprostol had 25 μg of misoprostol placed intravaginally in post fornix, every 4 hours for a maximum 8 doses.
The women assigned to the disoprostone group, received a maximum of 3 doses of vaginal gel, each containing 2 mg of dinoprostone in their post fornix once every 6 hours.
In both these groups subsequent doses were withhold if regular uterine contraction was established (at least 1 in 10 minutes regularly), tachysystole (6 contraction in 10 minutes), uterine hyperstimulation or non-reassuring FHR or rupture of membranes occurred. Oxytocin was begun 4 hours after the last dose of misoprostol or dinoprostone in women who did not have spontaneous labour (regular contraction with continued cervical change). All the women underwent cardiotocography 20 minutes after administration of the medication or implantation of the catheter.
Our intent was to evaluate the success of preinduction cervical ripening, by noting so the primary outcome measure i.e change in Bishop score. For women in the Foley catheter group, that was defined as the difference between initial cervical examination and examination at the time of extrusion. In the misoprostol and dinoprostone group, it was the difference between initial examination and Bishop score assigned with the last dose of misoprostol and dinoprostone.
Secondary outcome measures included total time for induction (time of placement of ripening agent until delivery), delivery route, uterine tachysystole (defined as six contraction in 10 minutes, in two consecutive 10 minutes periods), uterine hypertonus (contraction lasting longer than 3 minutes), subject comfort as women were asked to evaluate their discomfort on a visual scale from 0 to 10.
Data Analysis
Data were analysed by using SPS version 15.0. Qunatitative variable age, gestational age, and preinduction Bishop score was presented by mean ± standard deviation. Student T- test was performed to compare these among 3 groups. Frequency and Percentage was computed for presentation of parity, indication of induction, cervical ripening, mode of delivery, induction to delivery interval and maternal complications.Chi square test was applied to compare these variables among 3 groups at p<0.05 level of significance.
Results
One hundred sixty women were enrolled for the study. Two were excluded because of deviation from entry criteria. One woman received misoprostol and Foley catheter both and one women received 50 μg misoprostol. Results of one hundred fifty eight women were analyzed. Depending on the cervical ripening agent to which they were randomized were divided into the following three groups. Group I (n=50) received Foley catheter, Group II (n=54) received misoprostol and Group III (n=52) received dinoprostone.
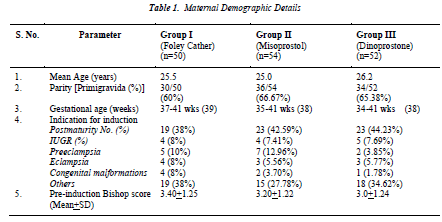
The demographic characteristics of the women in the three groups, documented in Table I, demonstrated no significant difference in mean age, parity, gestational age, Bishop score at entry. The indication for induction of labour were comparable.
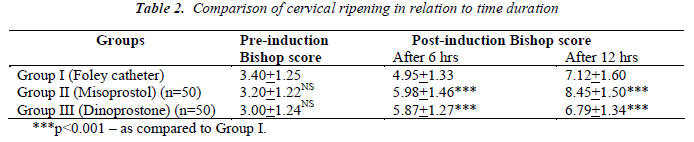
Comparison of cervical ripening in relation to time duration shown in Table II. There was no statistically significant difference between the groups in terms of Bishop score after 6 hours and 12 hours. But on comparison of Group II (misoprostol) and Group III (Dinoprostone) to Group I (Foley) it was statistically significant (p<0.001).
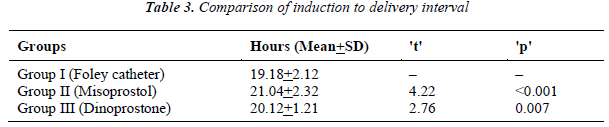
With regards to outcomes concerning labour, there were significant differences between the induction to delivery interval between all 3 groups (Table III).
The time duration between induction to delivery was 19.18+2.12 hours, 21.04+2.32 hours; 20.12+1.21 hours (mean+SD) for catheter, misoprostol and dinoprostone group, respectively and on comparison of Group I (Foley) to Group II (misoprostol) and Group III (dinoprostone) it was statistically significant (p<0.001).
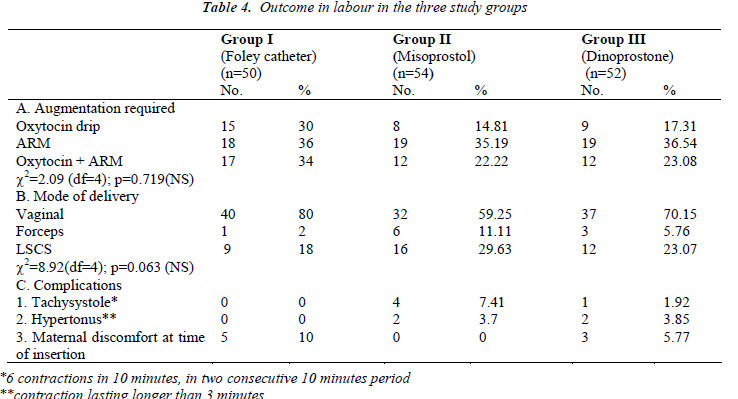
After initiation of induction of labour in Group I (Foley), all women required augmentation in which 30% required Oxytocin drip, 36% required artificial rupture of membrane (ARM) and remaining 34% women required ARM+oxytocin both. In Group II (misoprostol) 15 women had spontaneous rupture of membrane while 39 women required augmentation and maximum number of women (35.19%) required ARM. In Group III (Dinoprostone) 12 women had spontaneous rupture of membrane while 40 women required augmentation and maximum number of cases (36.54%) delivered following only ARM (Table IVA). Table IVB shows the mode of delivery, maximum number of women delivered vaginally. In Group I (Foley) Group I (Foley), 18% women, Group II (misoprostol), 29.63% and in Group III (dinoprostone), 21.15% women required LSCS. The difference were not statistically significant.
