Research Article - Current Pediatric Research (2022) Volume 26, Issue 2
Efficacy of muscle energy technique on forward head posture and cervical mobility in visually impaired children: A randomized controlled trial
Eman Wagdy1*, Noha Elserty2, Hebatallah Mohamed Said Zaghloul3, Marian Mamdouh Fayez4
1Department of Physical Therapy for Woman and Child Health, Beni-Suef University, Beni Suef, Egypt
2Department of Physical Therapy, College of Basic Science, Benha University, Benha, Egypt
3Department of Musculoskeletal Disorders and Its Surgery, Benha University, Benha, Egypt
4Department of Physical Therapy for Pediatrics, Egyptian Chinese University, Cairo, Egypt
- Corresponding Author:
- Eman Wagdy
Department of Physical Therapy for Woman and Child Health, Beni-Suef University, Beni Suef, Egypt
E-mail: Eman.Wagdy@pt.bsu.edu.eg
Received: 27 January, 2022, Manuscript No. AAJCP-22-52597; Editor assigned: 28 January, 2022, PreQC No. AAJCP-22-52597(PQ);
Reviewed: 10 February, 2022, QC No. AAJCP-22-52597; Revised: 20 February, 2022, Manuscript No. AAJCP-22-52597(R);
Published: 28 February, 2022, DOI:10.35841/0971-9032.26.2.1255-1263.
Abstract
Background: Children with visual impairment don’t have sufficient visual acuity to participate easily in everyday activities and then, maladaptive postural alignment is exist including sway back posture, kyphosis, forward head and rounded shoulder. Aim: This research aimed to evaluate the efficiency of muscle energy technique on forward head posture as well as cervical mobility in visually impaired children. Methods: Fourty children with visual impairment of both sexes aged 8-14 years have been enrolled in this research. They have been assigned into two equal groups at random; the study group receives sub occipital muscle energy technique and both groups receive deep cervical flexor training for 6 weeks. AutoCAD software was used to analyze cervical angles including Craniovertevral (CVA), Craniorotational (CRA), Craniohorizontal (CHA) and, cervical ROM device has been employed to evaluate cervical mobility in all directions for both groups; before and after treatment. Results: After treatment findings revealed a significant increase in Craniovertebralangle (CVA), cervical ROM in all directions while, a significant decrease in Craniorotational (CRA) and Craniohorizontal (CHA) angles (P<0.001) in both groups. In all variables, the study group enhanced significantly more than the control group after treatment. Conclusion: Both techniques of muscle energy and deep cervical flexors training were effective in reducing forward head posture and promoting cervical mobility among visually impaired children. However, a sub occipital muscle energy technique was useful than deep cervical flexors training.
Visual impairment, Forward head, Range of motion, Muscle energy technique.
Introduction
Because vision is the main origin of stimuli, allowing for direct interactions with the outer environment, it has a critical role in the development of the body. Despite the fact that the body requires data from a variety of sensory and proprioceptive organs, vision is the most crucial since it encodes and interprets data from all other senses [1]. Impaired vision from birth or early childhood could have a significant effect on an infant's or child's development, limiting involvement in physical, social, educational, and employment prospects as well as negatively impacting mental health [2].
Visual impairment is defined as a functional restriction of the eyes or the visual system caused by congenital, hereditary, or acquired conditions [3], and can showed as decreased visual acuity or contrast sensitivity, photophobia, diplopia, visual distortion, visual field loss, visual perception problems, or any combination of the aforementioned [4]. It can vary in severity from minor vision loss to complete loss of light perception, as well as partial or entire loss of vision ability, and is often linked to abnormal motor development and coordination [4,5].
School children spend most of their day in doing tasks like writing and reading that require near point vision [3]. This has a great impact on children with visual impairment as they had to keep an abnormal position to have a clear vision which leads to head over trunk misalignment [1,6]. A head-over-trunk misalignment is considered a Forward Head Posture (FHP) in which the head is positioned excessively anteriorly in comparison to a vertical reference line [7]. It is distinguished by upper cervical hyperextension and lower cervical spine flexion, resulting in shortening of the upper neck extensors and weakness in the deep neck flexors [8]. Musculoskeletal dysfunction, neck pain, and limited cervical range of motion are all possible outcomes of such a cervical muscle imbalance [8]. Prior research found that having a higher FHP was related to having a lower Craniovertebral Angle (CVA) and increase in Craniohorizontal Angle (CHA) [7] and Cranio-Rotational Angle (CRA) [9].
Different techniques have been used in improving forward head and cervical mobility such as stretching program [10,11], strengthening exercises for deep cervical flexors [12-18], cervical mobilization [19], Neck and scapular stabilization [20,22], Kendell exercise [23], McKenzie exercise [14,24-26], kinesiotaping and, myofascial release [25].
