Research Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2022) Volume 12, Issue 91
Evaluate the safety and efficacy of antibiotics in postoperative Hernioplasty and Herniorrhaphy.
Shaik Shabana Tahaseen*, Bogyam Bhavana, Veldurthi Hari Sushma, L Grace
Department of Pharmacy Practice, Dr. KV Subba Reddy Institute of Pharmacy, Kurnool, Andhra Pradesh, India
- Corresponding Author:
- Shaik Shabana Tahaseen
Department of Pharmacy Practice
Dr. KV Subba Reddy Institute of Pharmacy
Kurnool, Andhra Pradesh, India
E-mail: tahaseen8985@gmail.com
Received: 25-June-2022, Manuscript No. AABPS-22-67680; Editor assigned: 28-June-2022, PreQC No. AABPS-22-67680(PQ); Reviewed: 13-July-2022, QC No. AABPS-22-67680; Revised: 16-July-2022, Manuscript No. AABPS-22-67680(R); Published: 23-July-2022, DOI:10.35841/2249-622X.91.132
Citation: Tahaseen SS, Bhavana B, Sushma VH et al. Evaluate the safety and efficacy of antibiotics in postoperative Hernioplasty and Herniorrhaphy. Asian J Biomed Pharmaceut Sci. 2022;12(91):132
Abstract
Aim: To evaluate the safety and efficacy of antibiotics in post-operative Hernioplasty and Herniorrhaphy. Objectives: Assessing the clinical efficacy of post-operative antibiotics like ceftriaxone, amikacin and piperacillin plus tazobactam in reducing surgical site infections. By measuring the wound status of patients by using wound grading during postoperative follow up intervals. To determine social demographic details and categoric the types of hernia in study population. Methods: This is a prospective observational study performed and conducted at General surgery department, Government General Hospital, Kurnool. Individual were analyzed by particulars of age, sex, date of admission and date of surgery, investigations, past history, comorbid conditions like hypertension, diabetes etc., patients were selected on the basis of inclusion and exclusion criteria. Results: A totals of 58 patients the distribution of male (75.8%) and female (24.1%). The majority of type of hernia is direct inguinal hernia of 17(29.3%) when compared to all types of hernias. The administration of post-operative antibiotics like ceftriaxone + metronidazole, piperacillin/ tazobactam + metronidazole, ceftriaxone + metronidazole + amikacin and sulbactam sodium + cefoperazone sodium + metronidazole, is markedly reduced surgical site infections. Wound grades in post-operative patients were comes under grade 0 was more compared to grade1 and grade 2. Conclusion: In this study the different groups of antibiotics like cephalosporin’s, Anti protozoal drugs and aminoglycosides in post-operative surgeries are showing equal effectiveness in reducing surgical site infection in both comorbid and noncomorbid conditions.
Keywords
Post-operative, Hernioplasty, Herniorrhaphy, Antibiotics
Introduction
Definition
A hernia is defined as protrusion of whole or a part of viscous through the wall that contains it. The term can be applied to protrusion of a muscle through its facial covering or of brain through fracture of skull or through foramen magnum into the spinal card. The commonest variety of hernia is protrusion of a viscous or a part of it through the abdominal wall [1,2].
Epidemiology
At first hernia was recorded In Egyptian papyrus 1500BC and then it was regarded as a social stigma. It will occur in all type of Male and Female. In all these abdominal hernias are common. It has approximately 10% of the general surgical workload. The relative frequency of external abdominal hernias. Inguinal hernias account for 75% of abdominal wall hernias and life time risk of 27% in men and 3% in women (Table 1).
| Type of hernia | Incidence |
|---|---|
| Epigastric | 1% |
| Incisional | 10% |
| Inguinal | 78% |
| Femoral | 7% |
| Umbilical | 3% |
| Others (rare) | 1% |
Table 1. Relative frequency of external abdominal hernias.
Classification
Hernias are classified into congenital or acquired shown in Congenital:
These are of pre-formed sac that occurs as consequence of intra uterine development.
Acquired
This acquired type has two types:
Primary hernia
These occur at natural points such as Structure penetrates the abdominal wall Muscles and Apo neuroses fail to overlap normally Fibrosis tissue develops to close defect.
Secondary hernia
These develop at surgical site and injury to wall which contents of a body cavity.
• Congenital
• Acquired
• Indirect inguinal hernia
• Direct inguinal hernia
• Umbilical hernia
• Femoral hernia
• Incisional hernia
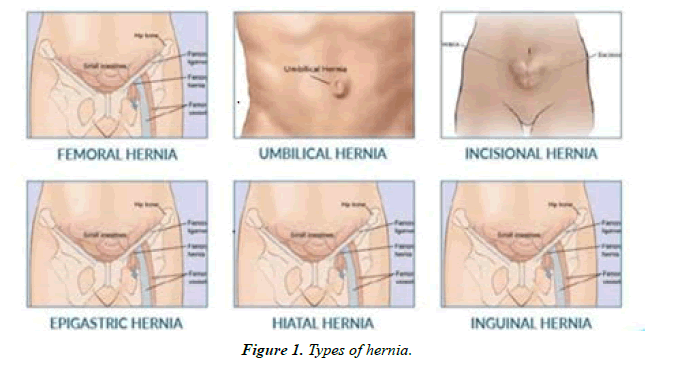
• Epigastric hernia (Figure 1)
Aetiology
The hernia is mainly occurring based upon the two factors which are predisposing to hernia that develops intra activity pressure and weak abdominal wall. In abdomen the pressure occurs by heavy lifting, cough, straining to pass wire benign prostatic hyperplasia or carcinoma, straining to pass faucesconstipation or large -bowel obstruction, abdominal distension that may presence of an intra-abdominal contents. In weak abdominal wall it occurs by advancing age, malnutrition -macronutrients or micronutrients, paralysis of motor nerves, abdominal collagen metabolism.
Pathophysiology
Defect or weakness in the muscular wall may be, congenital or acquired weakness or caused by trauma. Increased the intraabdominal pressure as a result of risk factors. As a results of weakness of the abdominal wall and increased pressure the abdominal contents can protrude causing herniation When the contents of the hernial sac can be replaced into the abdominal cavity by manipulation, the hernia is said to be reducible. Irreducible and incarcerated hernia refers to hernias that cannot be replaced by manipulation. When the pressure from the hernial ring cuts off the blood supply to the herniated segment of the bowel, it becomes strangulated. Signs and Symptoms: For Inguinal, Incisional, Femoral, Umbilical, Epigastric these are signs and symptoms:
1. Swelling beneath the skin of abdomen or groin
2. Constipation and bloody stools
3. Discomfort in abdomen when lifting or bending
4. Burning sensation at bulge
5. Weakness in groin
6. Shooting pain
7. Pain around testicles
8. Vomiting Diagnosis tests
Ultra sound Computer tomography scans (CT-scan) Magnetic resonance imaging (MRI).