Maternal complications were infrequent in all groups. The most frequent complaints in group 1 (Foley group) was maternal discomfort at the time of insertion of foley catheter(10%). Uterine contractile abnormalities like tachysystole (6 contraction in 10 minutes, in two consecutive 10 minutes period) was present in 7.41% women in group 2 (misoprostol group) while it was present in 1.92% women in group 3 (Dinoprostone group). Uterine hypertonus (contraction lasting longer than 3 minutes) were frequent in both Group II (misoprostol group) & group 3(Dinoprostone group. (Table IVC).
Discussion
We found that a pharmacologic method i.e. misoprostol (PGE1), dinoprostone (PGE2) and a mechanical method, the Foley catheter for cervical ripening were similarly effective most of the time. The purpose of this study was to highlight a simple method for ripening of cervix that may be suitable for an obstetrical unit.
In this study 156 women were selected by randomization 50 women were in Group I (Foley), 54 women in Group II (misoprostol) and 52 women in Group III (Dinoprostone). Demographic, socio-economic and obstetric characteristics were comparable between the three study groups. None of these characteristics showed any significant differences between these three groups.
In our study we found that there was no statistically significant difference in all 3 groups in terms of Bishop score after 6 hours and 12 hours (i.e. pre-induction cervical ripening). A study by Rabindranath [12] et al. concluded that extra-amniotic Foley catheter balloon is more effective than intracervical PGE2 gel for preinduction cervical ripening. Similar results were also found by another study, Sciscione AC [13] et al. concluded that use of Foley catheter result in higher post-induction Bishop score, greater change in Bishop score and shorter induction time than PGE2. Ghezz [14] et al. also concluded that Foley catheter could be a better alternative then intravaginal PGE2 gel for cervical ripening. A review documented the superiority of the catheter over PGE2 and showed the catheter to have the same efficacy as application of PGE1, but PGE1 have fewer abnormalities in contraction. In contrast to our observation, another recent study done by Owalabi AT [15] concluded that a 50 μg dose of misoprostol is more effective than a balloon catheter in inducing labour, with the same degree of safety. Adeniji OA [16] et al. concluded that intravaginal misoprost is as effective a preinduction cervical ripening agent as transcervical Foley catheter. Greybush [17] et al. documented that a supracervical foley catheter had similar efficacy in cervical ripening to intravaginal misoprost. Sherman [18] et al. showed the change in cervical ripening around score 4 when intracervical foley catheter was used as inducing agent.
In our study it was found that the interval of time between induction and delivery in general and vaginal delivery in particular is shorter with the foley catheter than with the two other treatment modalities, which are similar in this respect. A study done by Prager M [19] et al. concluded that transcervical Balloon catheter can be used to achieve effective and safe for induction of labour while misoprostol and dinoprostone are also effective and safe for induction of labour. Ghezzi F et al. reported that induction of labour to delivery time were similar in both Foley catheter and PGE2 gel. A review documented the superiority of catheter over PGE2 and showed the Foley catheter to have the same efficacy as application of PGE1, while causing fewer abnormalities in contraction. In contrast to our observation another study concluded that 50 microgram dose of misoprostol is more effective than a balloon catheter in inducing labour, with the same degree of safety.
In our study augmentation by oxytocin drip or artificial rupture of membrane (ARM) of labour occurred more in dinoprostone group.Similar results were observed in study of A.T. Owolabi [15] et al.
We observed that more women had spontaneous vaginal delivery in Foley catheter group than misoprostol and dinoprostone group through the difference was not statistically significant. Incidence of LSCS was more in misoprostol group rather than in Foley catheter group and dinoprostone group. Rozenberg [20] et al. demonstrated that the rate of caesarean section performed for acute fetal distress was higher with use of misoprostol. However, Gemund [21] et al. showed lower operative delivery rate in the misoprostol group. M. Prager [19] et al. showed no difference in mode of delivery between all three treatment modalities. Other comparison of PGE2 with the catheter procedure have concluded that the latter demonstrates either a higher efficacy or a lower incidence of caesarean section, a difference that may reflect the use of different Protocols.
We observed that misoprostol treated women have more uterine contractile abnormalities (hyper stimulation syndrome) while no cases of hyper stimulation were noted in the Foley catheter arm in this study. This result was also supported as well as contradicted by literature. In a report by Perry [22] et al. showed that Foley-dinoprostone group had a lower frequency of hyper-stimulation syndrome than misoprostol.