Muscle Energy Technique (MET) is a type of active muscle-based therapy in which the therapist monitors the patient's voluntary contraction of muscles in a carefully controlled direction versus a counterforce generated by the therapist. It can help with pain relief, stretching tight muscles and fascia, reducing muscular tonus, improving local circulation, strengthening weak musculature, and mobilizing joint limitations [27]. Many studies have shown that using MET may decrease pain, enhance ROM, and decrease the degree of neck disability [16]. Different studies had investigated the effect of MET on forward head and cervical mobility among adults of different ages [11,18,27-29].
So, according to literature reviews, our study was the first randomized controlled trial performed to investigate the efficiency of muscle energy technique on forward head posture as well as cervical mobility in visually impaired children.
Material and Methods
Study design
A randomized clinical study has been approved by the faculty of physical therapy's ethical committee at Cairo university, Egypt (No: P.T.REC/012/002972) and registered on clinicaltrial.gov. (No: NCT04716348). This research was carried out between February and June of 2021. Parents’ informed consent has been obtained prior to the beginning of the research procedure.
Study population and randomization
Fourty children with visual impairment aged from 8-14 years old were recruited from different schools and charity organization for visually impaired children, Cairo, Egypt. The following criteria were used to include children with visual impairment who had been diagnosed by a pediatric ophthalmologist in this research: the children's ages varied from 8 to 14 years, their visual acuity was 6/24, 6/36 and 6/60 after correction, wearing glasses more than one year before recruitment, their craniovertebral angle was <50°, craniohorizontal angle >15°, craniorotational angle >143°, had adequate functional hearing and, able to stand and walk independently. We excluded children with total deafness, visual acuity of or better than 6/18 after correction, spinal deformities, cervical fracture or tumor, injury of cervical region (e.g. atlantoaxial instability), history of previous cervical spine surgery, symptomatic pain, intellectual or/mental disabilities and, regular participation in any sport activities.
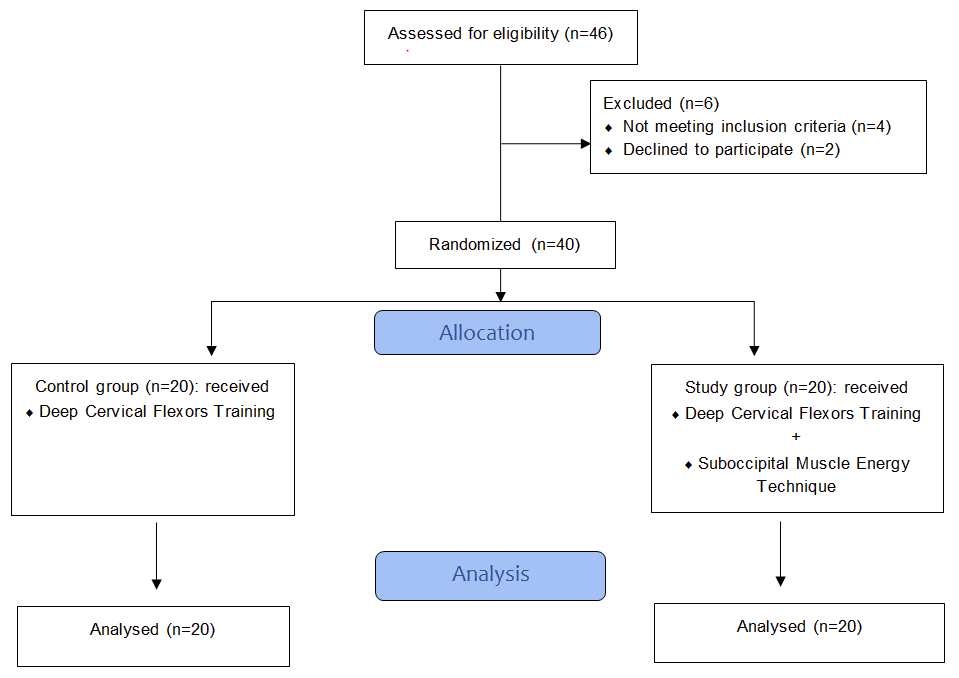
Children were randomly assigned into two groups through sealed enveloped method. The children's allocation CONSORT flow chart was illustrated in Figure 1.
Procedures
Measurement Procedure
Forward head posture: Photogrammetry, a digital imaging technology, has been employed to evaluate head and neck posture while standing from the lateral perspective [30]. It is a simple, easy, and objective way [31,32] with a high interrater and intrarater reliability in assessing FHP [33]. Every child has been instructed to stand in a comfortable position with placing his/her weight equally on bilateral bared feet [34]. A colored adhesive marker [35] has been put on the anatomical points while exposing the child’s neck and upper trunk. The spinouts process of C7, the ear tragus, and the eye's external canthus were the anatomical points [35] used to calculate the selected 3 angles in this study, which are:
- Craniovertebral Angle (CVA): It is the angle formed when a horizontal line passes through the spinous process of C7 as well as a line passes through the ear tragus. It estimates the position of the neck on the upper trunk; a small angle suggests a forward head posture [33].
