Case Report - Current Pediatric Research (2018) Volume 22, Issue 3
Environmental factors predisposing to type 1 diabetes mellitus in children: A descriptive study of various pediatric endocrine clinics in Jeddah, Saudi Arabia.
Rayan Ali I Alghamdi, Abdulmoein Eid Al-Agha*, Abdulrhman Mohammad Banasser, Hesham Fouad Barradah, Saleh Jameel Almatrafi, Ibrahim Musnef K Alyazidi, Abdullah Sabti S AlmoeirfiDepartment of Pediatrics, King Abdul-Aziz University, Jeddah, Saudi Arabia
- Corresponding Author:
- Abdulmoein Eid Al-Agha
Professor, Pediatric Endocrinology, King Abdulaziz University Hospital
Pediatric Department, POBox 80215, Jeddah 21589, Saudi Arabia
Tel: + 966 2 640 3841
Fax: + 966 2 6408353
E-mail: aagha@kau.edu.sa
Accepted date: August 14, 2018
Abstract
Background: There is increasing incidence of Type 1 Diabetes Mellitus (T1DM), an autoimmune disease that destroys pancreatic beta cells and is caused by multiple environmental factors. This increasing incidence has been associated with different factors. We aimed to investigate the relationship between environmental factors, such as vitamin D deficiency, socioeconomic status, maternal age, low birth weight, mode of delivery, and breastfeeding; and T1DM. In addition, we critically discussed environmental factors promoting the progression to T1DM. Methods: We analyzed data of 250 children and adolescents aged<18 years who were selected through a random sampling technique. Descriptive data were collected from various ambulatory pediatric endocrine clinics in Jeddah city by reviewing both the medical records of patients and the phoenix system. Results: The 250 patients included 125 boys and 125 girls with T1DM. Evaluation of environmental factors revealed that 111 (44.4%) patients had low vitamin D levels, 106 (42.4%) had good income, 140 (56.7%) had maternal age>30 years at delivery, 190 (76%) had normal birth weight, 173 (69.2%) were delivered through vaginal birth, 72 of 117 patients were breast and bottle fed, and 72 of 142 patients were fed for 1-2 years after birth. Conclusions: There was a significant association between environmental factors and increased risk of T1DM. The most common environmental factors that increased the risk of T1DM were maternal age>30 years and low vitamin D levels in the infant as well as good or average socioeconomic status.
Keywords
Environmental factor, Type 1 diabetes mellitus, Pediatric endocrine clinic.
Introduction
Type 1 Diabetes Mellitus (T1DM) is an autoimmune disease that triggers the destruction of pancreatic beta cells, and is caused by several environmental factors [1]. The incidence of T1DM has almost doubled from 2.8% to 4.0% per year worldwide [2]. Therefore, we examined a previously proposed hypothesis, to explain the drastic increase in the incidence of T1DM. Several studies have investigated the relationship between environmental factors and the risk of childhood-onset T1DM; some studies have demonstrated a weak relationship, while others have confirmed a significant relationship [3]. In recent years, the increasing incidence of T1DM has been associated with various factors [4]. The aim of our study was to investigate the relationship between environmental factors, such as vitamin D deficiency, as well as socioeconomic status, maternal age, low birth weight, mode of delivery, and breastfeeding, and T1DM. In addition, we discussed environmental factors that are promoting the progression to T1DM.
Materials and Methods
Study design
This is a descriptive study conducted at King Abdul- Aziz University Hospital, with data collected from diabetes mellitus clinics in Jeddah, Saudi Arabia, from July to October 2017.
Study population
The study population comprised 250 children and adolescents<18 years of age who were selected through a random sampling technique. Individuals>18 years were excluded from this study. Participants with type 2 diabetes mellitus and those who underwent pancreatectomy were excluded from the study.
Data collection
Data were collected from both the medical records and the phoenix medical system. These medical records were from the Department of Pediatrics, King Abdul-Aziz University, Jeddah, Saudi Arabia. All demographic data, including age, sex, birth weight, mode of delivery, and type of feeding in children diagnosed with T1DM, were collected.
Ethical considerations
This study was approved by the Institutional Review Board of King Abdul-Aziz Hospital. All information of the patients was kept confidential.
Statistical analysis
Data were entered, coded, cleaned, and analyzed using the statistical package for social science version 22 (IBM SPSS).