Management of hernia
Basically, there is no pharmaceutical treatment for hernia, if hernia occurs it should be preceded with surgical procedure. It is going to be done in mainly two ways:
• Open mesh repair
• Laparoscopic technique
Surgical repair of inguinal hernias is a common procedure in adult men. However recurrence of hernia has been reported to occur after repair in 15 percent or more cases, and postoperative pain and disability are frequent, when traditional surgical methods are used, outcomes after repair of recurrent hernias have been worse than after primary repair. After the introduction of tension-free surgical repair with the use of prosthetic mesh, recurrence rates were reported to be less than 5 percent and patients’ comfort was reported to be substantially improved over that obtained by the traditional, tension producing techniques. Local anesthesia is used, and patients are discharged within a few hours. A laparoscopic method of performing a tension-free repair has subsequently been reported to result in low recurrence rates and to be associated with substantially less pain in the immediate postoperative period and earlier return to normal activities than the open-repair technique. The laparoscopic technique however requires general anesthesia, and it is more often associated with serious intraoperative complications than is open repair, although such type of complications are infrequent. We conducted a multicenter, randomized trial to compare recurrence rates and other outcomes after either of two standardized tension-free herniorrhaphies: open repair and laparoscopic repair [3].
Role of prophylactic antibiotics definition
Prophylactic antibiotics are defined as antibodies used to prevent infection in the absence of infection. The microorganisms are attacked at their lodgment in the wound or the body cavity before their colonization. The aim is to prevent sepsis rather than to treat sepsis. Administration of prophylactic antibiotics is a scientifically approves method pf primary prevention of post-operative wound infection. The role of prophylactic antibiotics is to support the body’s ability to resist contamination. Therefore to be effective they must be administered before the bacterial inoculation.
Indication of antibiotic prophylaxis
Prophylactics antibiotics are indicated when the surgical procedure has a higher chance of contamination or when the resistance of the patient is low. Traditionally antibiotic prophylaxis is indicated in clean contaminated and when contamination occurs accidentally at the time of surgery. They are also indicated in clean procedures when prosthetic implants are used. The role of antibiotics in contaminated procedures is essentially therapeutic. Is there a role for prophylactic antibiotics in clean surgery? Role of prophylactic antibiotics in surgery remains controversial. Studies conducted during late 50’s and early 60’s concluded that there is no role of prophylactic antibiotics in surgery. On the contrary it was believed that they resulted in a higher infection rate.
Principles of Antibiotic Prophylaxis
Timing of antibiotic prophylaxis
Is there a relationship between the timing of antibiotic administration and wound infection? An antibiotic to be effective as a prophylactic agent would be present in an appropriate concentration at the time of the contamination.
Vulnerable period
The duration of the operative procedure represents the decisive period that has been most aptly called the vulnerable period. The rationale behind the use of prophylactic antibiotics is to boost the host defense mechanism to defeat the bacterial challenge during the vulnerable period. If the antibiotics are given too early, no, antibiotic activity might be left in the tissues to resist the contamination during the surgery. So much so, if the antibiotics are given too late the bacterial load might be too high to resist the infection. Classified antibiotic prophylactic according to the timing of administration as:
Early: when the antibiotic is administered within 2 to 24 hours before surgery.
Pre-operative: when administered 2 hours before the incision.
Peri-operative: when administered during the first 3 hours after the incision.
Post-operative: when administered 3 to 24 hours after the incision.
Duration of prophylactic antibiotic administration.
Prophylactic antibiotics can successfully reduce incidence of post-operative wound infection, in this difficulty some suggest short course and some suggest large course. After all type of studies single dose prophylaxis just prior to incision.
Antibiotic Treatment
Role of antibiotics
The role of antibodies is a well-established infection, is an adjuvant to the local wound management, though they can be curative in the early stages. When used appropriately they can be preventing septicemia. They can be used either systemically or locally. Clinical response should be apparent within 36 hours after starting the antibiotics and should be continued for 5 days. Prolong usage leads to toxic effects and super infection. If there is no obvious clinical improvement, either the organism causing wound might not be sensitive to the antibiotic used or the antibiotic dosage may be inappropriate. Antibiotics are ineffective in the presence of necrotic tissue. Hence adequate debridement is essential [4].
Pharmacotherapy
In hernia people will go through the surgery after surgery to reduce the infection rate antibiotic therapy should be used. Here third generation cephalosporin’s are used to treat patients
Ceftriaxone
It has longer duration of action. Its t 1/2 is 8 hours, penetrating once, or at most twice daily dosing. Penetration into CSF is good and elimination occurs equally in urine and bile. It shows high efficacy in serious infections. Brand name: Rocephin
Mechanism of action
It works by inhibiting the muco peptide synthesis in bacterial cell wall. The beta-lactam ceftriaxone binds to carboxyl peptidases, endo peptidases, and Tran’s peptidases in the bacterial cytoplasmic membrane. These enzymes are involved in cell-wall synthesis and cell division. Binding of ceftriaxone to these enzymes causes the enzyme to lose activity, so bacteria produce cell wall causing cell death.
Route of administration
• It is only given as parental route either as Intramuscular or Intravenous.
• Dosage: 1 to 2gm
Side effects
• Pain
• Vomiting
• Diarrhea
• Headache
• Dizziness
• Loss of appetite
Adverse effects
• Bleeding
Amikacin
Amikacin is an antibiotic medication used for many bacterial infections. This includes joint infections, intra-abdominal infections, meningitis, pneumonia, sepsis and urinary tract infections. This is also used for multi-drug resistant tuberculosis. Brand name: Amikin
Mechanism of action
It binds to bacterial 30S ribosomal subunits and interferes with mRNA binding and tRNA acceptor sites, interfering with bacterial growth. This leads to disruption of normal protein synthesis and production of non-functional toxic peptides. It is gram-positive and gram-negative bacteria.
Route of administration
• It is given in either IM or IV route
• Dose: 250 mg/ml
Side effects
• Nausea
• Vomiting
• Stomach upset
• Numbness/tingling
• Muscle weakness
• Seizure
• Abdominal pain
Adverse effects
• Neurotoxicity
• Nephrotoxicity
• Ototoxicity
Non pharmacological treatment
i. Avoid food that cause acid reflux or heart burn such as spicy food
ii. Don’t lie down or bending after taking meals
iii. Stop smoking
iv. Avoid heavy lifts
v. Avoid doing heavy exercise
vi. Use proper lifting technique
vii. Lose weight
Complications
Hernia is of Reducible, irreducible, obstructed, strangulated or inflamed.
Reducible hernia
In this type the contents are returned but the sac persists. The contents do not re appear necessarily until some external gravity raised in intra -abdominal pressure.