- Craniorotational Angle (CRA): It is the angle created by the lines linking C7 to the ear tragus and the ear tragus to the eye lateral canthus [30].
- Craniohorizontal Angle (CHA): It is the angle created by a horizontal line passing through the ear tragus and a line connecting the ear tragus and the eye external canthus intersecting. It estimates the head-on-neck angle or upper cervical spine position; a large angle indicates more extension of the head [35].
Each child was asked to look forward [32]. Then, photos were captured by a digital camera (Sony cybershop 8 MP) mounted on a tripod positioned at 2 m from the child's lateral foot [30]. The camera height has been adjusted depending on the child’s height at the level of the ear tragus [33]. Three photos were taken for each child then, saved them on a personal computer and the average of each angle was calculated [9] and analyzed using the auto-CAD software (version 2014) which is a two-dimensional graphical software that includes an electronic drawing sheet.
Cervical mobility: The device of cervical range of motion (CROM) has become one of the clinically accessible methods for measuring cervical ROM as it is easy to use and has test-retest reliability of measurements in all movement directions. It is comprised of a velcro-strapped plastic frame that is put over the nose and ears. Two independent inclinometers are mounted to the frame and point out the head's position in relation to the gravity line for measuring sagittal and frontal plane movements. Another inclinometer used for measuring transverse plane movement which operated in conjunction with a magnet yoke [8].
Each child has been asked to sit upright on a chair while securing the thoracic spine to the chair with a belt strap to avoid any thoracic spine motion. The CROM device (deluxe CROM instrument; Model #12–1,156; fabrication enterprises, white plains, NY) was then placed on the child's head as if they were wearing spectacles [8,36]. All children were given a clear demonstration of the neck motion that needed to be done [37], and they were instructed to do 3 repetitions of neck flexion-extension (sagittal plane), left and right parts of lateral flexion (frontal plane), and rotations (transverse plane) to promote compliance of the soft tissues of the neck and ensure consistency when measuring active CROM [38].
All children have been prompted to self-correct their posture to an upright position with the chin held in before the ROM measurements [8] and instructed to perform each test actively [36] by moving their heads from neutral to maximal flexion, extensions, left lateral flexion, right lateral flexion, left rotations, and right rotation postures [39] until the CROM stopped due to muscle tightness or pain, or until a substitution motion occurs [38]. For every motion, three measurements have been obtained, and the average of the three has been calculated.
Intervention procedures
Children in both the study and control groups received Deep Cervical Flexors (DCF) training using pressure biofeedback unit (PBU-stabilizer TM, Chattanooga group, INC., Chattanooga, TN). The activation of the cervical flexors with PBU is useful for strengthening weaker muscles and thus promoting muscle performance [16].
Children have been given practice sessions with the PBU to learn the Craniocervical Flexion (CCF) movement, and they have been told to relax the neck musculature and focus on allowing a gentle and slow head nodding motion, as well as avoiding head lifts to reduce superficial flexor recruitment. The examiner monitoring and corrected any substitutes throughout the practice phase of the CCF movement to verify that the movement was performed correctly, and any involvement of superficial neck flexor muscles was discouraged by the examiner through verbal feedback [40].
The exercise consists of five progressive phases, beginning with a baseline pressure of 20 mmHg and progressing to 22 mmHg, 24 mmHg, 26 mmHg, 28 mmHg, and 30 mmHg [41]. All of the children were positioned in a crook-lying posture on a plinth. The beginning posture has been standardized by positioning the child's chin and forehead horizontal inside an imagined line parallel to the plinth, extending from the ear tragus and bisecting the neck longitudinally. PBU air bag was clipped together in three fold and, placed sub occipital. Following inserting the deflated pressure sensor behind the neck, right close to the occiput, it has been inflated to a baseline pressure of 20 mmHg to only fill the gap between the neck and the support surface without driving the neck into a lordosis. This gives the child feedback and instructions on how to complete the exercise. Children have been taught how to conduct CCF and have practiced head nodding to gradually target (achieve incremental targets) and hold the 5 levels of pressure between 22 and 30 mmHg for 10 seconds. The CCF exercise program consisted of three sets of ten repetitions every, performed three times per week six weeks with two mints of resting in between sets [42].
The study group also received Post Isometric Relaxation (PIR) technique of Sub Occipital Muscle Energy Technique (SMET). Each child was supine, and the therapist stood on the child's head side. The sub occipital muscle restriction barrier has been detected by placing one hand on the occiput and the other on the C2 spinous process. Whereas the child was encouraged to undertake an isometric contraction of the sub occipital muscle by saying "tip your chin upwards versus the resistance supplied by the therapist's shoulder", the therapist put his anterior portion of the shoulder on the forehead of the child. The child used more than 30% to 40% force to overcome the therapist's resistance. The abovementioned contraction has been sustained for 10 seconds, and the child has been requested to inhale throughout the contraction, followed by an exhale, and the therapist stretched the sub occipital muscle throughout the exhalation stage for 30 seconds, after which the child relaxed for approximately 20 seconds. The muscle has been reintroduced into the new barrier, and the procedure described above has been repeated 5 times [27]. Duration of Suboccipital Muscle Energy Technique (SMET) was 3 times/week for 6 successive weeks.