Results
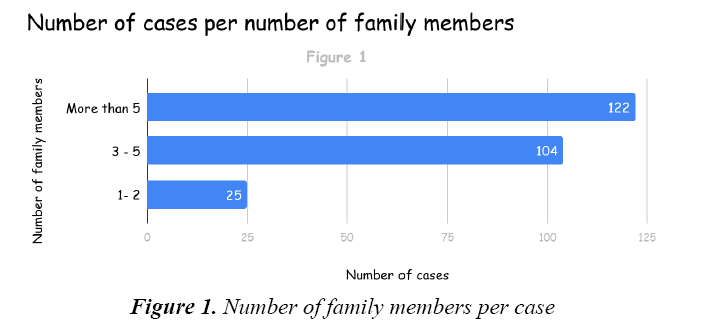
A total of 250 T1DM cases were reviewed from July to September 2017. Among these, 204 cases (81.6%) were Saudis and 46 (18.4%) were non-Saudis. Furthermore, 142 cases (56.8%) did not have consanguineous parents, while 108 (43.2%) had consanguineous parents. Income for assessing the socioeconomic status was as follows: 40 cases (16%) had low income, 104 cases (41.6%) had average income, and 106 cases (42.4%) had good income. The number of family members was assessed and we noted that 25 cases (10%) had 1-2 family members, 103 cases (41.2%) had 3-5 family members, and 122 cases (48.8%) had>5 family members (Figure 1). Maternal age at delivery was also evaluated (Table 1). At the time of delivery of the study participants (children and adolescents), 7 mothers (2.8%) were<20-years-old, 100 mothers (40.5%) were aged between 20-29 years, 123 mothers (49.8%) were aged between 30-39 years, and 17 mothers (6.9%) were ≥ 40-years-old. Birth weight was examined and we observed that 34 cases (13.6%) had low birth weight, 190 cases (76%) had normal birth weight, and 26 cases (10.4%) had large birth weight. Mode of delivery was assessed and 173 mothers (69.2%) had vaginal birth and 77 (30.8%) had cesarean section.
| Maternal Age | Number of Cases |
|---|---|
| <20 years | 7 (2.8%) |
| 20-29 years | 100 (40.5) |
| 30-39 years | 123 (49.8%) |
| ≥ 40 years | 17 (6.9%) |
Table 1: Maternal age distribution
The different feeding types are presented in Table 2. Seventy-nine cases (31.6%) were breastfed, 54 (21.6%) were bottle fed and 117 (46.8%) were breast- and bottle fed. For feeding duration, 28 cases (11.2%) were fed for <6 months, 67 cases (26.8%) were fed for 6 months to 1 year, 142 cases (56.8%) were fed for 1-2 years, and 13 cases (5.2%) were fed for>2 years. Following the assessment of vitamin D levels, we noted that 139 cases (55.6%) of vitamin D levels were within normal, while 111 cases (44.4%) had low vitamin D levels.
| Feeding duration | Type of feeding | Total | ||
|---|---|---|---|---|
| Breast Feeding | Bottle Feeding | Both | ||
| <6 months | 7 | 11 | 10 | 28 |
| 6 months to 1 year | 27 | 11 | 29 | 67 |
| 1-2 years | 40 | 30 | 72 | 142 |
| >2 years | 5 | 2 | 6 | 13 |
| Total | 79 | 54 | 117 | 250 |
Table 2: Types and duration of feeding
Discussion
We analyzed the relationship between environmental factors and T1DM in children and adolescents<18 years of age and assessed for their age, birth weight, mode of delivery, and type of feeding. This topic has received significant attention from researchers worldwide. Our study had a medium sample size and our data were acquired from computerized registries with almost complete coverage of information. We considered other confounding factors such as type 2 diabetes mellitus, and maturity-onset diabetes mellitus of the young.
Vitamin D interacts with the immune system in different ways [5]; hence, its concentration in relation to T1DM, among other autoimmune diseases, has been largely investigated, although evidence on the relationship between vitamin D and T1DM remains controversial [6]. Vitamin D deficiency among T1DM patients was high and almost correlated with glycemic control, in a study conducted between January and December 2013 at the outpatient department of King Abdul-Aziz University Hospital, where, 77% diabetes mellitus patients had decreased vitamin D levels. In addition, 66% patients had impaired vitamin D levels with poorly controlled blood sugar (hemoglobin A1c [HbA1c]>9%). Furthermore, the results of the study demonstrated that vitamin D supplementation could aid in managing glucose levels [7].