Irreducible hernia
In this the contents do not return to their body cavity. For this the main cause for irreducibility have narrow neck with rigid margin adhesion forms between contents and the sac., These irreducible hernias have greater risk to obstruction and strangulation than reducible hernia. Obstructed hernia: In this intestine contains in lumen become occulated obstruction is at neck of the sac but caused by adhesion within it. If obstruction is at both ends of loop, fluid accumulates in it that blood supply is intact which becomes impended and strangulation. Here the term incarcerated describe irreducible but not strangulated. So, irreducible, obstructed called an incarcerated one [5].
Strangulated hernia
Ten percent of groin hernias present for the first time with strangulation.
Inflamed hernia
• It is inflamed by any process that causes tissues or organ that is normally here herniated.
• Acute appendicitis
• Meckel’s diverticulitis
• Acute salpingitis
• It impossible to inflammable hernia that is strangulated.
• The most common form of hernia occurs are
Inguinal hernia
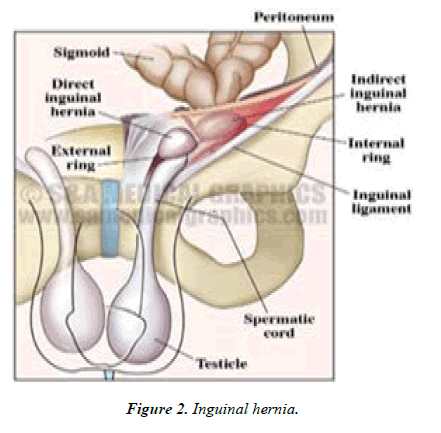
An inguinal hernia occurs when tissue such as part of intestine, protrudes through a week spot in the abdominal muscles. The bulge can be painful, especially when you cough bend over or lift heavy object. Rarely, hernia, do not cause pain. It is not a dangerous but leads to life – threatening complications. These are more common in men than in women and mostly occur on right side (Figure 2).
Classification
In this the inguinal hernias are of like
I. Indirect inguinal hernia
II. Direct inguinal hernia
III. Pantaloons hernia
Indirect inguinal hernia
• This passes through the internal ring lateral
• To interior Epigastric artery and external ring
• Above the pubic crest and tubercle Direct inguinal hernia:
• It occurs at posterior walls of canal medial to inferior Epigastric artery and covered by layers of cord.
Pantaloons hernia
It has both combination of indirect and direct inguinal hernia.
Signs and symptoms
• If you aren’t able to push the hernia in the contents of hernia may be trapped in abdominal wall. An incarcerated hernia may.
• Become strangulated which cuts off blood flow to tissue that’s trapped. The difference between direct and indirect inguinal hernia mentioned in detail in table.
• A strangulated hernia can be life threating if it isn’t treated.
• Nausea, vomiting or both
• Fewer
• Sudden pain that quickly intensifies
• A hernia bulge that turns red, purple or dark
• Inability to more your bowels or pass gas
Causes
• Some inguinal hernias have no apparent causes others occur of
• Increased pressure within abdomen
• A preexisting weak spot in abdominal
• Straining during bowel movements or urination
• Strenuous activity
• Pregnancy
• Chronic coughing or sneezing
Risk factors
1. That contributes to developing an inguinal hernia includes.
2. Being male they are eight times more likely to
3. Develop an inguinal hernia than are women
4. In older people muscles weaker as your age
5. Any family history conditions
6. Chronic cough such as smoking
7. Chronic constipation causes staining during
8. Bowel movements
9. In pregnancy being pregnant can weakness the abdominal muscles and causes increase pressure inside abdomen.
10. Premature birth and low birth weight
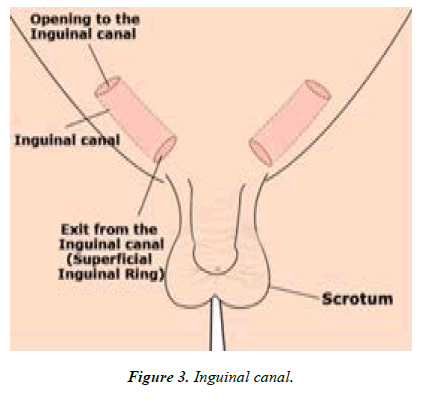
11. Previous inguinal hernia or hernia repair (Figure 3).
Complications
Pressure on surrounding tissue that enlarge over time if not done surgery in men large hernia can extend into scrotum, which cause pain and swelling. Incarcerated hernia that trapped in a weak point in abdominal wall, the contents can obstruct the bowel that leads for severe pain, nausea, vomiting and the inability to have a bowel movement or pass gas. Strangulation, incarcerated hernia can cut of blood flow to part of intestine strangulation can lead to death that affect bowel tissue strangulated hernia is life threatening that requires immediate surgery.
Incisional hernia
Incisional hernia occurs at surgical incisions that are from previous abdominal surgeries. It occurs when the incision of internal organ such as appendix or intestine or other tissues fail to heal properly on time. The people who undergo abdominal surgeries will experience incisional hernia. Mostly after three to six of surgery it will occur in some cases it takes year to occur. Incisional hernia is of post-operative complication and such can be considered in terms pre-operative and postoperative (Table 2).
| Indirect | Direct | |
|---|---|---|
| Patient’s age | Any age usually young | Older |
| Cause | May be congenital | Acquired |
| Bilateral | 20% | 50% |
| Protrusion on coughing | Oblique | Straight |
| Appearance on standing | ||
| Reduction on lying down | Does not reach full size immediately | Reaches full size immediately |
| Descent into scrotum | May not reduces immediately | Reduces immediately |
| Occlusion of internal ring | Common | |
| Strangulation | Rare | |
| Relation to inferior Epigastric vessels | Controls | |
| Not uncommon | Does not control | |
| Lateral | Unusual | |
| Medial |
Table 2. Difference between direct and indirect inguinal hernia.
Pre-operative factors
• Age- tissue of elderly don’t heal than of young
• Malnutrition
• Sepsis
• Anemia- inhibits fibroblast division
• Jaundice- impedes collagen maturation
• Obesity- pre-disposes to wound infection, seroma and hematoma
• Diabetes mellitus – pre disposes to wound infection
• Steroids
• Peritoneal contamination
Operative factors: Types of incisions
• Technique and materials intension in the closure impedes blood supply to the wound badly tied knot can work loose, closure with absorbable suture materials fails to support the abdominal wall for a sufficient time to permit sound union
• Types of operation – It involves bowel or urinary tract are more likely to develop wound infection.
• Drains – A drain passing through the wound results the wound often results in a hernia. Post-operative factors
• Wound infection
• Abdominal distension -Post operative increases in wound, stitches may cut off
• Coughing- It generates wound formation rupture of wound.
