Case Report - Journal of Gastroenterology and Digestive Diseases (2016) Volume 1, Issue 2
Esophageal Candidiasis in an Immunocompetent Girl with Chronic Anaemia
- *Corresponding Author:
- Patricia Barros García
Department of Paediatrics, Hospital San Pedro de Alcántara, Avda. Pablo Naranjo s/n. CP-10.003, Cáceres, Spain
Tel: 0034927256200
Fax: 0034927256202
E-mail: pbarrosg@yahoo.es
Received date: June 26, 2016; Accepted date: September 02, 2016; Published date: September 05, 2016
Abstract
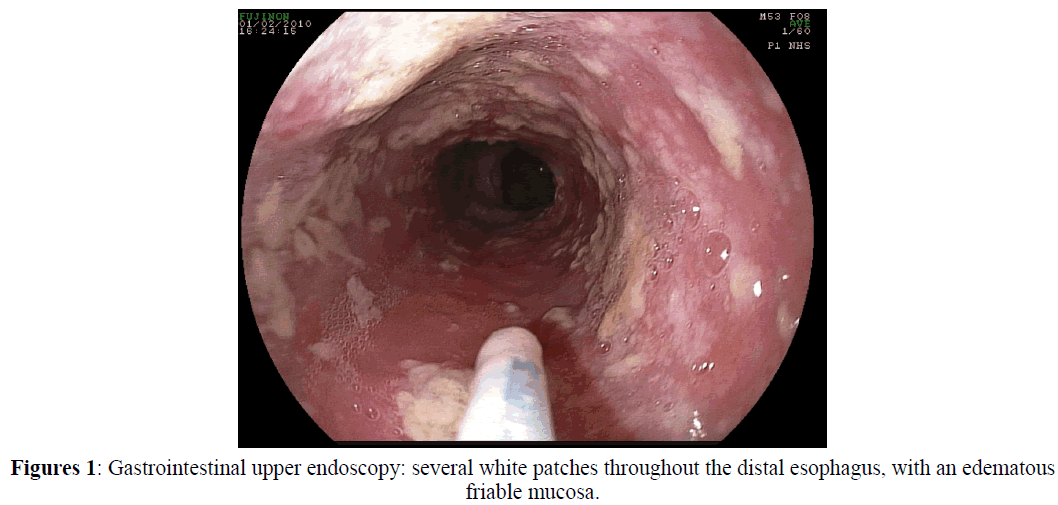
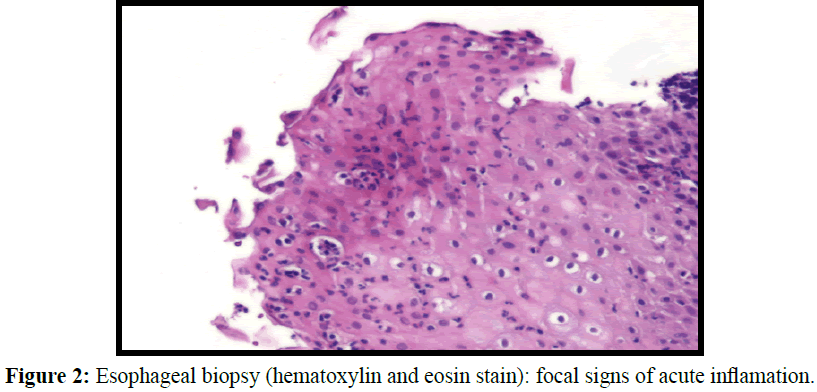
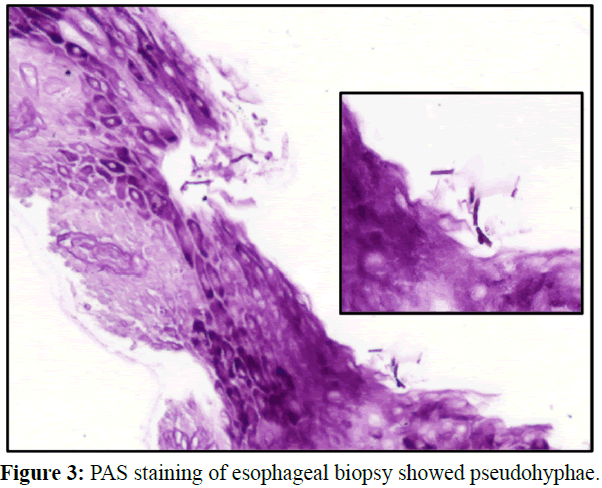
Infection is an uncommon cause of esophagitis among the paediatric population. The main risk factor is immunodeficiency. In children immunocompromised due HIV infection, certain endocrine diseases, and corticosteroid or immunosuppressive therapy, Candida albicans is the most common etiologic agent. The prevalence of Candida esophagitis has increased because of an improvement in survival and management of immunological diseases. Even though it is not frequent in immunocompetent children, there have been reported cases related with risk factors (Chocarro, 2000) such as antibiotic intake (which allow bacterial overgrowth and fungal colonization), proton pump inhibitors (which produce hypochlorhydria allowing oral bacteria to colonize gastric mucosa, and to increase the risk of infectious esophagitis), esophageal obstruction (aperistalsis and stasis helps the fungal overgrowth) and systemic or inhalated corticotherapy (that suppresses lymphocyte and granulocyte function) (Simon, 1997). Candida esophagitis has also been reported in healthy patients, with no evidence of causal mechanism (Alemán, 1996). The most common symptomatology consists in odynophagia, dysphagia and retrosternal chest pain, but epigastralgia, vomiting and gastrointestinal bleeding can also occur. Chronic or acute anaemia could be the sole sign of an asymptomatic presentation (Ortuño Cortés, 1997., Weerasuriya, 2006). The absence of oral candidiasis does not exclude the diagnosis of Candida esophagitis (Mathieson, 1983). The pathophysiology of the infection is complicated. It includes a large number of factors, such as fungal virulence, mucosal integrity and host susceptibility. Esophagoscopy is the most specific and sensitive method of diagnosis. Characteristic endoscopic findings are confluent or isolated white plaques adhered to the mucosa with edema, erythema and friability, with or without ulcers covered by exudate. The diagnostic confirmation is performed by demonstrating the presence of pseudohyfae or by obtaining evidence of tissue invasion on mucosal biopsy (Ahuja, 2016). Fungal culture does not allow differentiation of colonization from infection (Mathieson, 1983). The treatment of choice is fluconazole, but there are new therapeutic options (Ahuja, 2016).
