Case Report - Otolaryngology Online Journal (2018) Volume 8, Issue 4
Efficacy of Peripheral Neurectomy in the Management of Refractory Cases of Trigeminal Neuralgia
- *Corresponding Author:
- Colonel Priya Jeyaraj
MDS, Classified Specialist (Oral and Maxillofacial Surgery)
Commanding Officer, Military Dental Centre (Gough Lines)
Secunderabad, Telangana, India
Tel: +919596840303
E-mail: jeyarajpriya@yahoo.com
Received date: November 8, 2018; Accepted date: November 30, 2018; Published date: December 6, 2018
Abstract
The treatment modalities to afford a cure from the intractable pain associated with Trigeminal neuralgia have been wide and varied. Six cases of Trigeminal neuralgia, three affecting the Infraorbital branch of the Maxillary division and three involving the Inferior Alveolar branch of the Mandibular division are presented. The neuralgia in all these cases had become refractory to increasing doses of medication. All six patients were thereafter successfully treated by Peripheral Neurectomy of the involved nerve trunks, which resulted in a complete resolution of all symptoms with no recurrence even after a follow up period of three to five years. Histopathological and immunohistochemical examination of the extirpated nerve fibers revealed varying degrees of axonal degeneration and demyelination of the nerve sheaths at different locations, which could be a contributory or even an etiological factor of the condition, thus corroborating and confirming the relevance and efficacy of the mildly invasive surgical procedure of Peripheral Neurectomy in affording a permanent cure of the refractory neuralgic pain. In addition, an adjunctive measure has been proposed and elucidated, which comprises of electrocauterisation of the nerve canal and foramen following the nerve extirpation, which could prevent possible regeneration of remnants of the nerve fibers, in this way, further ensuring a permanent resolution and cure, with nil recurrence.
Keywords
Trigeminal neuralgia; Tic doloureux; Peripheral neurectomy; Electrocauterisation
Introduction
Trigeminal neuralgia (TN) also known as ‘tic doloureux’, is a neuropathic pain syndrome, characterized by severe unilateral paroxysmal facial pain. The condition is described as a sudden, intermittent, severe, sharp, paroxysmal, spasmodic, lancinating, usually unilateral pain in the facial region along the distribution of one or more branches of the Trigeminal nerve [1], lasting from seconds to minutes and triggered by trivial stimuli such as talking, eating, shaving, brushing the teeth, washing the face, or even a wisp of a breeze on the face.
The pain is severe enough to cause the patient to grimace in agony and live in constant fear and apprehension of the next episode. Episodes of pain increase in frequency, severity and duration with passage of time and intervening periods of remission grow shorter, unless definitive treatment is instituted [2].
The condition most commonly affects individuals over the age of 40, and can affect both genders with a slight predilection for females [2].
Stimulation of certain areas of the face, which may be either intraoral or cutaneous, often elicits an attack.
An area of facial skin or oral mucosa where lowintensity mechanical stimulation (such as light touch, an air puff, or even hair-bending) can elicit a typical pain attack, is typically referred to as the ‘Trigger zone’. It is usually a few millimetres in size and found in the perioral regions such as the lips, cheek, chin, nose etc.
TN has an idiopathic primary etiology and can also secondarily result from compression of the Trigeminal nerve root or nucleus by vessels (aneurysms), multiple sclerosis (due to sclerotic plaque compression) [3] or tumors (angiomas and vascular malformations), as a result of mechanisms such as direct tumoral compression, neurovascular compression or chemical irritation by neoplastic factors [3,4].
Other etiologic factors proposed include Diabetes Mellitus, Herpes Simplex Virus, Allergies, Congenital skull base deformities, Sagging of hind brain, Non myelinating lesions of pons or medulla, infiltrative disorders of the Trigeminal nerve, nucleus, ganglion or root [3,5].
One of the most important etiological factors of this condition is idiopathic or secondary demyelination of the involved nerve fibers, resulting in hyperexcitability of the sensory neurons which thence discharge bursts, resulting in the episodes of pain [4].
A diagnostic nerve block with a local anesthetic, of the branch involved will most likely confirm the diagnosis of TN.