Another study involving 60 Saudi adults with T1DM and 60 normal controls (non-diabetes mellitus individuals) demonstrated that vitamin D insufficiency was higher in adults with T1DM than the non-diabetes mellitus controls. Furthermore, vitamin D insufficiency was frequent in Saudi due to cultural and social factors such as the decreased exposure to both sunlight and vitamin D supplements [8].
Talaat et al. [9] proposed that vitamin D may play a role in the pathogenesis of T1DM and demonstrated that in T1DM children, insufficient levels of 25[OH] D correlated with elevated HbA1c levels, circulatory cytokines, and antibody markers [9].
A systematic review and meta-analysis of five observational studies (four case-control studies and one cohort study) and no randomized controlled trials, examined if vitamin D supplementation in infancy reduced T1DM development in later life. The study stated that observational studies provided evidence that vitamin D supplementation in infancy can protect against the development of T1DM in adults. However, for a solid conclusion to be achieved, randomized controlled trials with long periods of follow-up are recommended [10].
Mäkinen et al. [6] investigated if there were measurable variances in serum 25[OH] D concentrations among children who developed T1DM (cases) and those who remained non-diabetic with no islet autoantibodies (controls) who were followed up from birth until disease onset. The results of the study by Mäkinen et al. [6] revealed that serum 25[OH] D concentrations were not associated with the development of T1DM in Finland; although, vitamin D consumption has been linked with the development of T1DM for quite some time [11]. In addition, decreased serum 25[OH] D concentrations have been noted in T1DM cases more often than in controls worldwide [12-17]. The changes in 25[OH] D concentrations may be observed following the diagnosis, since T1DM can influence vitamin D metabolism, and T1DM-related problems could lead to a decrease in vitamin D-binding protein via excretion into the urine [18]. The outcomes of this prospective study propose that the progress of T1DM is not correlated with marked changes in vitamin D status [6].
In our study, the descriptive results demonstrated that 55.6% cases had vitamin D deficiency and 44.4% did not have vitamin D deficiency. This suggests that vitamin D could contribute to the process of the disease and in its control [7].
Some studies demonstrated that there was no association between low socioeconomic status and T1DM; however, they revealed that low socioeconomic status may be associated with an increased incidence of severe hypoglycemia in children and adolescents, with T1DM. Low socioeconomic status of parents of patients and of patients themselves has strong influence on the development of end-stage renal disease in T1DM [19,20]. Low socioeconomic status with the need for income support increases the risk of mortality in patients with childhood-onset T1DM and implicated in patients who died after the age of 18 years [21]. In our study, we observed an association between a family with >5 members with good income as well as those who live in an apartment with no consanguinity and T1DM.
A population-based Norwegian cohort study evaluated births between 1989 and 1998 and identified 1824 T1DM cases. A negative result was observed between maternal age at birth and T1DM among firstborn children; however, among fourth born children, there was a 43.2% increase in the incidence of diabetes mellitus for each 5-year increase in maternal age [22].
On the other hand, a study from the United Kingdom assessed the effect of parental age and risk of diabetes mellitus within a large population, based on the cohort of children with diabetes mellitus and their siblings. An increase in maternal age at childbirth was associated with a log linear increase in the risk of diabetes mellitus in the offspring [23]. In our study, we observed that the mothers of 100 out of 250 (40.5%) children and adolescents were 20-29-years-old at the time of their delivery and 123 out of 250 (49.8%) were 30-39-years-old at the time of delivery. This means that increase in maternal age is associated with an increased risk of T1DM in their children.