Sample size
Before the research, the sample size had been computed by G*POWER statistical software (version 3.1.9.2; Franz Faul, Universitat Kiel, Germany) using Craniovertebral Angle (CVA) as the primary outcome, revealing that the suitable sample size for such research had been 20 in each group. The following values were used in the calculations: α=0.05, β=0.2 and effect size= 0.91 and allocation ratio N2/N1 =1.
Statistical analysis
For comparing children's characteristics between groups, descriptive statistics and an unpaired t-test have been employed. The Chi-squared test has been applied to compare sex distributions. The Shapiro-Wilk test has been performed to ensure that the data has a normal distribution. To verify that the groups were homogeneous, Levene's test for homogeneity of variances has been performed. Using a mixed design MANOVA, the effects of the Craniovertebral Angle (CVA), Craniorotational Angle (CRA), Craniohorizontal Angle (CHA), and neck ROM were compared within and between groups. For subsequent multiple comparisons, post-hoc tests employing the Bonferroni correction have been performed. All statistical tests had a significance level of p<0.05. The Statistical Package for Social Studies (SPSS) version 25 for windows has been employed to conduct the statistical analyses (IBM SPSS, Chicago, IL, USA).
Results
Table 1 displays the mean ± SD of the study and control groups' children's age, weight, height, and BMI. The characteristics of the children did not differ significantly between groups (p<0.05).
| Study group | Control group | ||
|---|---|---|---|
| Mean ± SD | Mean ± SD | p-value | |
| Age (years) | 11.55 ± 1.79 | 11.15 ± 1.66 | 0.46 |
| Weight (kg) | 44.35 ± 6.89 | 44.67 ± 6.01 | 0.87 |
| Height (cm) | 146 ± 9.42 | 146.15 ± 9.7 | 0.96 |
| BMI (kg/m²) | 20.7 ± 1.76 | 21.05 ± 1.73 | 0.53 |
| Sex | |||
| Boys | 9 (45%) | 10 (50%) | 0.75 |
| Girls | 11 (55%) | 10 (50%) | |
Table 1. Children's basic characteristics. SD: Standard Deviation; p-value: Probability value.
A significant interaction between treatment and time (F(9,30)=53.09, p=0.001) was discovered using mixed MANOVA. Time had a significant major impact (F(9,30)=655.04, p=0.001). Treatment had a significant major impact (F(9,30)=4.32, p=0.001). Tables 2 and 3 indicated descriptive statistics of Craniovertebral Angle (CVA), Craniorotational Angle (CRA), Craniohorizontal Angle (CHA), and neck ROM and the level of significance of comparison among groups and the level of significance of comparison between before treatment and after treatment in every group.
The study and control groups both had a significant increase in Craniovertebral Angle (CVA) and a significant decrease in Craniorotational Angle (CRA) and Craniohorizontal Angle (CHA) after treatment compared to before treatment (p<0.001). Also, there was significant increment in after treatment neck ROM in both the study and control groups compared to before treatment ROM (p<0.001).
Before treatment, all parameters were not significantly different between the two groups (p>0.05). When the study and control groups have been compared after treatment, the study group had a significant increase in Craniovertebral Angle (CVA) and a significant reduction in Craniorotational Angle (CRA) and Craniohorizontal Angle (CHA) compared to the control group (p<0.01). In addition, when compared to the control group, the study group indicated a significant increase in flexion, extension, rotation, and side bending (p<0.01).
| Study group | Control group | |||
|---|---|---|---|---|
| Mean ±SD | Mean ±SD | MD (95% CI) | P value | |
| CVA (degrees) | ||||
| Before treatment | 45.04 ± 0.91 | 45.49 ± 1.17 | -0.45 (-1.11:0.21) | 0.18 |
| After treatment | 49.28 ± 1.2 | 46.97 ± 0.91 | 2.31 (1.62:3) | 0.001 |
| MD (95% CI) | -4.24 (-4.71:-3.77) | -1.48 (-1.95:-1) | ||
| p=0.001 | p=0.001 | |||
| CRA (degrees) | ||||
| Before treatment | 155.2 ± 1.76 | 155.1 ± 1.61 | 0.1 (-0.98:1.18) | 0.85 |
| After treatment | 151 ± 1.45 | 152.6 ± 1.63 | -1.6 (-2.59:-0.61) | 0.002 |
| MD (95% CI) | 4.2 (3.75:4.64) | 2.5 (2.05:2.94) | ||
| p=0.001 | p=0.001 | |||
| CHA (degrees) | ||||
| Before treatment | 28.02 ± 1.27 | 28.05 ± 1.28 | -0.03 (-0.84:0.79) | 0.95 |
| After treatment | 24.25 ± 1.2 | 26.3 ± 1.08 | -2.05 (-2.78:-1.31) | 0.001 |
| MD (95% CI) | 3.77 (3.38:4.16) | 1.75 (1.35:2.14) | ||
| p=0.001 | p=0.001 | |||
Table 2. Mean Craniovertebral Angle (CVA), Craniorotational Angle (CRA), Craniohorizontal Angle (CHA) of the study and control groups before and after treatment. SD: Standard Deviation; MD: Mean Difference; CI: Confidence Interval; p-value: Level of significance.