Other investigations for refractory cases of TN include Computed Tomographic scans to rule out intracranial tumors, and to visualize the anatomic landmarks around the Trigeminal (Gasserian) ganglion and the Cerebellopontine angle to aid in open surgical intervention.
TN pain typically remits and relapses in an unpredictable manner, even when patients are on conventionally used medications, thus resulting in considerable debility and a poor quality of life. A wide range of drugs which include carbamazepine, oxcarbazepine, phenytoin, gabapentin, baclofen, lamotrigine and topiramate have been conventionally used to treat TN [5,6].
These drugs act by blocking the Na+ channels and altering the conductance of Ca++, Na+ and K+ ions across the nerve cell membranes, thus preventing generation or reducing the number of action potentials. These drugs are effective for a while, following which their dosage often needs to be increased and suitably titrated to provide the same degree of pain relief. Also the drugs have numerous side effects at even therapeutic doses, such as gingival hypertrophy, hirsutism, osteomalacia, megaloblastic anemia, ataxia, vertigo, nystagmus and diplopia [7].
Several invasive approaches such as botulinum toxin injection [8], trigeminal nerve block at the level of the sphenopalatine ganglion, microvascular decompression, radiofrequency rhizotomy [9], etc. have been performed for the seemingly elusive relief from pain.
However, none of these methods are free of complications and recurrence of pain after a temporary period of remission is only too common. Regional nerve blocks afford only temporary relief [10,11].
This article describes the efficacy of a minor surgical procedure, namely, Peripheral neurectomy of the involved branch of the Trigeminal Nerve in bringing about a permanent resolution of the condition.
Adjunctive steps taken intraoperatively to prevent or retard regeneration of the nerve fibers within the empty have also been described, which help to afford a permanent cure for this debilitating and distressing condition.
Case Series
A 62-year-old edentulous male patient reported with the complaint of severe, episodic, shooting pain on the left side of his face which had first started over two years ago and had increased in severity and duration of each attack over the past six months.
The spasmodic pin was triggered by rinsing his mouth and on eating. He had undergone conservative treatment in the form of medications, which included painkillers as well anti-seizure drugs such as carbamazepine and gabapentin, prescribed by various practitioners and had also undergone multiple dental extractions (for suspected dental etiology of the pain) until he had become completely edentulous. However there was no remission of the painful episodes which continued unabated, and in fact increased in severity and frequency over time.
On clinical examination, intra oral palpation of the left mandibular vestibule region triggered off an episode of excruciating, lancinating pain over left temporal, pre auricular and mandibular body and symphyseal regions.
The pain did not cross the midline and could be relieved by administration of a right inferior alveolar nerve block with 2% lignocaine. This was diagnostic of Trigeminal neuralgia involving the mandibular division on the left side affecting the inferior alveolar and mental branches.
The patient was taken up for surgery under General anesthesia for peripheral neurectomy of the inferior alveolar and mental branches of the Mandibular division of the Trigeminal nerve on the left, via an intraoral approach.
After local infiltration of 2% Lignocaine with 1:80,000 Adrenaline, an incision was placed along the anterior border of the left ramus of the mandible, and a mucoperiosteal flap was raised exposing the site of entry of the inferior alveolar nerve into the mandibular foramen on the lingual side of the ramus at the region of the lingula.
The nerve was firmly grasped with a hemostat, dissected as far posteriorly as was possible, where it was then transected.
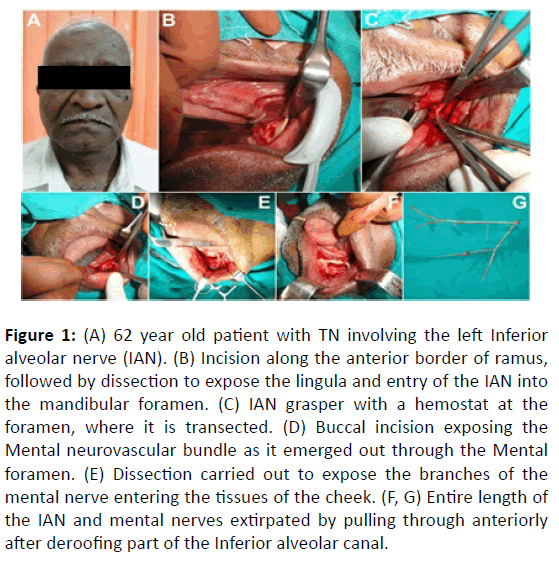
Thereafter, a vestibular incision was placed and a mucoperiosteal flap raised in 33, 34 and 35 region, exposing the mental neurovascular bundle exiting the body of the mandible at the mental foramen. The branches of the mental nerve were carefully dissected free, separating them out from the surrounding tissues (Figure 1).