Introduction
Infection is an uncommon cause of esophagitis among the paediatric population. The main risk factor is immunodeficiency. In children immunocompromised due HIV infection, certain endocrine diseases, and corticosteroid or immunosuppressive therapy, Candida albicans is the most common etiologic agent. The prevalence of Candida esophagitis has increased because of an improvement in survival and management of immunological diseases. Even though it is not frequent in immunocompetent children, there have been reported cases related with risk factors (Chocarro, 2000) such as antibiotic intake (which allow bacterial overgrowth and fungal colonization), proton pump inhibitors (which produce hypochlorhydria allowing oral bacteria to colonize gastric mucosa, and to increase the risk of infectious esophagitis), esophageal obstruction (aperistalsis and stasis helps the fungal overgrowth) and systemic or inhalated corticotherapy (that suppresses lymphocyte and granulocyte function) (Simon, 1997). Candida esophagitis has also been reported in healthy patients, with no evidence of causal mechanism (Alemán, 1996). The most common symptomatology consists in odynophagia, dysphagia and retrosternal chest pain, but epigastralgia, vomiting and gastrointestinal bleeding can also occur. Chronic or acute anaemia could be the sole sign of an asymptomatic presentation (Ortuño Cortés, 1997., Weerasuriya, 2006). The absence of oral candidiasis does not exclude the diagnosis of Candida esophagitis (Mathieson, 1983). The pathophysiology of the infection is complicated. It includes a large number of factors, such as fungal virulence, mucosal integrity and host susceptibility. Esophagoscopy is the most specific and sensitive method of diagnosis. Characteristic endoscopic findings are confluent or isolated white plaques adhered to the mucosa with edema, erythema and friability, with or without ulcers covered by exudate. The diagnostic confirmation is performed by demonstrating the presence of pseudohyfae or by obtaining evidence of tissue invasion on mucosal biopsy (Ahuja, 2016). Fungal culture does not allow differentiation of colonization from infection (Mathieson, 1983). The treatment of choice is fluconazole, but there are new therapeutic options (Ahuja, 2016).
Case Report
A 9-years-old afebrile girl was admitted to our hospital for an episode of witnessed loss of consciousness, increased respiratory secretions, facial cyanosis, without tonic-clonic movements, which lasted a few seconds. She was born at 37 weeks’ gestation, through an emergent caesarean section due to severe perinatal asphyxia. At the age of 2 and 18 months, she was admitted to the hospital for pulmonary aspiration. Diagnosed with cerebral palsy (CP), psychomotor retardation, refractory epilepsy and central precocious puberty. Treatments included continuous topiramate, levetiracetam and omeprazole, for several years. The patient had not required antibiotics for an extended period and could be fed orally only with a soft diet, because of an oropahryngeal dysphagia. She had no history of vomiting, dysphagia, abdominal pain, regurgitation or choking. The stools were normal. Physical examination: Weight: 40 kg (97% percentile). Height: 142 cm (90% percentile). T: 36.9°C. HR: 84 bpm. RR: 20 rpm. Sat O2: 92%. BP: 99/53 mmHg. Hemodynamically stable. No signs of respiratory distress. Pale skin and mucous membranes. Well hydrated. Hyperemic oropharynx with white friable plaque, easily bleeding to pressure. Pulmonary auscultation significant for loud coarse upper airway sounds. Spastic tetraparesis. Laboratory studies showed: haemoglobin 6.2 g/dl, haematocrit 21.8%, mean corpuscular volume 52.7 fl, leukocyte count, platelets and coagulation test within normal range. Serum glucose, electrolytes, renal profiles, albumin, total protein, transaminases normal. Serum iron 14 μg/dl, ferritin 4 ng/ml. IgA antiendomisyal and IgA antitransglutaminase test were negatives. Humoral and cellular immunologic study normal. HIV negative. Oropharyngeal exudates culture: C. albicans isolated. Negative stool hemoccult. Chest X-ray normal. Gastrointestinal upper endoscopy: several white patches throughout the distal esophagus, with an edematous friable mucosa (Figure 1). Esophageal biopsy: focal signs of acute inflammation and presence of pseudohyfae. Findings consistent with Candida esophagitis (Figures 2 and 3). 24 hours esophageal-pH-metry: no able to assess due patient intolerance. The patient received a blood transfusion and supplemental iron, with an improvement in haemoglobin. She was started on therapy with fluconazole 5 mg/kg/day for 3 weeks. Repeat esophagoscopy was performed two months after, which demonstrated complete resolution of the lesions. Control blood count was normal after three months on iron therapy.