• Approximately 40% of incisional hernia occurs by of wound infection (Table 3).
| Patient-related factors | Technical factors related to surgical technique | Disease related factors | Biological factors |
| Age more than 60 years | Wrongly placed incision: lumbar incision, subcostal incision, lower midline incision and large transverse incision | Emergency operations | Nutritional deficiencies |
| Gender: female after caesarean section | Wound has not been approximated | Type of surgery: bowel surgery, abdominal aortic aneurism, stoma | Collagen and metalloproteinase synthesis |
| Smoking | appropriately | closure, operations for peritonitis | |
| Socioeconomic condition: low profile | Low surgical skill to close the abdomen Strength and length of suture used is not appropriate | Re-laparotomy | |
| Occupation: lifting heavy weight Comorbidities: diabetes mellitus, chronic cough, benign hypertrophy of the prostate, stricture of the urethra, chronic constipation, ascites, obstructive jaundice, chronic renal failure and certain connective tissue diseases (Marfan’s syndrome, osteogenesis imperfecta and Ehlers- | Wound infection | ||
| Danlos syndrome) | Long operating time | ||
| Post-organ transplant patient on | Increased blood loss | ||
| immunosuppressive agents/corticosteroids | Damaged control surgery in trauma Open abdomen: in the case of severe septicaemia, chance of abdominal compartment syndrome | ||
| Obesity: (BMI >25 kg/m2) |
Table 3. Risk factors of incisional hernia.
Risk factors
• Patient-related factors
• Technical factors related to surgical technique
• Disease related factors
• Biological factors, detail of these risk factors.
Femoral hernia
A femoral hernia is a bulge in the upper part of the thigh near the groin. They account of 7% of all hernia but they are four times more common in women than in men.
Umbilical hernia
An umbilical hernia is a ventral hernia located at the umbilicus. Classification of abdominal wall hernia defines the umbilical hernia located 3cm above to 3cm below the umbilicus. It is the second most common type of hernia in an adult following inguinal hernia. It accounts for 6%-14% of all abdominal wall hernia in adults [6].
Epigastric hernia
It is a type of an abdominal walls hernia due to a weakness, gap or opening in the muscles or tendon of upper abdominal walls, on the Alba line between the umbilicus and the xiphoid process. It is a quite uncommon and represents 0.5- 5% of all hernia. There is male pre dominance with a male to female ratio of 3:1. It is usually occurs in obese patients.
Literature Review
The role of Prophylactic Cefazolin in the prevention of infection after various types of abdominal wall hernia Repair with Mesh. 19 March 2014 to 13 January 2015. This is a Prospective Randomized control Study over a Period of 5 Years. The Study results has revealed that patients received Prophylactic Cefazolin (Study Group) and the remaining patients didn’t receive any Prophylactic antibiotics (Control Groups). This Study shows that Preoperative Administration of Single dose Cefazolin for Prosthetic hernia Repairs didn’t markedly decrease the risk of wound Infection.
Conducted study on Prophylactic Antibiotic in the mesh repair of inguinal hernia in at Swami Vivekananda Subharti University Meerut from September 2016 to October 2018. This is a Randomized, Prospective, Double.
Blind Study Conducted over a Period of two years. In 100 patients of primary Inguinal hernia given Single dose of prophylactic antibiotics half an hour prior to Mesh Repair Surgery and 50 Patients in Study Group and Routine Antibiotics to remaining 50 in Control group. The Result shows that Prophylactic Antibiotics group reported to have an infection rate of 12% Compared to 10% in Control Group. After 1 month of Surgery Infection was 4% in both groups none of them required Mesh removed. The Use of Prophylactic Antibiotics in our Study was seen to be Effective as routine Preoperative and Postoperative Antibiotics [7].
Conducted Study on Prophylactic antibiotics in open Mesh Repair of Inguinal hernia. Jawaharlal Institute of Postgraduate Medical Education and Research, Puolcherry, A Cochrane Meta-analysis in 2005 Concluded that antibiotics Prophylaxis for Elective Inguinal hernia Repair cannot be firmly recommended or discarded and further studies are needed for the Use of Mesh Repair This is a Prospective, Randomized, Double Blind Study Conducted a period of twenty Months from November 2006 to January 2008. In 450 patients 225 received IV Cefazolin and 225 received a placebo undergoing Primary Inguinal hernia Repair using Polypropylene Mesh.334 Patients completed a follow up period 9 months.172 in Antibiotic group and 162 in Control group. The Overall Infection rate was 87%, Wound Infection in antibiotics group was 7% and 10% in Control group. The result concluded that, shouldn’t recommend the routine use of antibiotic Prophylactic in elective Mesh Repair that rest of Infection occurred between 7th and 12th Postoperative day after discharge.
Conducted Study on to determine the Efficacy of Preoperative Single dose Antibiotics with placebo in patients undergoing Mesh Repair for Inguinal hernia. This randomized controlled trial, was carried in Ayyub teaching Hospital, Abbottabad from January to December 2011. The Study Population included Male patients, above 18 years of age; Patients were divided into 2 groups. Group A people given Single dose of Antibiotic before Inguinal hernia Mesh Repair and
Group B people were given placebo. The Efficacy was accessed in terms of SSI. The results concluded that total 166 cases of inguinal hernia Mesh Repair patients. 83 patients were recruited in each group. In Group A SSI was 7.2% while 92.8% was healthy Scar and In Group B SSI was 15% and 68% had healthy Scars. The difference between 2 groups was Significant, This Study Stays that Antibiotic Prophylaxis is a preferred option for Mesh plasty [8].
Conducted Study on Efficacy of Antibiotics Prophylaxis in preventing SSI in patients Undergoing Lichtenstein’s Hernioplasty at our tertiary care Centre. In the study SSI rates were high both in the antibiotic and placebo group compared to the incidence of Surgical site infections in hernia mesh Repair, reported worldwide, even though the rates of surgical site infections were high in both the antibiotic and control groups, the difference was not known significantly. Based on our results we conclude that routine use prophylactic antibiotic does not decrease the incidence of SSI in mesh hernia repair. The study highlights the need for further research with larger study group and the concentrations of associated risk factors with SSI. This will be of great benefit to check unwarranted administration of antibiotics, which may further lead to a drug reaction and at the same time, will increase the cost of treatment for patient in developing countries like India with limited resources25.