Figure 1: (A) 62 year old patient with TN involving the left Inferior alveolar nerve (IAN). (B) Incision along the anterior border of ramus, followed by dissection to expose the lingula and entry of the IAN into the mandibular foramen. (C) IAN grasper with a hemostat at the foramen, where it is transected. (D) Buccal incision exposing the Mental neurovascular bundle as it emerged out through the Mental foramen. (E) Dissection carried out to expose the branches of the mental nerve entering the tissues of the cheek. (F, G) Entire length of the IAN and mental nerves extirpated by pulling through anteriorly after deroofing part of the Inferior alveolar canal.
The main trunk was grasped with a hemostat, the mandibular canal was then deroofed to the required distance, and the grasped mental nerve pulled through, by firmly tugging on the hemostat anteriorly, thereby extirpating the entire inferior alveolar nerve.
Sharp bony margins were smoothed using vulcanite trimmers and the exposed canal and foramen regions were thoroughly cauterized with electrocautery as an adjunctive measure to prevent any chance of future regeneration of nerve filaments in the region. Hemostasis was achieved followed by soft tissue closure of the operated sites.
The patient recovered uneventfully and without any complications and there was a complete resolution of the neuralgic pain with no recurrence of the episodic attacks throughout the follow up period of three years.
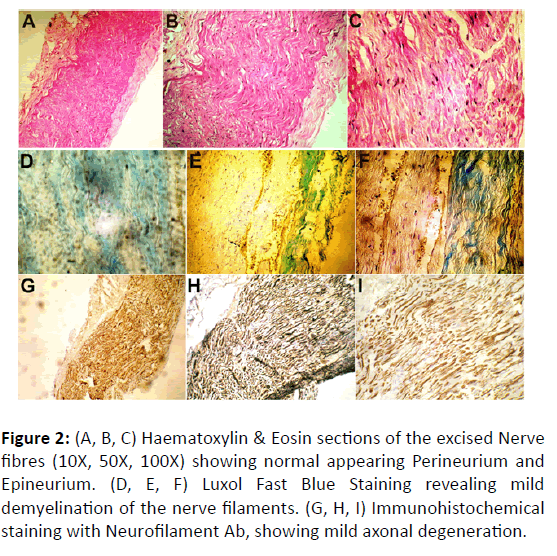
The extirpated nerve fibers were sent for histopathological and immunohistochemical examination (Figure 2). HPE revealed nerve fibers with seemingly normal epineurium and Perineurium (Figures 2A-2C).
Figure 2: (A, B, C) Haematoxylin & Eosin sections of the excised Nerve fibres (10X, 50X, 100X) showing normal appearing Perineurium and Epineurium. (D, E, F) Luxol Fast Blue Staining revealing mild demyelination of the nerve filaments. (G, H, I) Immunohistochemical staining with Neurofilament Ab, showing mild axonal degeneration.
Luxol Fast Blue staining revealed demyelination of the axon sheaths of the nerve filaments at different locations (Figures 2D-2F). Immunohistochemical staining with Neurofilament Antibody revealed a mild axonal degeneration at various locations of the nerve filaments, which could well be an etiological and contributory factor of the typical painful episodes of the neuralgia (Figures 2G-2I).