There are several studies investigating the relationship between Body Mass Index (BMI) and low birth weight and T1DM. All children were aged between 38-40 weeks of gestational age. We noted that diabetes mellitus patients had lower birth weight and lower BMI at birth than healthy children. Children with diabetes mellitus demonstrated a significant increase in BMI during the first two years of life. Children with the lowest BMI at birth were the youngest at onset of T1DM. BMI at diagnosis was not related to any of the variables studied. There were no sex differences. Awadalla et al. [24] demonstrated that low BMI at birth and increase in BMI in the later years of life were risk factors for T1DM; this appeared to be related to the intrauterine environment. Previous studies suggested that birth weight and weight gain during the first year of life are related to the risk of T1DM in later life. Another study suggested that environmental factors during prenatal life may influence the risk of T1DM. It has been proposed that low birth weight, which was shown to be a risk factor for type 2 diabetes mellitus was associated with an increased risk of T1DM [25-27]. The results from a metaanalysis indicate that high birth weight is significantly associated with an increased risk of developing T1DM in later life. However, to date, there are no data to indicate that low birth weight and/or slow weight gain during infancy led to the development of T1DM later in life. Another study demonstrates a different result showing the relationship between birth weight, early weight gain, and subsequent risk of type 1 diabetes mellitus [28]. A control study in Norway on 471 children revealed a significant association between birth weight and the risk of T1DM [29]. In contrast, our study demonstrated that there is no significant association between birth weight and increased risk of T1DM, which is based on the result observed with various birth weights; 76% cases had normal birth weight and T1DM.
A meta-analysis of observational studies performed in the UK revealed that there is a 20% increase in the risk of T1DM in children born via caesarean section [30]. Based on our results, we observed that 30.8% of the children who developed type T1DM were delivered via cesarean section.
A study conducted in Sweden from 1984 to 2012 did not find a high risk of T1DM in the age group<18 years among children born via cesarean section. Unadjusted data revealed a strong correlation between the incidence of pediatric T1DM and cesarean section. The unadjusted Odds Ratio (OR) of 1.12 was in line with that from other studies; however, after adjustments for potential confounders, there was no risk found [31].
Another study demonstrated that delivery via cesarean section is related to a relative risk of approximately 1.2 for pediatric T1DM, with varying results among different studies. New results from the German BABYDIAB study demonstrated that cesarean section did not increase the risk for islet autoantibodies but increased the risk of progression from islet autoimmunity to clinical T1DM. Further research to validate this finding should be replicated in other longitudinal studies to investigate the mechanism of this relationship with islet autoimmunity or with progression from islet autoimmunity to pediatric T1DM [32].
A systematic review conducted by Patelarou et al. [33] demonstrated a protective association between breastfeeding for at least 6 months after birth and development of T1DM. Most studies in this systematic review revealed that absence of breastfeeding or breastfeeding for a short period is a major risk factor for the development of T1DM. The protective effect of breast milk may be attributed to its antimicrobial properties, which protect the infant against a broad range of microorganisms [33]. Thus, breastfeeding appears to protect infants from infections by enteroviruses and B-cell autoimmunity that could result in the development of T1DM [34]. Some studies have provided adequate evidence that early introduction of cow milk in the first year of life was associated with a high risk of T1DM [35- 37].
The risk of diabetes mellitus via cow milk could be explained by early immunization to bovine insulin that occurs in some individuals; whether this initiates an autoimmune response to human insulin and insulinproducing B cells remains to be confirmed [38,39]. However, some studies did not find a relationship between diabetes mellitus autoimmunity and duration of breastfeeding or early exposure to cow milk [40,41], while another study did [42]. In our study we observed that 28 (11.2%) infants were fed milk for<6 months, 67 (26.8%) infants were fed milk for 6 months to 1 year, 142 (56.8%) infants were fed milk for 1-2 years, and 13 (5.2%) infants were fed milk for>2 years. In addition, we noted that 79 (31.6%) infants were breast fed, 54 (21.6%) babies were bottle fed, and 117 (46.8%) infants were fed via both.
In conclusion, our study identified the most common environmental factors that influenced the incidence of T1DM in children and adolescents. Low birth weight was not a significant risk factor of T1DM. However, normal birth weight, maternal age F>30 years, vaginal birth, feeding type, low vitamin D levels in children, and a good socioeconomic status demonstrated a strong significant association with T1DM. We recommend that children should be given vitamin D supplement due to lack of exposure to sunlight and vitamin supplements.
References
- Yoon JW, Jun HS. Autoimmune destruction of pancreatic beta cells. Am J Ther. 2017;12:580-91.
- Al-Rubeaan K. National surveillance for type 1, type 2 diabetes mellitus and prediabetes Mellitus among children and adolescents: a population-based study (SAUDI-DM). J Epidemiol Community Health. 2015;69:1045-51.