Conducted Study on Antibiotic Prophylaxis in Elective tension free mesh inguinal hernia Repair. Hernia is one of the so-called clean operations many surgeons however use antibiotics especially in the mesh repair, without strong evidence to support this policy we conducted a single center prospective randomized trial with a view to classify this issue on a scientific basis. From January 2000 all patients undergoing elective inguinal hernia repair using a tension free polypropylene mesh technique, provided they fulfilled predetermined criteria, were randomized to have a single dose of Amoxicillin clavulanic acid or placebo in a double minded manner. The main end point was to detect any difference in infectious complicated rates with specific interest to wound infection rates in between the two groups. The two groups were comparable using demographic data. In total 19 cases with infectious complications were detected. Fourteen of these were wound infections. They were 5 cases of wound infections in group A and nine cases of in group B. All wound infections were treated with antibiotics. The wound was open in some cases mesh removal was not required in any of the cases. From the results of this study, it does not appear that antibiotic prophylaxis any benefits to in the elective mesh inguinal hernia Repair.
Randomized, Double Blind, placebo-controlled trial to determine effectiveness of antibiotic prophylaxis for tension free Herniorrhaphy. In recent years, use of prosthetic material for inguinal hernia repair has increased dramatically tension free repair have gained popularity not only for recurrent or complicated hernias, but primary hernias as well. Although routine use of prophylactic antibiotics is not recommended in the Philippines for open non-implant hernia therapy, there is a little direct clinical evidence in which to base recommendations when implantable mesh is used. We conducted a Prospective, Randomized Double Blinded, placebo-controlled trail comparing wound infections rates 360 patients (180 received a prophylactic antibiotic, 180 received a placebo). Undergoing primary inguinal hernia repair electively using polypropylene mesh. Results were assessed using chi-squared. Groups were well matched for all preoperative variables studied, including comorbid conditions. Six patients from the antibiotic group & four from the placebo group failed to follow up after the second week. Superficial surgical site infections (SSI) developed in 3 patients from the antibiotic group & 6 from the placebo group. One from each developed deep surgical site infection. Both patients readmitted & underwent repeated deloridement, which eventually resulted in graph to loss.
Conducted study on prophylactic antibiotic usage in patients undergoing inguinal mech Hernioplasty. To assess the efficacy of antibiotic prophylaxis in this procedure the patients were evaluated for the status of the suture line as well as the Presence of wound infection. This study was undertaken to assess the usefulness of antibiotic prophylaxis in inguinal mesh Hernioplasty in a tertiary care Indian hospital. The prophylactic antibiotic administration in clean contaminated surgeries (colorectal resection). Reduce the infections complications significantly the same cannot be said for clean surgeries such as hernia repairs. This study documented a statistically significant decrease in the overall wound infections when a single dose of antibiotic was used during Liechtenstein Repair.
Conducted study on Survey and evaluation of antibiotic prophylaxis usage in Surgery wards of tertiary level institution before and after the implementation of Clinical guidelines. Standardized recommendations in the guideline were done by the nominal group technique post recommendation evaluation was done to observe the impact in clinical practice. Antibiotic prophylaxis is one component of preventive strategy against surgical site infections that is based on a good surgical technique, strict aspects in operating theatre and control. In patients undergoing surgical procedures under clean and clean –contaminated category, were included the wound was inspected for any evidence of infection starting from 48 hours after surgery, to the day when the patient was discharged. Patients who underwent Laparoscopic procedures were discharged on the 3rd and 4th post-operative day. The rest of the patients were discharged after the suture removal, with clinically no evidence of surgical site infections. The patient who satisfied the superficial Incisional Surgical Site Infection criteria was studied. Cefotaxime was the most commonly used antibiotic for prophylaxis followed by Amoxicillin – clavulanic in the present study. Cefotaxime showed an impressive susceptibility pattern in the present study [9,10].
Aim and Objective
Aim
To evaluate the safety and efficacy of antibiotics in postoperative Hernioplasty and Herniorrhaphy.
Objective
Cephalosporin’s like ceftriaxone, aminoglycosides like amikacin and Beta-lactam antibiotics like piperacillin and tazobactam are these clinical efficacies in reducing surgical site infections. By measuring the wound status of patients by using wound grading during post-operative follow up intervals. To determine social demographic details and categoric the types of hernia in study population.
Need for the study
Prophylactic antibiotics of third generation cephalosporin’s antibiotics example ceftriaxone, cefazolin are active against staphylococcus aureus and staphylococcus epidermidis. These are the causative organisms isolated from hernia repair surgery. So, these make an idea to study the effectiveness of different combinations of post-operative antibiotics like ceftriaxone, cefoperazone, amikacin, piperacillin plus tazobactam in normal and co-morbid conditions.
There is no Indian study to evaluate the safety and efficacy of post-operative antibiotics in Hernioplasty and Herniorrhaphy.
Methodology
Research Methodology
This is a prospective observational study performed and conducted at General surgery department, Government General Hospital, Kurnool.
Plan of study
Materials
A total 73 attended surgical operations in that 58 cases are included in the study which are undergone elective surgeries. In this both males and females are included in this study. The duration of this study was 6 months. The study material was used as patient data collection proforma. Methods:
Individual cases were analysed with regard to following particular
I. Age
II. Sex
III. Date of admission, Date of surgery
IV. Investigations
V. Past history
VI. Comorbid conditions like Diabetes, Hypertension etc.
Operative data
• Type of anesthesia
• Duration of surgery
• Pre-operative preparation
• Post -operative antibiotics
• Drains used or not
Patients were selected on the basis of inclusion and exclusion criteria.
Inclusion criteria
• Patient who is newly diagnosed with hernia.
• Patients of either sex between 18 and 75 years included
in our study.
• Patients representing co-morbid conditions.
• All types of hernia patients are included in the study.
Exclusion criteria:
• Patients age less than 18 years and above 75years.
• Patients with malignancies.
• Patients with previous history of hernia surgery.
Patients with complicated hernias like strangulated and
incarcerated hernia.
Patients taking steroid
Plan of work
1. The data was taken from the patients by collecting data through proforma (patient data collection proforma)
2. All the hernia cases are elective cases.
3. Before the surgery the patients are prepared with preoperative antibiotics and clean the body.
4. During the surgery the patient was given anesthesia and the procedure was done according to the condition.
5. After the completion of surgery patient was put on with antibiotics Injection ceftriaxone 1gm and metronidazole to reduce the post-operative infection rate.
6. Post-operative safety was measured by wound infection grade up to day 5 of post-operative period.
7. Follow up was taken before the discharge.
Statistical analysis
The statistical analysis was carried out to evaluate the effectiveness of different group’s postoperative antibiotics by using ANOVA.