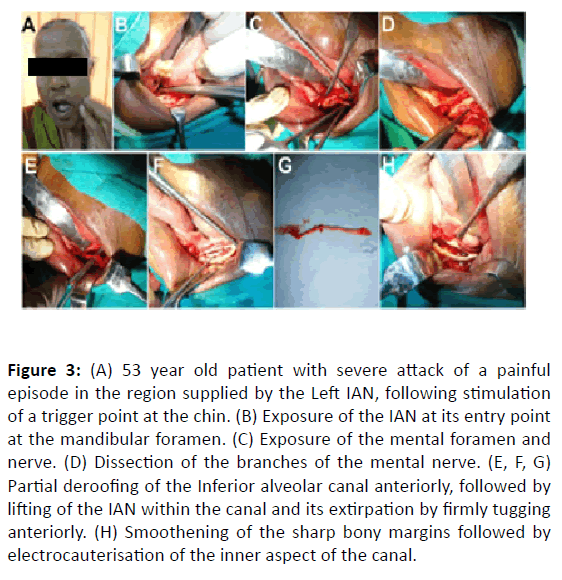
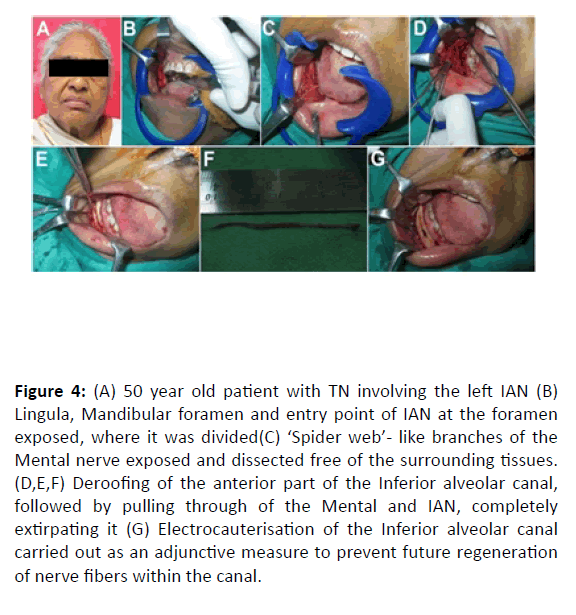
Two other cases of TN involving the Inferior Alveolar Nerve (IAN) in a 53 and a 50 year old female patient (Figures 3 and 4) were treated in a similar manner with an excellent outcome with total resolution of the neuralgic pain with nil recurrence in the entire four year follow up period.
Figure 3: (A) 53 year old patient with severe attack of a painful episode in the region supplied by the Left IAN, following stimulation of a trigger point at the chin. (B) Exposure of the IAN at its entry point at the mandibular foramen. (C) Exposure of the mental foramen and nerve. (D) Dissection of the branches of the mental nerve. (E, F, G) Partial deroofing of the Inferior alveolar canal anteriorly, followed by lifting of the IAN within the canal and its extirpation by firmly tugging anteriorly. (H) Smoothening of the sharp bony margins followed by electrocauterisation of the inner aspect of the canal.
Figure 4: (A) 50 year old patient with TN involving the left IAN (B) Lingula, Mandibular foramen and entry point of IAN at the foramen exposed, where it was divided(C) ‘Spider web’- like branches of the Mental nerve exposed and dissected free of the surrounding tissues. (D,E,F) Deroofing of the anterior part of the Inferior alveolar canal, followed by pulling through of the Mental and IAN, completely extirpating it (G) Electrocauterisation of the Inferior alveolar canal carried out as an adjunctive measure to prevent future regeneration of nerve fibers within the canal.