| Study Group | Control Group | |||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | MD (95% CI) | P value | |
| ROM (degrees) | ||||
| Flexion | ||||
| Before treatment | 61.75 ± 4.9 | 60.3 ± 3.46 | 1.45 (-1.27:4.17) | 0.28 |
| After treatment | 69.25 ± 4.86 | 65.2 ± 3.65 | 4.05 (1.29:6.8) | 0.005 |
| MD (95% CI) | -7.5 (-8:-6.99) | -4.9 (-5.4:-4.39) | ||
| p=0.001 | p=0.001 | |||
| Extension | ||||
| Before treatment | 65.2 ± 3.6 | 65.6 ± 4.32 | -0.4 (-2.94:2.14) | 0.75 |
| After treatment | 73.2 ± 3.31 | 69.75 ± 4.12 | 3.45 (1.05:5.84) | 0.006 |
| MD (95% CI) | -8 (-8.87-7.12) | -4.15 (-5.02:-3.27) | ||
| p=0.001 | p=0.001 | |||
| Right rotation | ||||
| Before treatment | 66.9 ± 3.47 | 67.4 ± 3.25 | -0.5 (-2.65:1.65) | 0.64 |
| After treatment | 74.35 ± 2.62 | 71.9 ± 2.82 | 2.45 (0.7:4.19) | 0.007 |
| MD (95% CI) | -7.45 (-8.09:-6.8) | -4.5 (-5.14:-3.85) | ||
| p=0.001 | p=0.001 | |||
| Left rotation | ||||
| Before treatment | 65.5 ± 2.87 | 65.9 ± 2.31 | -0.4 (-2.07:1.27) | 0.63 |
| After treatment | 73.2 ± 2.94 | 69.8 ± 2.06 | 3.4 (1.77:5.03) | 0.001 |
| MD (95% CI) | -7.7 (-8.25:-7.15) | -3.9 (-4.45:-3.35) | ||
| p=0.001 | p=0.001 | |||
| Right bending | ||||
| Before treatment | 37.1 ± 2.61 | 37.6 ± 3.05 | -0.5 (-2.31:1.31) | 0.58 |
| After treatment | 42.5 ± 2.16 | 40.3 ± 3.16 | 2.2 (0.46:3.93) | 0.01 |
| MD (95% CI) | -5.4 (-5.88:-4.91) | -2.7 (-3.18:-2.21) | ||
| p=0.001 | p=0.001 | |||
| Left bending | ||||
| Before treatment | 39.4 ± 2.62 | 39.25 ± 2.88 | 0.15 (-1.61:1.91) | 0.86 |
| After treatment | 43.8 ± 1.93 | 41.65 ± 2.71 | 2.15 (0.63:3.66) | 0.006 |
| MD (95% CI) | -4.4 (-4.91:-3.88) | -2.4 (-2.91:-1.88) | ||
| p=0.001 | p=0.001 | |||
Table 3. The study and control groups' mean neck ROM before and after treatment: SD: Standard Deviation; MD: Mean Difference; CI: Confidence Interval; p-value: Level of significance.
Discussion
Normal biomechanics inside the musculoskeletal system require good posture and muscle balance, while bad posture creates muscular imbalance, which leads to abnormal relationship between different body components [43]. As a consequence of a loss of visual data [1] and wearing glasses, children experiencing visual impairment can have postural alterations. FHP is a prevalent postural abnormality in visually impaired children [44], and it induces joint dysfunction and unusual afferent data, influencing the tonic neck reflex by causing extension at the atlanto-occipital (C1 to C2) joints, the lower cervical spine flexion (C4 to C7), and the mid cervical lordosis flattening [10]. Cervical angles are variables used mainly to diagnose forward head posture as the smaller the CVA, the higher the FHP, and the less the mobility of the neck [45] while, increased the CRA and CHA leading to increasing the severity of FHP [35,46].