Results
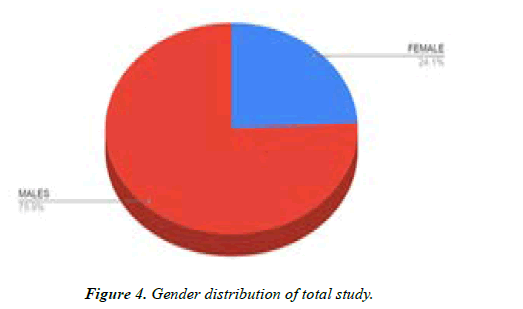
Gender distribution of total study
A Total of 73 patients were presented to the general surgery. But only 58 patients have undergone hernia surgery. Among 58 patients 44 (75.95%) were male and other 14 (24.1%) were female (Table 4, Figure 4).
| Gender | No of patience | Percentage (%) |
|---|---|---|
| Female | 14 | 24.1 |
| Male | 44 | 75.8 |
Table 4. Gender distribution.
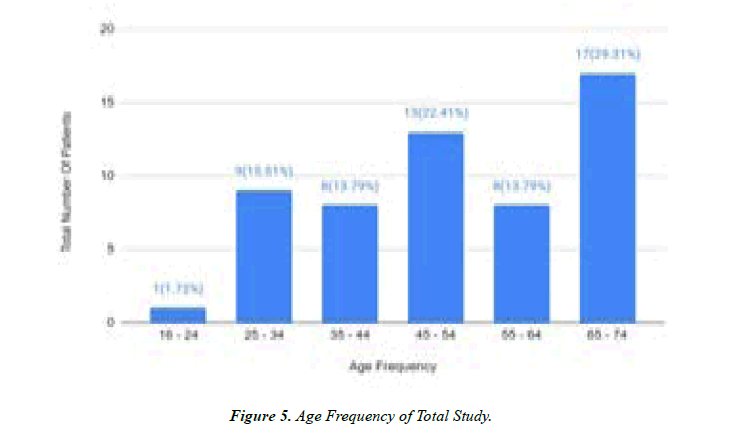
Age distribution of total study
Out of fifty eight patients, 17 (29.3%) patients underwent surgery who is 65-74 years of age (Table 5, Figure 5).
| Age of frequency | No. of Patients | Percentage (%) |
|---|---|---|
| 16-24 | 1 | 1.7 |
| 25-34 | 9 | 15.5 |
| 35-44 | 8 | 13.7 |
| 45-54 | 13 | 22.4 |
| 55-64 | 8 | 13.7 |
| 65-74 | 17 | 29.3 |
Table 5. Age distribution.
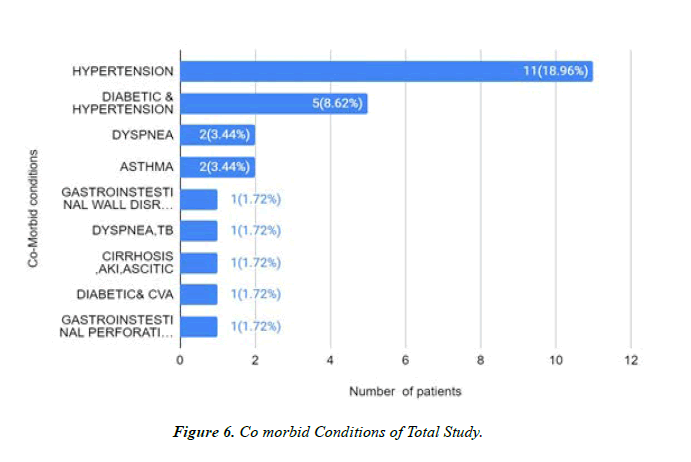
Comorbid conditions of total study
Co morbid Conditions in the considered 58 patients gives the details such as patients with hypertension were more 11 (18.9%) when compared to diabetic and hypertension 5(8.6%), asthma 2(3.4%),dyspnea 2 ( 3.4%), gastrointestinal wall disruption 1 (1.7%), dyspnea, TB 1(1.7%), cirrhosis, AKI, ascites 1 (1.7%) and diabetic and CVA 1(1.7%) (Table 6, Figure 6).
| Comorbid condition | No. of Patients | Percentage (%) |
|---|---|---|
| Hypertension | 11 | 18.9 |
| Diabetic and hypertension | 5 | 8.6 |
| Asthmatic | 2 | 3.4 |
| Dyspnea | 2 | 3.4 |
| Dyspnea, TB | 1 | 1.7 |
| Gastrointestinal wall disruption | 1 | 1.7 |
| Cirrhosis, AKI, Ascites | 1 | 1.7 |
| Diabetic and CVA | 1 | 1.7 |
Table 6. Co-morbid Conditions.
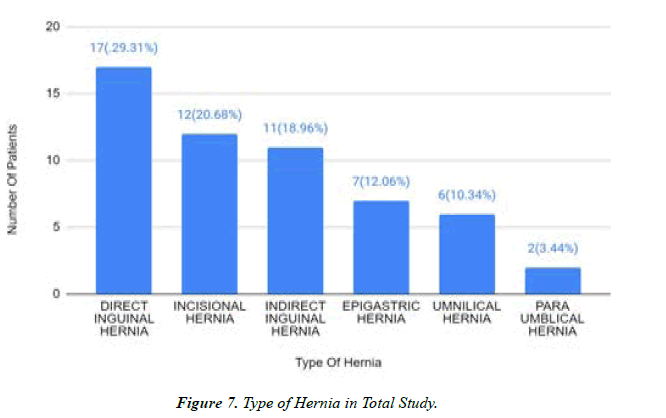
Distribution of type of hernia in total study
The hernia was divided into direct inguinal hernia, indirect inguinal hernia, incisional hernia, Para umbilical hernia, and umbilical hernia and Epigastric hernia. From an aggregate of 58 patients the direct inguinal hernia was more 17 (29.3%) when contrasted with the incisional 12(20.6%), direct inguinal hernia 11(18.9%), Para umbilical hernia 2(3.4%), umbilical hernia 6(10.3%) and Epigastric hernia 7(12%) (Table 7, Figure 7).
| Indirect inguinal Hernia | 11 | 18.9 |
| Epigastric Hernia | 7 | 12 |
| Umbilical Hernia | 6 | 10.3 |
| Para umbilical Hernia | 2 | 3.4 |
Table 7. Distribution of Type of Hernia.
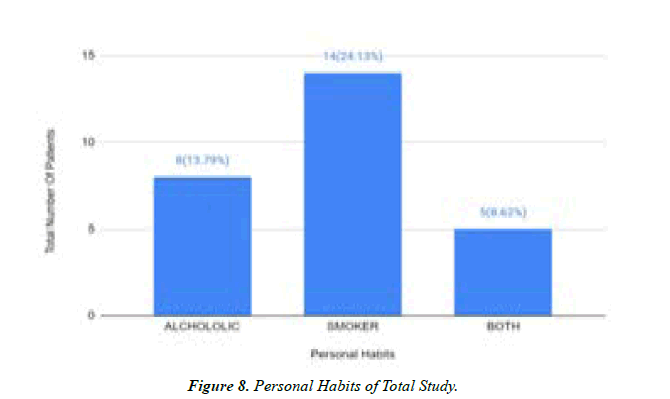
Personal habits of total study
The personal habits were divided into alcoholic, smoker and both. From our case study the smokers were higher when compared with other groups. The populations of alcoholic were 8 (13.7%), smokers were 14(24%) and both were 5(8.6%) (Table 8, Figure 8).
| Personal habits | No. of Patients | Percentage (%) |
|---|---|---|
| Alcoholic | 8 | 13.7 |
| Smoker | 14 | 24 |
| Both | 5 | 8.6 |
Table 8. Personal Habits.