- Cardwell CR, Stene LC, Joner G, et al. Maternal age at birth and childhood type 1 Diabetes Mellitus: A pooled analysis of 30 observational studies. Diabetes Mellitus. 2010;59:486-94.
- Gale EA. The rise of childhood type 1 diabetes mellitus in the 20th century. Diabetes Mellitus. 2002;51:3353-61.
- Cantorna MT, Snyder L, Lin YD, et al. Vitamin D and 1, 25(OH) 2 D regulation of T cells. Nutr. 2015;7:3011-21.
- Mäkinen M, Mykkänen J, Koskinen M, et al. Serum 25-hydroxyvitamin D concentrations in children progressing to autoimmunity and clinical type 1 diabetes mellitus. J Clin Endocrinol Metab. 2016;101:723-9.
- Al Agha A, Ihab AA. Association among vitamin d deficiency, type 1 diabetes mellitus and glycemic control. J Diabetes Mellitus Metab. 2015;6:1-5.
- Al-Daghri NM, Al-Attas OS, Alokail MS, et al. Lower vitamin D status is more common among Saudi adults with Diabetes Mellitus type 1 than in non-diabetics. BMC Public Health. 2014;14:153.
- Talaat IM, Nasr A, Alsulaimani AA, et al. Association between type 1, type 2 cytokines, diabetic autoantibodies and 25-hydroxyvitamin D in children with type 1 diabetes mellitus. J Endocrinol Invest 2016;39:1425-34.
- Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 Diabetes Mellitus: a systematic review and meta-analysis. Arch Dis Child. 2008;93:512-7.
- Hyppönen E, Laara E, Reunanen A, et al. Intake of vitamin D and risk of type 1 Diabetes Mellitus: A birth-cohort study. Lancet. 2001;358:1500-3.
- Bin-Abbas BS, Jabari MA, Issa SD, et al. Vitamin D levels in Saudi children with type 1 diabetes mellitus. Saudi Med J. 2011;32:582-92.
- Littorin B, Blom P, Schölin A, et al. Lower levels of plasma 25-hydroxyvitamin D among young adults at diagnosis of autoimmune type 1 Diabetes Mellitus compared with control subjects: Results from the nationwide Diabetes Mellitus Incidence Study in Sweden (DISS). Diabetologia. 2006;49:2847-52.
- Greer RM, Portelli SL, Hung BS-M, et al. Serum vitamin D levels are lower in Australian children and adolescents with type 1 Diabetes Mellitus than in children without Diabetes Mellitus. Pediatr Diabetes Mellitus. 2013;14:31-41.
- Pozzilli P, Manfrini S, Crino A, et al. Low levels of 25-hydroxyvitamin D3 and 1, 25-dihydroxyvitamin D3 in patients with newly diagnosed type 1 Diabetes Mellitus. Horm Metab Res. 2005;37:680-3.
- Janner M, Ballinari P, Mullis PE, et al. High prevalence of vitamin D deficiency in children and adolescents with type 1 Diabetes Mellitus. Swiss Med Wkly. 2010;140:W13091.
- Bener A, Alsaied A, Al-Ali M, et al. High prevalence of vitamin D deficiency in type 1 Diabetes Mellitus and healthy children. Acta Diabetol. 2009;46:183-9.
- Thrailkill KM, Jo CH, Cockrell GE, et al. Enhanced excretion of vitamin D binding protein in type 1 Diabetes Mellitus: A role in vitamin D deficiency? J Clin Endocrinol Metab. 2011;96:142-9.
- Toppe C, Mollsten A, Schon S, et al. Socioeconomic factors influencing the development of end stage renal disease in people with Type 1 Diabetes Mellitus-A longitudinal population study. Diabet Med. 2017;34:676-82.
- Sawka AM, Boulos P, Talib AS, et al. Low socioeconomic status and increased risk of severe hypoglycemia in type 1 Diabetes Mellitus: a systematic literature review. Can J Diabetes Mellitus. 2007;31:233-41.
- Bruno G, Spadea T, Picariello R, et al. Piedmont Study Group for Diabetes Mellitus Epidemiology. Early life socioeconomic indicators and risk of type 1 Diabetes Mellitus in children and young adults. J Pediatr. 2013;162:600-5.
- Stene LC, Magnus P, Lie RT, et al. Maternal and paternal age at delivery, birth order, and risk of childhood onset type 1 Diabetes Mellitus: population based cohort study. Bmj. 2001;323:69.