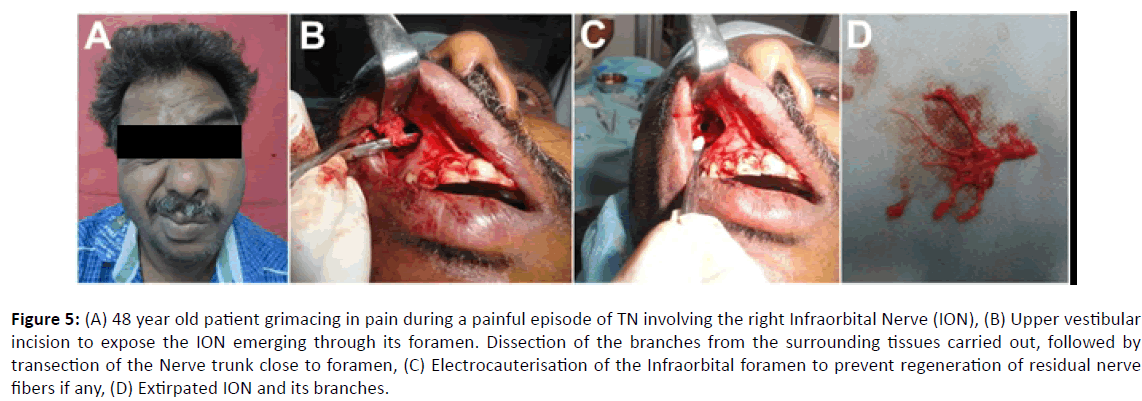
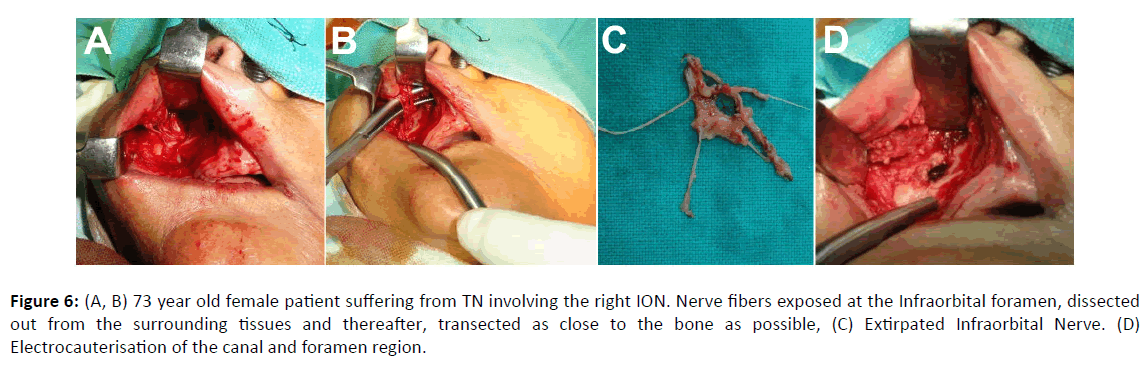
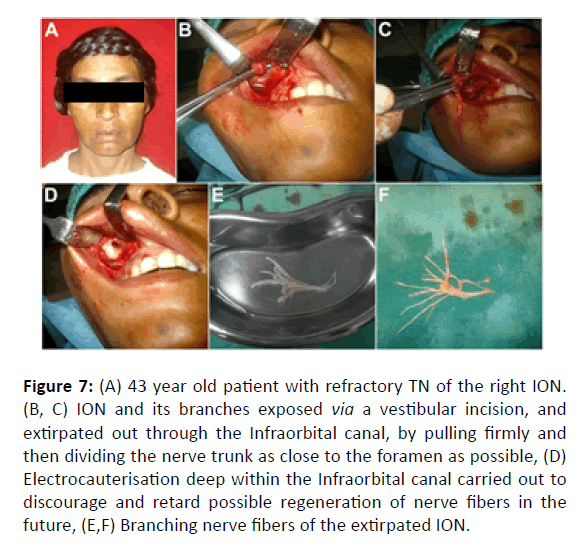
Three patients, a 48-year-old male (Figure 5), a 73- old-female (Figure 6) and a 43-year-old female (Figure 7) exhibited TN with involvement of the Infraorbital branch of the Maxillary division of the Trigeminal nerve. In all these three cases, an upper buccal vestibular incision was placed, and a mucoperiosteal flap raised to expose the Infraorbital nerve (ION) exiting from the Infraorbital foramen.
Figure 5: (A) 48 year old patient grimacing in pain during a painful episode of TN involving the right Infraorbital Nerve (ION), (B) Upper vestibular incision to expose the ION emerging through its foramen. Dissection of the branches from the surrounding tissues carried out, followed by transection of the Nerve trunk close to foramen, (C) Electrocauterisation of the Infraorbital foramen to prevent regeneration of residual nerve fibers if any, (D) Extirpated ION and its branches.
Figure 6: (A, B) 73 year old female patient suffering from TN involving the right ION. Nerve fibers exposed at the Infraorbital foramen, dissected out from the surrounding tissues and thereafter, transected as close to the bone as possible, (C) Extirpated Infraorbital Nerve. (D) Electrocauterisation of the canal and foramen region.