When a muscle's performance deteriorates, the balance between the stabilizers in the posterior area of the neck and the Deep Cervical Flexors (DCF) is disrupted, leading to a loss of correct alignment and posture. This misalignment may lead to cervical impairment [16,18]. Because the cervical muscles are densely packed with muscle spindles and contribute to improved sensorimotor function, they are critical for preserving neck and head control throughout both static and dynamic activities [47]. As a result, it is critical to recover from forward head posture in terms of improving head’s position and increasing ROM [30] through inhibition, stretching, and training of deep cervical flexors for the correction/normalization of spinal curvature, as well as a reduction in compressional and tensional stress on the joints and its surroundings soft tissues [28].
Muscle Energy Technique (MET) is a versatile technique that has traditionally been employed to treat muscle strain, local edema, as well as joint dysfunction [29]. No studies found the effect of MET on visually impaired children, so our research aims to evaluate the efficiency of MET on forward head posture and cervical mobility in visually impaired children.
The findings of this research revealed that the study and control groups had a statistically significant increase in (CVA), neck ROM in all directions, and a statistically significant reduction in (CRA) and (CHA) after treatment compared to before treatment (p<0.001). Other findings of this research revealed that there had been no significant difference in all parameters between the study and control groups before treatment (p>0.05), but that after treatment, the study group had a significant increase in (CVA), neck ROM in all directions, and a significant decrease in (CRA) and (CHA) compared to the control group (p<0.01).
A number of muscle spindles in the sub occipital muscles help to stabilize the cervical spine by controlling head’s rotational movement and modifying head posture [48]. Edrish et al. [7], Prerana et al. [31] and Maitrayee et al. [33], in their studies related to subjects with FHP and medical students with upper crossed syndrome, asserted that MET declines hyper activation and tightness in shortened muscles. The mechanism behind the results of MET in the form of Post-Isometric Rehabilitation (PIR) and reciprocal inhibition [30] may be a neurophysiologic mechanism that stimulates the Golgi tendon reflex, hinders the alpha motor neuron, and thus hinders the sub occipital muscles, this significantly improving cervical angles as well as the function of the cervical spine [27].
Also, traction provided by the therapist during MET application causes stretching of the posterior neck fascia and the sub occipital muscles and thus increasing the muscles' extensibility and viscoelasticity [27]. Sajjad et al. [11], Syeda et al. [14], Mona et al. [30], Muhammad et al. [28] in their studies related to participants suffering from mechanical neck pain, forward head posture and upper crossed syndrome showed that muscle energy technique increases neck ROM. The mechanism behind the result of Muscle Energy Technique (MET) could be attributed to shifts in muscle expandability, resulting in an increase in muscle length. Also, the inhibiting impact of the Golgi tendon reflex, which is stimulated throughout isometric muscle contraction, results in reflex muscle relaxation and a decrease in muscle spasm and tightness. As a result, the potential explanation for the increase in ROM is based primarily on the impact of autogenic inhibition [27]. Because larger forces can generate enhanced viscoelastic change and passive extensibility, combining contractions and stretches may be more efficient for generating viscoelastic change than passive stretching [29]. Because fluid is propelled throughout the body by changing blood and lymph pressure gradients, rhythmic repetitive muscle contractions conducted throughout MET could help relieve passive congestion in the paraspinal muscles. Fluid drainage from the zygapophyseal joint as well as segmental muscles has also been proposed as a method of making difference ROM and end-feel [29].
Different studies related to subjects with chronic neck pain and cervical spondylotic radiculopathy postulated that training and/or strengthening of deep cervical flexors leads to improvement of cervical angles and correction of the FHP. The mechanism behind the result has been underlined by the fact that DCF has a significant postural function in supporting and straightening the cervical lordosis, leading to improved FHP through refinement of cervical angles [13,17,49,50].
It was reported that strengthening deep craniovertebral flexors can improve muscular function/performance and ROM. Motor learning, which needs data from the outside body and also proprioception, is used to explain the mechanism behind the result. We could enhance motor behavior with biofeedback training by strengthening the patient's goal-oriented behavior. With DCF training with pressure biofeedback, the patient could receive external feedback on his task performance. Participants might also use auditory and/or visual feedback to control the recruitment and frequency of motor unit discharge. Another explanation for increased muscle strength is the application of feedback that can be owing to an increase in the mean firing rate, motor unit recruitment, and active motor unit synchronization [14,16,18,42].
The limitation of this study was the failure to control factors influencing the FHP, such as upper extremity alignment, pelvic tilt, and lower extremity alignment, psychological situation, the environment or physical conditions in which the children live, physiologic alterations due to human growth and development, and time spent using magnification tools besides wearing glasses. Further research with scheduled follow up along with the children’s life span to determine the preservation of changes of cervical angles and ROM. Also, studies to investigate the effect of MET on blind children is recommended.
Conclusion
According to the results of this research, both techniques of muscle energy and deep cervical flexor training were effective in reducing forward head posture and promoting cervical mobility among visually impaired children. However, a sub occipital muscle energy technique was useful than deep cervical flexors training.
Conflict of Interest
The authors have not declared any conflict of interest.