Conclusion
The cervical ripening with foley catheter has the advantage of low cost, simple, safe and lack of systemic and serious side effects and induces significant ripening and dilation of cervix and shorter induction to delivery time.Induction with Misoprstol or Dinoprostone is equally effective and safe. But because of the lower cost and greater easy of storage of the Misoprostol favours its use. In the case of women where placement of the catheter in the cervix is difficult initial ripening with Misoprostol and subsequent insertion of a ballon catheter can be considered as a best option.
Acknowledgements
We would like to sincerely thanks to the residents, research Team and nurses staff of CSM medical University for their engagement in this study.
References
- Crane J, Leduc L, Farine D, Hodges S, Reid GJ, Van Aerde J. Induction of labour at term—SOGC Clinical Practice Guideline. J Obstet Gynaecol Can 2001; 23 (8): 717-728
- Wing D. Induction of labor: indications, techniques, and complications. (www.UpToDate.com). 31 July 2006.
- Sujata/ Iqbal/Das/Agarwal/Singh Biomedical Research 2012 252 Volume 23 Issue 2 3. American College of Obstetricians and Gynecologists. Induction of Labor. ACOG Practice Bulletin. Washington, DC: American College of Obstetricians and Gynecologists, 1999; 10.
- Royal College of Obstetricians and Gynaecologists. Induction of Labour. Guideline. No. 9. London, UK: RCOG Press, 2001.
- Hofmeyr GJ. Induction of labour with an unfavourable cervix. BestPract Res Clin Obstet Gynaecol 2003;17: 777-794.
- Cammu H, Martens G, Ruyssinck G, Amy JJ. Outcome after elective labor induction in nulliparous women: a matched cohort study. Am J Obstet Gynecol 2002;186:240–4.
- Seyb ST, Berka RJ, Socol ML, Dooley SL. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol 1999; 94: 600-607.
- Luthy DA, Malmgren JA, Zingheim RW. Cesarean delivery after elective induction in nulliparous women: the physician effect. Am J Obstet Gynecol 2004; 191: 1511-1515.
- Margulies M, German Campos Pérez , LilianaS Voto. Misoprostol to induce labour. The Lancet, 1992; 339: 64
- Embrey, Mollison BG. The unfavourable cervix and induction of labour using a cervical balloon. BJOG 1967; 74: 44.
- Obed JY, Adewole IF. The unfavourable cervix: improving the Bishop score with the Foley's catheter. West Afr J Med 1994; 13 (4): 209-212
- Rabindranath D, Vanita, Pallab R, Indu G. Comparison of extraamniotic Foley catheter and intracervical prostaglandin E2 gel for preinduction cervical ripeningActa Obstetricia et Gynecologica Scandinavica. 2005; 84: 362–367
- Sciscione AC, Nguyen L, Manley J. Colmorgen GA randomized comparison of transcervical Foley catheter to intravaginal misoprostol for preinduction cervical ripening. Obstet Gynecol. 2001; 97 (4): 603-607.
- Ghezzia F, Massimoa F, Raiob L Extra-amniotic Foley catheter and prostaglandin E2 gel for cervical ripening at term gestation.2001; 97: 183-187
- Owolabi AT, Kuti O, Ogunlola IO. Randomised trial of intravaginal misoprostol and intracervical Foley catheter for cervical ripening and induction of labour. J Obstet Gynaecol. 2005; 25 (6): 565-568.
- Adeniji OA, Oladokun A, Olayemi O. Pre-induction cervical ripening: transcervical foley catheter versus intravaginal misoprostol J Obstet Gynaecol 2005 Feb; 25 (2): 134-139.
- Greybush M, Singleton C, Atlas RO, Balducci J, Rust OA. Preinduction cervical ripening techniques compared. J Reprod Med. 2001; 46 (1): 11-17.
- Sherman DJ, Frenkel E, Tovbin J, Arieli S . Ripening of the unfavorable cervix with extraamniotic catheter balloon: clinical experience and review. Obstet Gynecol Surv. 1996; 51 (10): 621-627.
- Prager M, Eneroth-Grimfors E, Edlund M, Marions L A randomised controlled trial of intravaginal dinoprostone, intravaginal misoprostol and transcervical balloon catheter for labour induction. BJOG 2008; 115 (11): 1443-1450.
- Rozenberg P, Chevret S, Goffinet F, et al. Induction of labour with a viable infant: a randomised clinical trial comparing intravaginal misoprostol and intravaginal dinoprostone. Br J Obstet Gynaecol 2001; 108: 1255- 1262.
- Van Gemund N, Scherjon S, LeCessie S. A randomised trial comparing low dose vaginal misoprostol and dinoprostone for labour induction. BJOG. 2004; 111 (1): 42-49.
- Perry KG, Larmon JE, May WL, Robinette LG, Martin RW. Cervical ripening: a randomized comparison between intravaginal misoprostol and an intracervical balloon catheter combined with intravaginal dinoprostone. Am J Obstet Gynecol 1998; 178: 1333-1340.