Figure 7: (A) 43 year old patient with refractory TN of the right ION. (B, C) ION and its branches exposed via a vestibular incision, and extirpated out through the Infraorbital canal, by pulling firmly and then dividing the nerve trunk as close to the foramen as possible, (D) Electrocauterisation deep within the Infraorbital canal carried out to discourage and retard possible regeneration of nerve fibers in the future, (E,F) Branching nerve fibers of the extirpated ION.
The nerve branches were meticulously dissected out from the surrounding tissues, the nerve trunk grasped with a hemostat and pulled anteriorly and then transected as close to the bony foramen as possible.
The foramen and canal were then electrocauterised to destroy any residual nerve filaments within so as to prevent their possible regeneration at a later date. The results were gratifying with a complete resolution from the TN and nil recurrence.
Discussion
Trigeminal Neuralgia is the most common neurologic cause of facial pain and has been described by ‘The International Association for Study of Pain’ as a sudden, usually unilateral, severe, brief, stabbing, lancinating, recurring pain in the distribution of one or more branches of Trigeminal nerve [2]. These patients often live their lives in a constant fear and dread of the next attack of the pain, and history invariably reveals numerous visits to different medical practitioners and surgeons in the search of a seemingly elusive relief from their perpetual agony.
The various treatment modalities that have been employed include:
Invasive techniques (Open method)
• Partial sensory rhizotomy (PSR)
• Microvascular decompression (MVD)
• Radiofrequency Thermocoagulation (RFTC) at Gasserian ganglion
• Tractotomy
• Exploration at the point of exit
• Glycerol gangliolysis
• Rhizotomy
• Radiofrequency Thermocoagulation (RFTC)
• Percutaneous radiofrequency thermocoagulation (PRT)
• Percutaneous balloon compression(PBC)
• Peripheral procedures
• Neurectomy
• Neurolysis
• Electrosurgery
• Cryosurgery
No single treatment modality has been able to provide a permeant cure. Antiepileptic medications remain the mainstay of pharmacotherapy. Medical titration and daily dosing is a must when the condition is treated by medication alone. Many patients with TN eventually may become refractory to drug treatments and a few cases develop severe adverse effects. Resistance has been shown to develop even to the more invasive forms of treatment modalities such as blocking a peripheral nerve supplying the region, Gasserian Nerve block, thermocoagulation for ablation of the Trigeminal ganglion etc.
Glycerol or alcohol gangliolysis comprises of injection of 0.5 to 1.0 mL 100% absolute alcohol or glycerol into trigeminal ganglion within the Meckel’s cave or into the main nerve roots as they arise from the ganglion [12]. The supraorbital nerve, infraorbital nerve, mental nerve, maxillary nerve, mandibular nerve can be blocked. The duration of pain relief has been reported as less than 2 months in 74% (for alcohol) and 4 days (for glycerol). Furthermore, bony sequestrae, skin necrosis, diplopia and burning sensation are frequently encountered complications.
Microvascular decompression (MVD) consists of opening a keyhole in the mastoid area and freeing the trigeminal nerve from the causative compressing/pulsating artery by a piece of Teflon [13]. Although it has been reported to have a success rate of 75%-80% for medically refractory trigeminal neuralgia, it is associated with complications such as cerebellar haematoma, venous infarct, temporary diplopia and permanent facial numbness.
Peripheral Neurectomy is a safe, simple and minimally invasive, minor surgical procedure. It involves transsection of the infraorbital or of the Inferior Alveolar & Mental branches of the Trigeminal nerve as they exit their respective foramina on the facial skeleton, thus interrupting the flow of afferent impulses to the ganglion and thereby to the Centre [14]. As the procedure is minimally invasive, it is particularly of use in aged or debilitated patients in whom other extensive procedures such as MVD or percutaneous ablative procedures are contraindicated.
The average duration of pain remission of 59 months, may be lengthened by cauterizing or redirecting the cut nerve. Alternatively, the nerve could be extirpated followed by cauterization of the foramina, thereby ensuring regeneration of the nerve fibers is prevented, which was the procedure followed in all the cases reported.