- Bingley PJ, Douek IF, Rogers CA, et al. Influence of maternal age at delivery and birth order on risk of type 1 Diabetes Mellitus in childhood: prospective population based family study. Bmj. 2000;321:420-4.
- Awadalla NJ, Hegazy AA, Abd El-Salam M, et al. Environmental factors associated with type 1 diabetes mellitus development: A case control study in Egypt. Int J Environ Res Public Health. 2017;14:615.
- Harder T, Rodekamp E, Schellong K, et al. Birth weight and subsequent risk of type 2 Diabetes Mellitus: A meta-analysis. Am J Epidemiol. 2007;165:849-57.
- Whincup PH, Kaye SJ, Owen CG, et al. Birth weight and risk of type 2 Diabetes Mellitus: A systematic review. Jama. 2008;300:2886-97.
- Stene LC, Joner G, Norwegian Childhood Diabetes Mellitus Study Group. Atopic disorders and risk of childhood onset type 1 Diabetes Mellitus in individuals. Clin Exp Allergy. 2004;34:201-6.
- Harder T, Roepke K, Diller N, et al. Birth weight, early weight gain, and subsequent risk of type 1 Diabetes Mellitus: systematic review and meta-analysis. Am J Epidemiol. 2009;169:1428-36.
- Stene LC, Thorsby PM, Berg JP, et al. The relation between size at birth and risk of type 1 Diabetes Mellitus is not influenced by adjustment for the insulin gene (-23HphI) polymorphism or HLA-DQ genotype. Diabetologia. 2006;49:2068-73.
- Cardwell CR, Stene LC, Joner G, et al. Caesarean section is associated with an increased risk of childhood-onset type 1 Diabetes Mellitus: a meta-analysis of observational studies. Diabetologia. 2008;51:726-35.
- Samuelsson U, Lindell N, Bladh M, et al. Caesarean section per se does not increase the risk of offspring developing type 1 Diabetes Mellitus: A Swedish population-based study. Diabetologia. 2015;58:2517-24.
- Stene LC, Gale EA. The prenatal environment and type 1 Diabetes Mellitus. Diabetologia. 2013;56:1888-97.
- Patelarou E, Girvalaki C, Brokalaki H, et al. Current evidence on the associations of breastfeeding, infant formula, and cow's milk introduction with type 1 Diabetes Mellitus: A systematic review. Nutr Rev. 2012;70:509-19.
- Sadeharju K, Knip M, Virtanen SM, et al. Finnish TRIGR Study Group. Maternal antibodies in breast milk protect the child from enterovirus infections. Pediatrics. 2007;119:941-6.
- Hyppönen E, Kenward MG, Virtanen SM, et al. Infant feeding, early weight gain, and risk of type 1 Diabetes Mellitus. Childhood Diabetes Mellitus in Finland (DiMe) Study Group. Diabetes Mellitus Care. 1999;22:1961-5.
- Ahadi M, Tabatabaeiyan M, Moazzami K. Association between environmental factors and risk of type 1 Diabetes Mellitus-A case-control study. Endokrynol Pol. 2011;62:134-7.
- Virtanen SM, Knip M. Nutritional risk predictors of β cell autoimmunity and type 1 Diabetes Mellitus at a young age. Am J Clin Nutr. 2003;78:1053-67.
- Vaarala O, Knip M, Paronen J, et al. Cow's milk formula feeding induces primary immunization to insulin in infants at genetic risk for type 1 Diabetes Mellitus. Diabetes Mellitus. 1999;48:1389-94.
- Vaarala O. The gut immune system and type 1 Diabetes Mellitus. Ann N Y Acad Sci. 2002;958:39-46.
- Couper JJ, Steele C, Beresford S, et al. Lack of association between duration of breast-feeding or introduction of cow's milk and development of islet autoimmunity. Diabetes Mellitus. 1999;48:2145-9.
- Ziegler AG, Schmid S, Huber D, et al. Early infant feeding and risk of developing type 1 Diabetes Mellitus–associated autoantibodies. Jama. 2003;290:1721-8.
- Kimpimäki T, Erkkola M, Korhonen S, et al. Short-term exclusive breastfeeding predisposes young children with increased genetic risk of Type I Diabetes Mellitus to progressive beta-cell autoimmunity. Diabetologia. 2001;44:63-9.