References
- Michelle DP, Juliana FS, Silvia MAJ. Quantitative postural analysis of children with congenital visual impairment. J Manipulative Physiol Ther 2018; 41(1): 62-70. [Crossref][Google Scholar][Indexed]
- Dilay A, Sultan A. Screening of visually impaired children for health problems. Asian Nurs Res (Korean Soc Nurs Sci) 2015; 9(4): 285-90. [Crossref][Google Scholar][Indexed]
- Asmaa SAA, Samia AA, Hossam EE. Visual motor integration of schoolchildren with different levels of myopia. Med J Cairo Univ 2017; 85(2): 475-79. [Crossref][Google Scholar][Indexed]
- Ayanaw TF, Destaye SA, Alemayehu DG, et al. Visual impairment among primary school children in Gondar town, Northwest Ethiopia. J Ophthalmol 2020; 1-6. [Crossref][Google Scholar][Indexed]
- Raphael CMP, Patrícia SV, Míriam RMM, et al. Computerized photogrammetric assessment of postural alignment in visually impaired athletes. J Bodyw Mov Ther 2019; 23(1): 142-47. [Crossref][Google Scholar][Indexed]
- Jovelyn FD. Aerobic exercises: A corrective measure to postural defects of children with visual impairment. IJCDSE 2011; 2(4): 534-39. [Crossref][Google Scholar][Indexed]
- Apoorva K, Amrutkuvar R. A study of relation between myopia and head posture in young adult population. Indian J Public Health Res Dev 2020; 11(5): 49-54. [Crossref][Google Scholar]
- Bo-Been K, Ji-Hyun L, Hyo-Jung J, et al. Effects of suboccipital release with craniocervical flexion exercise on craniocervical alignment and extrinsic cervical muscle activity in subjects with forward head posture. J Electromyogr Kinesiol 2016; 30: 31-37. [Crossref][Google Scholar][Indexed]
- Seung-Hyean O, Kyung-Tae Y. The effects of stabilization exercises using a sling and stretching on the range of motion and cervical alignment of straight neck patients. J Phys Ther Sci 2016; 28(2): 372-7. [Crossref][Google Scholar][Indexed]
- Rodrigo MR, Pedro P-C, Ana IC. Effects of a resistance and stretching training program on forward head and protracted shoulder posture in adolescents. J Manipulative and Physiol Ther 2017; 40(1): 1-10. [Crossref][Google Scholar][Indexed]
- Syeda NG, Qurat-ul-ain, Shakil UR, et al. Effects of eccentric muscle energy technique versus static stretching exercises in the management of cervical dysfunction in upper cross syndrome: A randomized control trial. J Pak Med Assoc 2020; 70(3): 394-98. [Crossref][Google Scholar][Indexed]
- Ahmad HA, Zaheen AI. Effect of deep cervical flexor muscle training using pressure biofeedback on pain and forward head posture in school teachers with neck pain: An observational study. BioMed Res Int 2021; 5588580. [Crossref][Google Scholar][Indexed]
- Bhuvan DG, Shagun A, Bharat G, et al. Effect of deep cervical flexor training conventional isometric training on forward head posture, pain, neck disability index in dentists suffering from chronic neck pain. J Clin Diagn Res 2013; 7(10): 2261-4. [Crossref][Google Scholar][Indexed]
- Vijay K, Nishita YP, Mangala PP. To compare the effects of deep neck flexors strengthening exercise and McKenzie neck exercise in subjects with forward neck posture: a randomized clinical trial. Int J Physiother Res 2016; 4(2): 1451-58. [Crossref][Google Scholar][Indexed]
- Isha S, Chandan C, Shveta S, et al. Effects of deep cervical flexor training on forward head posture, neck pain, and functional status in adolescents using computer regularly. BioMed Res Int 2020; 1-7. [Crossref][Google Scholar][Indexed]
- Dong YK. Deep cervical flexor training with a pressure biofeedback unit is an effective method for maintaining neck mobility and muscular endurance in college students with forward head posture. J Phys Ther Sci 2015; 27(10): 3207-10. [Crossref][Google Scholar][Indexed]
- Thavatchai S, Rungthip P, Sureeporn U, et al. Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: A randomized controlled trial. J Pain Res 2019; 7(12): 915-25. [Crossref][Google Scholar][Indexed]
- Harshita Y, Manu G. Efficacy of muscle energy technique and deep neck flexors training in mechanical neck pain - a randomized clinical trial. Int J Ther Rehabil Res 2015; 4(1):52-66. [Crossref][Google Scholar][Indexed]
- Ho JA, Shin JP. Effects of cervical spine mobilization on respiratory function and cervical angles of stroke patients: A pilot study. Healthcare (Basel) 2021; 9(4): 377. [Crossref][Google Scholar][Indexed]