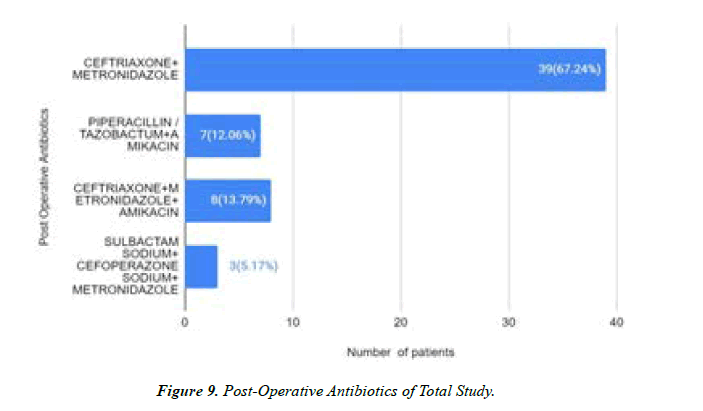
Post-operative antibiotics of total study
The Post-Operative Antibiotics were divided into ceftriaxone + Metronidazole
Group (A): Piperacillin/tazobactam + metronidazole
Group (B): Ceftriaxone + Metronidazole+ amikacin
Group (C): Sulbactam sodium + cefoperazone sodium+ metronidazole
Group (D): On observation of 58 patients, ceftriaxone + Metronidazole were 40 (67.2%) mostly used when compared to Piperacillin/tazobactam + metronidazole are 7 (12%), ceftriaxone + Metronidazole + amikacin were 8 (13.7%) and sulbactam sodium + cefoperazone sodium + metronidazole were 3 (5.1%) respectively (Table 9) (Figure 9).
| Post-operative antibiotics | No. of Patients | Percentage (%) |
|---|---|---|
| Ceftriaxone + Metronidazole | 40 | 67.2 |
| Piperacillin / tazobactam + Metronidazole | 7 | 12 |
| Ceftriaxone + Metronidazole + Amikacin | 8 | 13.7 |
| Sulbactam sodium + cefoperazone sodium + Metronidazole | 3 | 5.1 |
Table 9. Post-Operative Antibiotics.
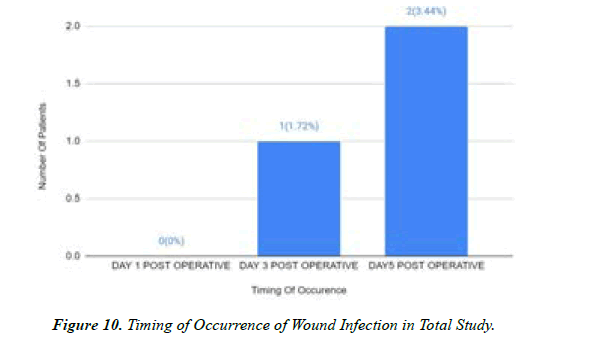
Timing of occurrence of wound infection in total Study
Occurrence of Wound Infection in post operation patients. The patients on day-5 post-operative were more 2 (3.4%), when compared to day-1 post-operative 0 (0%) and day-3 post-operative 1(1.7%) respectively (Table 10) (Figure 10).
| Timing of Occurrence | No. of Patients | Percentage (%) |
|---|---|---|
| Day 1 post-operative | 0 | 0 |
| Day 3Post operative | 1 | 1.7 |
| Day 5 Post-operative | 2 | 3.4 |
Table 10. Timing of Occurrence of Wound Infection.
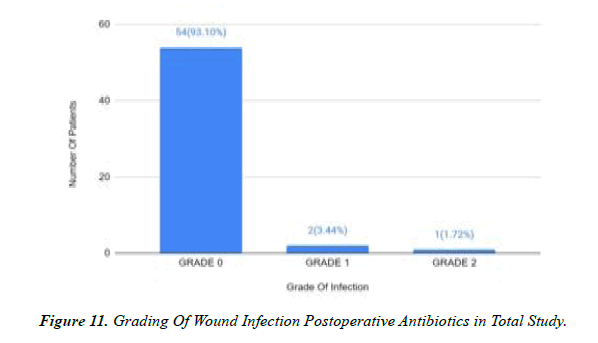
Grading of wound infection postoperative antibiotics in total study
The Grading of Wound Infection of Post-Operative Antibiotics from a total of 58 patients. The patients with grade 0 were 54(93.1%), when compared to grade-1 it is 2 (3.4%) and grade-2 it is 1 (1.7%) respectively (Table 11, Figure 11).
| Grading of Wound Infection | No. of Patients | Percentage (%) |
|---|---|---|
| Grade 0 | 54 | 93.1 |
| Grade 1 | 2 | 3.4 |
| Grade 2 | 1 | 1.7 |
Table 11. Grading of Wound Infection.
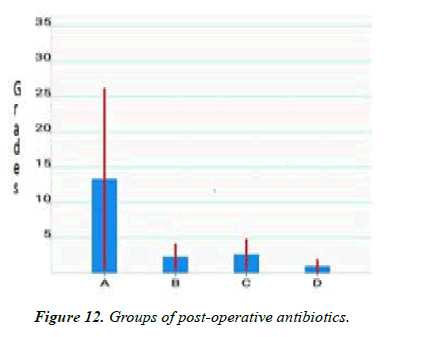
Comparison between Wound Status and Post-Operative Antibiotics
Wound infection which is measured in grades on x axis and post-operative antibiotics in y axis Grade O wound infection rate was more in all groups of post-operative antibiotics. Hence p value is not significant value (p = 0.552264). This indicates the all group are showing equal effectiveness in reducing surgical site infections (Table 12, Figure 12).
| Grades | Group A | Group B | Group C | Group D |
|---|---|---|---|---|
| Grade 0 | 39 | 6 | 7 | 3 |
| Grade 1 | 1 | 1 | 0 | 0 |
| Grade 2 | 0 | 0 | 1 | 0 |
Table 12. Wound Status and Post-Operative Antibiotics.