Discussion
Esophageal candidiasis is a rare entity in the paediatric population. Immunocompromised patients are the main risk group. Here we report the case of an immunocompetent paediatric patient with Candida esophagitis, but with other potential risk factors, like the treatment with proton pump inhibitors for a long period of time (Chocarro, 2000., Hasosah, 2009., Simon, 1997). There are defense mechanisms that maintain normal flora and inhibit fungus colonization such as salivation, esophageal clearance and mucosal integrity. It has been described that proton pump inhibitors produce hypochlorhydria, which induces changes in gastric bacterial flora and allows infection.
The deglutition process requires a high level of coordination between brain and the enteric nervous system. Patients with cerebral palsy usually have deglutition pathology due to motor disorders, which affect salivary flow (Erasmus, 2012). There are limited data regarding salivary production in CP patients, but studies, like (Senner, 2012), describe decreased salivary flow, which could be related to the motor disorders responsible for less frequent deglutition. All of these factors can potentially mitigate the defense mechanisms against Candida colonization. Therefore, there were risk factors in our patient, which could have facilitated Candida infection.
Gastroesophageal reflux due to brain injury occurs in up to 50% in CP patients (Erasmus, 2012). Our patient was on treatment with omeprezole to prevent potential gastroesophageal reflux disease. We were not able to perform a 24 hours esophageal- pH-metry, but histologic results rule out reflux esophagitis. Although the typical clinical manifestation includes digestive symptoms (Ahuja, 2016., Ortuño Cortés, 1997., Weerasuriya, 2006), there are cases reported without digestive complaints, as in our patient, where anaemia was the only indication for the endoscopy. A study realized by (Ortuño Cortés, 1997), described a group of immunocompetent adults with Candida esophagitis. 29% of the patient had anaemia, which was the endoscopy indication.
In Summary
We describe a new case of Candida esophagitis in a paediatric immune competent patient. She had associated risk factors such as proton pump inhibitors intake and cerebral palsy, which could favour fungal colonization and the infection.
References
- Ahuja, N.K., Clarke, J.O. (2016). Evaluation and Management of Infectious Esophagitis in Immunocompromised and Immunocompetent Individuals. Curr Treat Options Gastroenterol, 14(1), 28-38.
- Alemán, C., Alegre, J., Suriñach, J.M., Jufresa, J., Falcó, V., Fernández de, S.T. (1996). Esophageal candidiasis in patients without cellular immunity changes. Report of 7 cases. Rev Clin Esp, 196(6), 375-377.
- Chocarro, M.A., Galindo, T.F., Ruiz, I., González, L.A., Alvarez, N.F., Ochoa Sangrador, C., Martín Arribas, M.I. (2000). Risk factors for esophageal candidiasis. Eur J Clin Microbiol Infect Dis, 19(2), 96-100
- Erasmus, C.E., Van, H.K, Rotteveel, J.J., Willemsen, M.A., Jongerius, P.H. (2012). Clinical practice: swallowing problems in cerebral palsy. Eur J Pediatr, 171(3), 409-414.
- Hasosah, M.Y., Showail, M., Al-Sahafi, A. (2009). Esophageal candidiasis in an immunocompetent girl. World J Pediatr, 5(2), 152-154.
- Mathieson, R., Dutta, S.K. (1983 ) Candida esophagitis. Dig Dis Sci, 28(4), 365-370.
- Ortuño Cortés J.A., Tovar Martínez, A., Ruiz, R.J., García, G.A. (1997). Esophageal candidiasis in HIV-negative patients. Rev Esp Enferm Dig, 89(7), 503-510.
- Senner, J.E., Logemann, J., Zecker, S., Gaebler-Spira, D. (2004). Drooling, saliva production, and swallowing in cerebral palsy. Dev Med Child Neurol, 46(12), 801-806.
- Simon M.R., Houser W.L., Smith, K.A., Long, PM., (1997). Esophageal candidiasis as a complication of inhaled corticosteroids. Ann Allergy Asthma Immunol, 79(4), 333-338.
- Weerasuriya, N., Snape, J. (2006). A study of candida esophagitis in elderly patients attending a district general hospital in the UK. Dis Esophagus, 19(3), 189-192.