- Kiana F, Amir L, Malihe H. The effect of manual therapy and stabilizing exercises on forward head and rounded shoulder postures: A six-week intervention with a one-month follow-up study. BMC Musculoskelet Disord 2019; 20(86): 86. [Crossref][Google Scholar][Indexed]
- Na-Yeon K, Sang-Cheol I, Kyoung K. Effects of a combination of scapular stabilization and thoracic extension exercises for office workers with forward head posture on the craniovertebral angle, respiration, pain, and disability: A randomized-controlled trial. Turk J Phys Med Rehabil. 2021; 67(3): 291-99. [Crossref][Google Scholar][Indexed]
- Jeong-Il K, Hyun-Ho C, Dae-Keun J, et al. Effect of scapular stabilization exercise on neck alignment and muscle activity in patients with forward head posture. J Phys Ther Sci 2018; 30(6): 804-808. [Crossref][Google Scholar][Indexed]
- Yong- Soo K, Yu- Mi K, Je-Myung S. The effect of modified cervical exercise on smartphone users with forward head posture. J Phys Ther Sci 2017; 29(2): 328-31. [Crossref][Google Scholar][Indexed]
- SeYoon K, JuHyeon J, NanSoo K. The effects of McKenzie exercise on forward head posture and respiratory function. J Kor Phys Ther 2019; 31(6): 351-57. [Crossref][Google Scholar][Indexed]
- Jiyoung K, Sungjoong K, Jemyung S, et al. Effects of mckenzie exercise, kinesio taping, and myofascial release on the forward head posture. J Phys Ther Sci 2018; 30(8): 1103-07. [Crossref][Google Scholar][Indexed]
- Eun-Young K, Keun-Jo K, Hee-Ryong P. Comparison of the effects of deep neck flexor strengthening exercises and Mackenzie neck exercises on head forward postures due to the use of smartphones. Indian J Sci Technol 2015; 8(7): 569-75. [Crossref][Google Scholar]
- Mona HE, Khaled ZF. Effect of post isometric relaxation technique in the treatment of mechanical neck pain. Phys Ther Rehabili 2018; 5:1-6. [Crossref][Google Scholar][Indexed]
- Muhammad O, Naureen T, Reem JM. Effect of muscle energy techniques and facet joint mobilization on spinal curvature in patients with mechanical neck pain: A pilot study. J Pak Med Assoc 2020; 70(2):344-347. [Crossref][Google Scholar][Indexed]
- Karen LL, Gary F, Patrick M. The effect of muscle energy technique on gross trunk range of motion. JOM 2003; 6(1):13-18. [Crossref][Google Scholar][Indexed]
- Drashti T, Varadhrajulu G, Mandar M. The effect of forward head posture on spinal curvatures in healthy subjects. Asian Pac J Health Sci 2018; 5(1): 60-3. [Crossref][Google Scholar][Indexed]
- Han-suk L, Hyung-kuk C, Sun-wook P. The analysis of severity of forward head posture with observation and photographic method. J Korean Soc Phys Med 2015; 10(3): 9-17. [Crossref][Google Scholar] [Indexed]
- Xiaofei G, Guoxin F, Xinbo W, et al. Photographic measurement of head and cervical posture when viewing mobile phone: A pilot study. Eur Spine J 2015; 24(12): 2892-8. [Crossref][Google Scholar][Indexed]
- Aliaa RY. Photogrammetric quantification of forward head posture is side dependent in healthy participants and patients with mechanical neck pain. Int J Physiother 2016; 3 (3): 326-31. [Crossref][Google Scholar][Indexed]
- Suresh M, Shobha S, Baharuddin O, et al. Quantitative measurements of forward head posture in a clinical setting: a technical feasibility study. Eur J Physiother 2017; 19(3):1-5. [Crossref][Google Scholar][Indexed]
- Marwa MI, Nadia LR. The effect of prolonged time of tablet usage on postural alignment in children. Asian J Appl Sci. 2018; 6(6):396-402. [Crossref][Google Scholar]
- June Q, Yong-Hao P, Ross AC, et al. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther 2013; 18(1): 65-71. [Crossref][Google Scholar][Indexed]
- Karthi M, Gopalswami AD, Antony LA. Efficacy of endurance training on deep cervical flexor muscles using pressure feedback in mechanical neck pain. Int J Physiother 2019; 6(3): 95-101. [Crossref][Google Scholar]
- SinHo C, Yeon-Gyu J. Effects of the craniocervical flexion and isometric neck exercise compared in patients with chronic neck pain: A randomized controlled trial. Physipother Thepry Pract 2018; 34(12): 916-25. [Crossref][Google Scholar][Indexed]
- Yi-Liang K, Tsung-Han L, Yi-Ju T. Evaluation of a cervical stabilization exercise program for pain, disability, and physical impairments in university violinists with nonspecific neck pain. Int J Environ Res Public Health 2020; 17(15): 1-11. [Crossref][Google Scholar][Indexed]
- Marwa SMS, Nagwa IR, Moussa AS. Effect of deep cervical fle