Discussion
In our study we found the male patients are more 44(75.8%) when compared to female patients 14(24.1%) but in Bakhtiar Vllah et al. Study represents female patients are more, this is because of gender difference in accordance of disease and study population size[11-18]. In present study the majority of patients underwent surgery who is 65 to 74 years of age with a percentage of 29.3% but whereas Alagarsamy GS et al. study represents age frequency of 31 to 40 years with a percentage of (33%) underwent more surgeries. In our study we found that hypertension patients are more with percentage of (18.9%) when compared to patients of diabetic and hypertension 5 (8.6%), asthma 2 (3.4%), dyspnoea 2 (3.4%) gastrointestinal wall disruption 1 (1.7%), dyspnoea, TB 1 (1.7%), diabetic and CVA 1 (1.7%). In the present study we divided the personal habits into smoking, alcoholic and both in which we found that smokers patients are more 14 (24%) compared to alcoholic patients 8 (13.7%) and both (smoking and alcohol) patients are 5 (8.6%), this indicates that who are having smoking are more prone to Hernioplasty.
The present study is a prospective observational study in our study we divided the postoperative antibiotics into 4 groups indicates Group A (ceftriaxone + metronidazole) Group B (piperacillin/tazobactam + metronidazole), Group C (ceftriaxone + metronidazole + amikacin) Group D (sulbactam sodium + cefoperazone sodium + metronidazole), on observation of 58 patients ceftriaxone + metronidazole were given mostly 41 (70.68%) than compared to Group B, Group C, Group D than we observe less SSI but in Perez AR et al [19-22]. study represents by using sulbactam sodium + metronidazole, they includes the antibiotics prophylaxis is of no benefit to patients in inguinal hernia this is because of antibiotic difference in accordance to type of hernia and type of antibiotic prophylaxis used.
In our study, we found that the occurrence of wound infection, SSI in postoperative patients on day 5 postoperative with 2(3.4%) than compared to the day 1 postoperative 0(0%) and day 3 postoperative 1(1.7%), thus we can observe same SSI on day 5 postoperative in Ergul Z et al. study [23]. In the present study the majority of type of hernia is direct inguinal hernia of 17(29.3%). Our results are similar when compared with Alagarsamy GS et al. with type of hernia is direct inguinal hernia (28.9%). In our study grading of wound infection of postoperative of antibiotics from total 58 patients, the patients with grade 0 were 54 (93.1%) which means wound infection is healthy, when compared to Grade 1 it is 2 (3.4%) and Grade 2 it is 1 (.7%), which means most of the patients wound is healthy in hernia patients [24].
Conclusion
In this study the different groups of post-operative antibiotics like ceftriaxone, piperacillin plus tazobactam with ceftriaxone, Amikacin with ceftriaxone and sulbactam plus cefoperazone sodium with ceftriaxone and metronidazole are showing equal effectiveness in reducing surgical site infections in both comorbid and non-morbid conditions. It is concluded that post-operative administration of antibiotics decrease risk of wound infection in study population.
Limitations
The study period is shorter for making the surgical site infection rate.
In our study we did not compare the pre-operative and postoperative effectiveness of antibiotics in hernia population.
References
- Lewis FR, Klingensmith ME. Issues in general surgery residency training—2012. Annals of Surgery. 2012;256(4):553-9.
- Henry MM, Thompson JN. Clinical Surgery E-Book: With Student Consult Online Access. Elsevier Health Sci. 2012.
- Tuma F, Lopez RA, Varacallo M. Anatomy, abdomen and pelvis, inguinal region (inguinal canal). InStat Pearls 2021.
- https://www.webmd.com/digestive-disorders/understanding-hernia-symptoms
- https://www.mayoclinic.org/diseases-conditions/inguinal-hernia/diagnosis-treatment/drc-20351553
- Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. New Eng J Med. 2004;350(18):1819-27.
- Jordan VC, Murphy CS. Endocrine pharmacology of antiestrogens as antitumor agents. Endocrine Rev. 1990;11(4):578-610.
- Tripathi KD. Essentials of medical pharmacology. JP Med Ltd. 2013.
- https://www.rxlist.com/amikin-drug.htm
- Network NN, editor. Neonatal Formulary: Drug Use in Pregnancy and the First Year of Life. John Wiley & Sons. 2008.
- DeNoon DJ, Chang L. WebMD Health News.
- Kumar A, Paswan SS. Incisional Hernia. In Techniques and Innovation in Hernia Surgery. 2019.
- Lucas AG, Jaafar S, Mendez MD. Pediatric Umbilical Hernia. InStat Pearls 2021.
- Grella R, Razzano S, Lamberti R, et al. Combined epigastric hernia repair and mini-abdominoplasty. Case report. Int J Surgery Case Rep. 2015;8:111-3.
- Bahar MM, Nooghabi AJ, Nooghabi MJ, et al. The role of prophylactic cefazolin in the prevention of infection after various types of abdominal wall hernia repair with mesh. Asian J Surgery. 2015;38(3):139-44.
- Maheshwari MK, Singh R, Gupta S. Evaluation of administration of prophylactic antibiotics in mesh repair of inguinal hernia. Int Surgery J. 2019;6(5):1487-94.
- Shankar VG, Srinivasan K, Sistla SC, et al. Prophylactic antibiotics in open mesh repair of inguinal hernia–a randomized controlled trial. Int J Surgery. 2010;8(6):444-7.
- Ullah B, Khan SA, Ahmed S, et al. Efficacy of preoperative single dose antibiotic in patients undergoing mesh repair for inguinal hernia. J Ayub Med College Abbottabad. 2013;25(1-2):103-5.
- Alagarsamy GS, Ramasamy R. The efficacy of antibiotic prophylaxis in preventing SSI (surgical site infection) in patients undergoing Lichenstein’s hernioplasty at our tertiary care centre. Int Surgery J. 2017;4(6):1922-5.
- Tzovaras G, Delikoukos S, Christodoulides G, et al. The role of antibiotic prophylaxis in elective tension‐free mesh inguinal hernia repair: results of a single‐centre prospective randomised trial. Int J Clinical Practice. 2007;61(2):236-9.
- Fugazzotto PA. Shorter implants in clinical practice: rationale and treatment results. Int J Oral & Maxillofacial Implants. 2008;23(3).
- Perez AR, Roxas MF, Hilvano SS. A randomized, double-blind, placebo-controlled trial to determine effectiveness of antibiotic prophylaxis for tension-free mesh herniorrhaphy. J Am College Surgeons. 2005;200(3):393-7.
- Thakur L, Upadhyay S, Peters NJ, et al. Prophylactic antibiotic usage in patients undergoing inguinal mesh hernioplasty—A clinical study. Ind J Surgery. 2010;72(3):240-2.
- Sohil Ahmed K. Survey and evaluation of antibiotic prophylaxis usage in surgery wards of tertiary level institution before and after the implementation of clinical guidelines. Ind J Surgery. 2006;68(3):150-6.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref