Research Article - Allied Journal of Medical Research (2021) COVID-19 in the context of Medical Research
Epidemiology, clinical features and follow-up analysis of 73 cases of COVID-19
Li Yuhong1, Hu Xueyuan2, Pan Hongwei2, Wang Yuanjun1, Lv Ronghua1, Ai Shaozheng1, Jiao Zheng3, Hou Fenlian3, Tan Xiaobin1, Hou Ming1, Haining Fan1, Shen Youlu1*
1Department of Cardiology, Qinghai University Affiliated Hospital, Xining, China
2Department of Cardiology, Wuhan Xinzhou District Traditional Chinese Medicine Hospital, Wuhan, China
3Department of Respiratory, Qinghai University Affiliated Hospital, Xining, China
- Corresponding Author:
- ShenYoulu
Department of Cardiology,
Qinghai University Affiliated Hospital,
Xining, 810001,
China.
E-mail: 524369408@qq.com
Accepted date: December 31, 2020
Citation: Yuhong L, Xueyuan H, Hongwei P et al. Epidemiology, clinical features and follow-up analysis of 73 cases of COVID-19. Allied J Med Res. 2021;5(1): 79-84.
Abstract
Objective: To investigate the epidemiology, clinical features and follow-up analysis after discharge of COVID-19 patients.
Methods: In total, 73 COVID-19 patients (average age: 50.6 ± 10.8 years) were studied.
Results: Of the patients, 72.6% were infected by contact with a COVID-19 patient, 21.9% were infected by family clusters and 41.1% had some underlying disease. Initial symptoms were a fever, dry cough and fatigue. White blood and lymphocyte cell counts were low in 34.2% and 50.7% of patients, respectively. Chest CT imaging showed multiple ground glass and consolidation shadows in one or both lungs. All patients received an antiviral drug. At follow-up, a small number of patients had an intermittent dry cough, low fever, exertional dyspnea, recurrent pharyngeal pain and somnipathy. Nucleic acid and IgM antibody were positively detected in 4.1% and 5.5% of patients, respectively, and chest CT imaging showed multiple fibrous cords and mild fibrosis in both lungs in 4.1% of patients.
Conclusion: Individuals are susceptible to the novel coronavirus. Contact and familial clustering are the major infection routes. No specific changes in laboratory tests were evident but a reduction in lymphocyte count was common, and chest CT imaging revealed specific manifestations. Some discharged patients continued to display symptoms causing discomfort.
Keywords
Wuhan, COVID-19, Epidemiology, Clinical condition, Follow-up
Introduction
The novel coronavirus disease that emerged in 2019 was named “COVID-19” by the World Health Organization, and the International Committee on Taxonomy of Viruses officially named this novel coronavirus “severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2)” [1]. The disease has been included as an acute respiratory infection under the Law on the Prevention and Control of Infectious Diseases of the PR China. It is classified as a Category B infectious substance and is managed as a Category-A infectious disease [2]. As COVID-19 is a novel pneumonia caused by coronavirus, there is no conclusive clinical evidence or effective therapeutic drugs available at this time. Follow-up data after the discharge of patients are also lacking. Therefore, this study collected clinical data from 73 COVID-19 patients hospitalized in the Hospital of Traditional Chinese Medicine of Wuhan XinZhou District, and analyzed their epidemiology, clinical manifestations, laboratory tests, imaging features and follow-up after discharge, to provide a reference for the diagnosis, treatment, prevention and control of COVID-19.
Materials and Methods
Clinical data
Data from COVID-19 patients hospitalized at the Hospital of Traditional Chinese Medicine of Wuhan XinZhou District, Hubei Province, from January 29, 2020, to March 17, 2020, were retrospectively analyzed. A total of 73 cases were studied, including 35 males and 38 females, and 58 mild and 15 severe cases.
Methods
Diagnosis and clinical typing: Diagnosis was carried out based on the Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7) developed by the General Office of the National Health and Health Commission. In total, 73 patients who tested positive by real-time RT-PCR from a throat swab were included.
Nucleic acid test: RT-PCR was performed using test kits provided by Shanghai Jienuo Biological Technology Co. Ltd. The results were interpreted using a cut-off value of 40, and a Ct value <37 was regarded as positive, whereas a Ct value >40 was regarded as negative. For values between 37 and 40, the test was repeated.
Laboratory examination: Peripheral blood was collected on admission for routine blood tests. The following factors were analyzed: procalcitonin (PCT), C-Reactive Protein (CRP), the Erythrocyte Sedimentation Rate (ESR), myocardial injury biomarkers, and coagulation function and biochemistry. The normal ranges of all indexes were based on the laboratory test standards for the Hospital of Traditional Chinese Medicine of Wuhan Xin Zhou District.
Discharge criteria: Patients were discharged if the following criteria were met: (1) body temperature returned to normal for more than 3 days and respiratory symptoms improved significantly; (2) lung imaging showed significant inflammatory absorption; (3) two consecutive negative SARS-CoV-2 nucleic acid tests with a sampling interval of at least 1 day.
Observation indexes: The following indexes were observed and recorded for each of the patients: clinical manifestations, laboratory tests, imaging data, treatment and outcomes, and follow-up data after discharge.
Statistical methods
Countable data are presented as the number of cases (%) and measurable data are presented as the mean ± standard deviation (χ ± s).
Results
General characteristics of the patients
A total of 73 COVID-19 patients who had been hospitalized and discharged from the Hospital of Traditional Chinese Medicine of Wuhan Xin Zhou District, Hubei Province, were included in this study. Of these patients, 35 (46.7%) were male and 38 (53.3%) were female. Patients were aged 27-77 years, with a mean age of 50.6 ± 10.8 years; 37 patients (50.7%) were aged 20 to 49 years and 36 (49.3%) were aged ≥ 50 years. The average body mass index was 20.1 ± 2.8 kg/cm2. The time from contact to infection ranged from 3 to 14 days, with an average time of 6.9 ± 3.3 days. The transcutaneous oxygen saturation level after admission was 95.3 ± 2.3%, with 15 patients (13.7%) showing less than 93%.
Epidemiology
All of the 73 patients were residents of Xinzhou District, Wuhan, Hubei Province. Of these patients, 16 (21.9%) were infected by a family cluster; 53 (72.6%) had a contact history with a COVID-19 patient, of whom 6 (8.2%) were in the service industry, including 1 barber, 1 jewelry processor, 2 dentists and 2 drivers (1 taxi driver and 1 public service driver); 3 (4.1%) were nosocomial infections contracted during visits for other reasons; and the source of infection for the other 4 cases (5.5%) was unclear.
Clinical features
History of basic diseases: Of the 73 patients, 43 (58.9%) had no other disease, 6 (8.2%) had hypertension, 7 (9.5%) had diabetes, 4 (5.5%) had hypertension combined with diabetes, 1 (1.3%) had hypertension combined with COPD, 2 (2.7%) had COPD, 1 (1.3%) had hypertension combined with coronary artery disease, 1 (1.3%) had hypothyroidism, 5 (6.8%) were carriers of chronic viral hepatitis B, 1 had a metal sleeve implanted after tracheotomy for laryngeal cancer, 1 had a radius fracture, and 1 had chronic renal failure.
Clinical symptoms: The predominant symptom among the 73 patients was a fever. All of the patients experienced a moderate to high fever in the early stages of the disease of up to 40.9°C. The next most common symptom was a dry cough and fatigue. Rare symptoms included coughing with sputum, myalgia, dizziness and diarrhea. In fact, diarrhea was the first symptom in two cases.
Laboratory examination: After admission, routine blood tests showed decreased white blood cell counts (<4 × 109/L) in 25 patients (34.2%), decreased lymphocyte counts (<1.26 × 109/L) in 37 (50.7%), thrombocytopenia (<100 × 109/L) in 5 (6.82%) and thrombocytosis in 9 (13.1%; >300 × 109/L). The ESR, CRP and PCT results for the 73 patients showed elevated ESR in 97.2% of cases (71/73), elevated CRP in 27.4% of cases (20/73) and elevated PCT in 15.1% of cases (11/73).
Biochemical analysis showed hypoalbuminemia in 25 (34.2%) of the 73 patients, hypoglobulinemia in 24 (32.9%), elevated alanine aminotransferase in 22 (30.1%), elevated oxaline aminotransferase in 14 (19.2%), elevated total bilirubin in 1 (1.4%), elevated indirect bilirubin in 1 (1.4%), elevated blood urea nitrogen in 1 (1.4%), azotemia in 3 (4.1%; creatinine >106 μmol/L), elevated uric acid in 19 (26%), elevated homocysteine in 7 (9.6%), elevated cholesterol in 5 (6.8%) and elevated triglycerides in 17 (23.2%).
Myocardial injury biomarkers were tested in all patients. Elevated creatine kinase levels were evident in 12 patients (16.4%), elevated creatine kinase isoforms were present in 2 (2.7%), elevated troponin I was present in 5 (6.8%), elevated myoglobin was present in 6 (8.2%), elevated BNP was present in 8 (10.9%) and elevated lactate dehydrogenase was present in 27 (40%). Coagulation showed increased INR levels in 22 patients (30.1%) and D-dimer ≥ 0.5 μg/mL in 11 (15.1%).
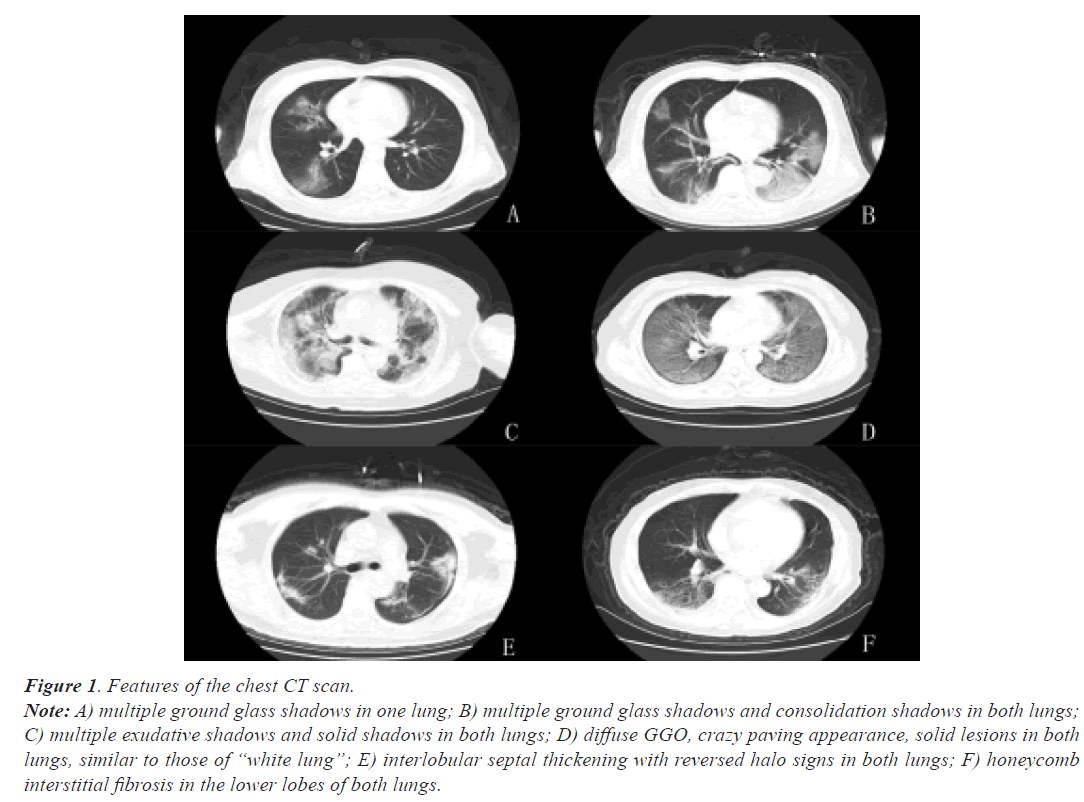
Imaging examination: All patients underwent a chest CT examination, in which 22 (30.1%) showed early lesions, 45 (60%) were in the progressive stage, 15 (20%) showed severe lesions and 16 (21.3%) were in the recovery stage; 3 (4.1%) had multiple ground glass shadows and consolidation shadows in one lung, 47 (63%) had multiple ground glass shadows and consolidation shadows in both lungs, of which 3 had diffuse distribution in both lungs; 11 (15.1%) had multiple lung consolidation and fibrous cords, with 1 patient having pleural effusion, and 11 (15.1%) had multiple interlobular septal thickening or cellular interstitial fibrosis in both lungs. The results are shown in Figure 1.
Figure 1: Features of the chest CT scan.
Note: A) multiple ground glass shadows in one lung; B) multiple ground glass shadows and consolidation shadows in both lungs;
C) multiple exudative shadows and solid shadows in both lungs; D) diffuse GGO, crazy paving appearance, solid lesions in both
lungs, similar to those of “white lung”; E) interlobular septal thickening with reversed halo signs in both lungs; F) honeycomb
interstitial fibrosis in the lower lobes of both lungs.
Treatment and outcomes: During hospitalization, all patients, with the exception of those with normal SpO2 levels, were given high-flow oxygen (oxygen flow rate of 4 L/min) through a nasal catheter. All patients were treated with Lianhuaqingwen, a traditional Chinese medicine, 53 (72.6%) were treated with one or two types of antiviral treatment including oseltamivir, arbidol and ribavirin; 9 (12.3%) were treated with empirical anti-infection such as cefprozil, levofloxacin, and moxifloxacin, 16 (21.9%) were treated with glucocorticoid during hospitalization, and 4 (12.9%) were treated with intravenous infusion of gammaglobulin. All 73 patients met the discharge criteria specified in the Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7), with a median length of stay of 18 days.
Follow-up after discharge: All 73 patients were reexamined and followed up during the second, fourth and eighth weeks after discharge. After discharge, 11 patients (15.1%) had an intermittent dry cough, 6 (8.2%) had a low-grade fever, 18 (24.6%) had exertional dyspnea, 16 (21.9%) had recurrent pharyngeal pain, 19 (26%) had somnipathy, 3 (4.1%) had a positive nucleic acid test, 4 (5.5%) had a positive IgM antibody test, 70 (95.9%) had a positive IgG antibody test and 3 (4.1%) had multiple fibrous cords and mild fibrosis in both lungs as observed by chest CT imaging (Table 1).
| Follow-up | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Item | Cough | Fever | Exertional dyspnea | Pharyngeal pain | Somnipathy | Re-positive nucleic acid | Positive IgM | Positive IgG | Insignificant CT absorption |
| Number of cases | 11 | 6 | 18 | 16 | 19 | 3 | 4 | 70 | 3 |
| (%) | 15.1 | 8.2 | 24.6 | 21.9 | 26 | 4.1 | 5.5 | 95.9 | 4.1 |
Table 1: Follow-up data of patients after discharge.
Discussion
The patients in this study were all local residents of Xinzhou District, Wuhan, with an average age of 50.6 ± 10.8 years. The proportion of young people was higher than that of middle-aged and older people, which was inconsistent with previous reports. This discrepancy might be due to the small number of cases in this study, and the fact that the younger and middle-aged people were more cooperative than the older people with the outpatient follow-up, recording of data and registration. The mean time from contact to infection was 6.9 ± 3.3 days, which was consistent with the guidelines and previous reports [3]. Transcutaneous oxygen saturation levels were 95.3% ± 2.3%, with 15 severe cases (20%) having an oxygen saturation level of less than 93%.
The primary source of transmission of COVID-19 is from contact with SARS-CoV-2-infected patients, and the routes of transmission include respiratory droplets and close contact transmission, with the population being generally susceptible [4]. All patients in this study reported the onset of disease before February 20, 2020, and the transmission route was mainly airborne or contact transmission. More than 20% of patients were clustered in households, 72.6% of patients had a history of contact with COVID-19 patients (some of whom were infected at work), and 3 cases were nosocomial infections. None of the patients had contact history with Huanan (South China) Seafood Market.
In this study, we found that patients with basic diseases were more susceptible to SARS-CoV-2 infection. The main basic diseases included hypertension, diabetes, coronary heart disease, COPD, chronic liver disease, chronic kidney disease, resection of a malignant tumor and hypothyroidism. This indicated that patients with the above basic diseases are at high risk of severe COVID-19. All 15 patients with severe COVID-19 in our study also had basic diseases such as diabetes and hypertension. SARS-CoV-2 invades host cells through the binding of S protein on surface spines and angiotensin-converting enzyme 2 receptor (ACE2) on the cell membrane surface [5]. ACE2 is widely expressed in various tissues of the body. In hypertension and diabetes patients, the functions of vascular endothelial cells are disordered, vascular permeability is increased, and inflammatory factors leak into the alveoli, resulting in infection [6,7].
The main symptom reported among the 73 patients was fever, with patients showing a moderate to high fever in the early stage of the disease, and a maximum temperature of 40.9 C. The next most common symptom was a dry cough and fatigue; coughing with sputum, myalgia, dizziness and diarrhea were observed in some cases, which was consistent with the guidelines. Few patients showed upper respiratory symptoms such as a runny nose and nasal congestion, which indicates that the target cells of SARS-CoV-2 were mainly in the lower respiratory tract [8]. In two patients, diarrhea was the first symptom, which is considered to be related to the high expression of ACE2 in human small intestinal epithelial cells [9].
Most COVID-19 patients have normal or reduced levels of peripheral blood leukocytes, and a decreased lymphocyte count is common, which progressively decreases with disease exacerbation [10]. In this study, 34.2% of patients had a decreased white blood cell count and 50.7% had a decreased lymphocyte count. The decrease in the white blood cell and lymphocyte counts reflects the fact that SARS-CoV-2 mainly attacks lymphocytes in the body, causing a decrease in CD4+ T lymphocytes, which leads to decreased immune function and thereby infection, and in severe cases, severe pneumonia [8].In this study, 97.2% of patients showed elevated levels of ESR, 27.4% of patients showed elevated CRP and 15.1% of patients showed elevated PCT levels, which may be because ESR can increase rapidly after viral infection, while CRP and PCT show no obvious response to viral infection [11]. Therefore, the joint detection of ESR, PCT and CRP may be helpful for the diagnosis of COVID-19. The present study found that 6.82% of patients had thrombocytopenia and 13.1% had thrombocytosis. It has been reported that in severe cases, primarily after viral infection, the virus can directly destroy platelets, and the production of anti-platelet antibodies further destroys platelets; consequently, the coagulation system is activated and converts prothrombin to thrombin and rapidly consuming platelets [12]. The infection increases the platelet count; therefore, the inflammatory state of COVID-19 may be an acute temporal response and viral infection may be associated with the activation of platelets by inflammatory mediators [13].
This study suggests that hypoalbuminemia, elevated blood uric acid and hyperlipidemia may also be high risk factors for COVID-19, and the presence of elevated levels of alanine aminotransferase and azotemia suggest that this novel coronavirus can damage the liver and kidneys after invasion [14]. Considering that SARS-CoV-2 mainly affects the immune system, hypoglobulinemia leads to decreased immune function and decreased globulin [15]. Myocardial injury biomarkers showed varying degrees of elevated cardiac enzymes, thus the significantly higher incidence of myocardial injury during SARS-CoV-2 infection may be related to direct myocardial cell damage caused by the virus through ACE2 receptor infection [16]. Coagulation function showed an increase of 30.1% in INR and 15.1% in D-dimer; in the early stages of COVID-19 infection, some severe and critically-ill patients progressed rapidly to acute respiratory distress syndrome, coagulation disorders, and even death during disease progression.
Based on the chest CT imaging features of COVID-19 patients, the disease can be divided into four stages: early stage, progression, severe stage and recovery stage [17]. In this study, chest CT examination of the 73 patients showed 30.1% to be at the early stage, 60% at the progression stage, 20% at the severe stage and 21.3% at the recovery stage, which is consistent with the pathological changes in viral pneumonia, in which both the interstitium and lung parenchyma are involved. Autopsy found that the lungs of COVID-19 patients showed obvious damage, with a patchy appearance visible by eye showing gray/white foci and dark red hemorrhages, and a soft texture to the touch, which were consistent with the imaging changes [13].
In this study, with the exception of patients with normal SpO2 levels, all patients were treated with a nasal catheter or high-flow oxygen. All 73 patients were treated with traditional Chinese antiviral therapy, and 21.9% were treated with glucocorticoids during hospitalization. All patients were discharged from the hospital with active antiviral, anti-inflammatory, empirical anti-infection, immune modulation and symptomatic support therapy. The time from contact to infection for COVID-19 has been reported to be approximately 4.6-5.2 days [18,19], whereas the results of the present study showed a time of 6.9 ± 3.3 days, which was longer than that reported previously. The median hospital stay in the current study was 18 days. These results indicated that the shorter the time from contact to infection, the shorter the average duration of hospitalization, and the more favorable the disease progression and epidemic control.
After discharge, all patients were followed up and ongoing symptoms included an intermittent dry cough, a recurrent low fever, exertional dyspnea, recurrent pharyngeal pain and somnipathy, along with positive tests for nucleic acid, IgM and IgG antibodies, and multiple fibrous cords and mild fibrosis observable by chest CT imaging of both lungs. As SARS-CoV-2 mainly caused alveolar exudation, alveolar epithelial cells were obviously damaged; however, after treatment, these symptoms were alleviated. Lung imaging showed obvious absorption of exudation and solid lesions, but the complete repair of alveolar epithelial cells took longer, in some cases more than 3 months, so symptoms such as a dry cough and dyspnea persisted [20]. Two patients discharged from hospital tested positive for nucleic acid after 2 weeks, and the possibility of two false negative nucleic acid tests before discharge was considered. One patient gave a positive nucleic acid test 8 weeks after discharge but had no particular symptoms and when re-tested a negative result was obtained. Falsepositive and false-negative results are possible for nucleic acid tests, and the patients should be repeatedly tested after diagnosis. In patients with mild disease and a short hospital stay, IgM antibodies were still present 2 weeks after discharge, but further follow-up showed negative results after an interval of 2 weeks. This result may be related to the infection time of the virus, with all patients testing negative for IgM antibodies and positive for IgG antibodies after an interval of 2 months from the initial infection [21]. Multiple fibrous cords and mild fibrosis in both lungs are manifestations of viral pneumonia, and antifibrotic therapy should be given if necessary. The high mental and psychological stress experienced by COVID-19 patients severely affects their sleep and can even cause depression [22]. Sleep quality was significantly improved in patients with sleep disorders following the assistance of psychiatrists at a later stage.
Conclusion
The benefits of this study are that complete data from the initial out-of-hospital infection to hospitalization and follow-up within 8 weeks after discharge were obtained and analyzed for COVID-19 patients. These data reflect the characteristics of COVID-19 cases in a comprehensive manner, thus providing a more complete and detailed analysis of the late complications of COVID-19. The implications of these findings may prove valuable in supporting clinical diagnosis and treatment strategies. One limitation of this study is that it is a single-center study with a small sample size, which may not fully represent all of the characteristics of COVID-19. Furthermore, this study was conducted in a grade-A secondary hospital, thus the detection of inflammatory factors could not be performed and high-resolution chest CT imaging was not available. Further studies should focus on the pathogenesis and early diagnosis of COVID-19, which will aid the control and treatment of this infectious disease.
Acknowledgments
We thank Kate Fox, DPhil, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
References
- Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-an update on the status. Mil Med Res. 2020;7:11.
- Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020.
- National Health Commission of the PRC, National Administration of Traditional Chinese Medicine. Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7) 2020.
- Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in china. N Engl J Med. 2020:2002032.
- Wan Y, Shang J, Graham R, et al. Receptor recognition by the novel coronavirus from wuhan: an analysis based on decade-long structural studies of sars coronavirus. J Virol. 2020;94:00127-20.
- Wu CM, Hu XL, song JX, et al. Heart injury signs are associated with higher and earlier mortality in coronavirus disease 2019 (COVID-19). Med Rxiv. 2020.
- Chai XQ, Hu LF, Zhang Y, et al. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019 nCoV infection. Bio Rxiv. 2020.
- Huang C, Wang Y, LI X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-06.
- Chen HY, Xuan BQ, Yan YQ, et al. Profiling ACE2 expression in colon tissue of healthy adults and colorectal cancer patients by single-cell transcriptome analysis. Med Rxiv. 2020.
- Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565-74.
- Mehrjardi M, Khkouee S, Pourabdollah M. Radio-pathological correlation of organizing pneumonia (OP): A pictorial review. Br J Radiol. 2017;90:20160723.
- Xu JL. Clinical study on severe infection related thrombocytopenia. Renowned Doctor, 2020:118.
- Zheng SY, Xiao QY, Xie Xh, et al. Association between secondary thrombocytosis and viral respiratory tract infections in children. Sci Rep. 2016;6:22964.
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, china. JAMA. 2020;323:1061-69.
- Xu X, Chn P, Wang J, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63:457-60.
- Pan F, Ye T, Sun P, et al. Time course of lung changes at chest ct during recovery from coronavirus disease 2019 (COVID-19). Radiol. 2020;295:715-21.
- Liu Q, Wang R, Qu G, et al. Gross examination report of a COVID-19 death autopsy. J Foren Med. 2020;36:1-3.
- Zhang MQ, Wang XH, An YL, et al. Clinical features of 2019 novel coronavirus pneumonia in the early stage from a fever clinic in Beijing. Chinese J Tubercul Resp Dise. 2020;43.
- LiQ, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199-07.
- Lee N, Hui D, Wu A, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1986-94.
- Nolan T, Hands RE, Bustin SA. Quantification of mRNA using real-time RT-PCR. Nat Protoc. 2006;1:1559-82.
- Deng YF. Professor of Psychiatry: Three ways to address psychological distress in people affected by COVID-19. Workmates. 2020:17.