The various surgical approaches for peripheral neurectomy of the terminal branches of the Trigeminal nerve are:
Infra orbital neurectomy:
• Intraoral conventional approach
• Brauns transantral approach
Inferior alveolar neurectomy:
• Extra oral approach- Risdon’s incision
• Intra oral approach- Dr Ginwalla’s incision
A few possible adverse effects after this minimal invasive procedure, depending upon the branch of the nerve extirpated, are paresthesia, facial sensory loss, weakness or paralysis of masseter muscles and, rarely, loss of the corneal reflex.
Conclusion
Efficacy of peripheral neurectomy of the involved branch of the Trigeminal nerve in the management of Trigeminal Neuralgia can be attributed to interruption of the conduction of afferent impulses thereby preventing and aborting the episodes of pain. Axonal degeneration of the involved fibers, as visualized on both histopathological as well as immunohistochemical examination of the extirpated nerve bundles, as demonstrated in this study, further correlates and corroborates with the rationale behind this minimally invasive procedure of peripheral neurectomy. It is suggested and proposed that following neurectomy,
electrocauterisation of the foramen and canal may be carried out intraoperatively, so as to prevent regeneration of the nerve fibers over time, which otherwise could lead to a possible recurrence of the condition.
Compliance with Ethical Standards
Disclosure of potential conflicts of interest
The author of this article has not received any research grant, remuneration, or speaker honorarium from any company or committee whatsoever, and neither owns any stock in any company. The author declares that she does not have any conflict of interest.
Research involving human participants and /or animals
All procedures performed on the patients (human participants) involved were in accordance with the ethical standards of the institution and/or national research committee, as well as with the 1964 Helsinki declaration and its later amendments and comparable ethical standards.
Ethical Approval
This article does not contain any new studies with human participants or animals performed by the author.
Informed Consent
Informed consent was obtained from all the individual participants in this study.
Funding
This study was not funded by any organization/ society.
References
- Okeson JP. The classification of orofacial pains. Oral Maxillofacial Surg Clin N Am 2008;20:133-44.
- Scrivani SJ, Mathews ES, Maciewicz RJ. Trigeminal neuralgia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:527-38
- Toda EK. Trigeminal neuralgia: Symptoms, diagnosis, classification and related disorders. Oral Sci Int 2007; 4:1-9.
- Zakrzewska JM, McMillan R. Trigeminal neuralgia: The diagnosis and management of this excruciating and poorly understood facial pain. Postgrad Med J. 2011;87:410-16.
- Stiles MA, Mitrirattanakul S, Evans J. Clinical manual of trigeminal neuralgia. 1st Edition 2007, Taylor & Francis CRC Press.
- Trevor Aj, Katzung BG, Kruidering-Hall MM, Susan B. Masters Katzung & Trevor's Pharmacology: Examination & Board Review, 10th Edition. Chapter 24. Drugs That Act in the Central Nervous System (Antiseizure Drugs)
- Zakrzewska JM, Patsalos PN. Long-term cohort study comparing medical (oxcarbazepine) and surgical management of intractable trigeminal neuralgia.Pain.2002;95:259-66
- Türk U, Ilhan S, Alp R, Sur H. Botulinum toxin and intractable trigeminal neuralgia.Clin Neuropharmacol.2005;28:161-2.
- Kanpolat Y, Savas A, Bekar A, Berk C. Percutaneous controlled trigeminal rhizotomy for the treatment of idiopathic trigeminal neuralgia: 25-year experience with 1,600 patients.Neurosurgery.2001;48:524-32.
- Arner S, Lindblom U, Meyerson BA, Molander C. Prolonged relief of neuralgia after regional anesthetic blocks: A call for further experimental and systematic clinical studies. Pain. 1990;43:287-97.
- Kibler RF, Nathan PW. Relief of pain and paranesthesia by nerve block distal to a lesion. J Neurol Neurosurg Psychiatry. 1960;23:91-8
- Niall. Peripheral alcohol injections in the management of trigeminal Neuralgia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:12-7.
- Sarah. Microvascular decompression for trigeminal neuralgia: Recurrences and complications. J Clin Neuroscience. 2005;12:787-9.
- Revant. Drug treatment of trigeminal neuralgia: A systematic review of the literature. J Oral Maxillofac Surg. 2007;65:40-5.