Research Article - Current Pediatric Research (2022) Volume 26, Issue 5
Efficacy of core stabilization versus active self-correction exercises in the treatment of adolescents with idiopathic scoliosis.
Ezzat El Sayed Moubarak1*, Sobhy Mahmoud Aly2, Mohamed K Seyam3, Ahmed Abd El-Moneim Abd El-Hakim4, Radwa S Abdulrahman5,6 and Amina Awad7
1Department of Rheumatology and Rehabilitation, College of Physical Therapy, Zagazig University Hospital, Egypt
2Department of Biomechanics, College of Physical Therapy, Cairo University, Cairo, Egypt
3Department of Physical Therapy and Health Rehabilitation, Majmaah University, Saudi Arabia
4Department of Physical Therapy for Basic Sciences, College of Physical Therapy, Beni-Suef University, Eg ypt
5Department of Physical Therapy for Pediatrics, College of Physical Therapy, Cairo University, Cairo, Egypt
6Department of Physical Therapy for Pediatrics and Pediatrics Surgery, College of Physical Therapy, Badr University in Cairo, Cairo, Egypt
7Department of Physical Therapy for Neurology, College of Physical Therapy, Cairo University, Cairo, Egypt
- Corresponding Author:
- Ezzat El Sayed Moubarak, Department of Rheumatology and Rehabilitation, College of Physical Therapy, Zagazig University Hospital, Egypt, E-mail: melsayed@horus.edu.eg
Received: 11 May, 2022, Manuscript No. AAJCP-22-63501; Editor assigned: 12 May, 2022, PreQC No. AAJCP-22-63501(PQ); Reviewed: 28 May, 2022, QC No. AAJCP-22-63501; Revised: 02 June, 2022, Manuscript No. AAJCP-22-63501(R); Published: 09 June, 2022, DOI:10.35841/0971-9032.26.5.1371-1380
Abstract
Background: Numerous therapeutic exercises are used in the rehabilitation of scoliosis. However, there is a lack of studies that compare the effectiveness of core stabilization and active self-correction exercises in treating adolescent idiopathic scoliosis. Objectives: To compare the effects of Core Stabilization (CS) and Active Self-Correction (ASC) exercises in treating adolescents with mild idiopathic scoliosis. Methods: A comparative study was conducted on thirty adolescents with mild idiopathic scoliosis; aged 10-14 years old, with Cobb’s angle between (10°–20°) and Risser grade below 2°, who were randomly assigned into two groups; CS (n=15) and ASC (n=15). Both groups were treated by three supervised sessions weekly for 12 successive weeks and a home program. Outcomes: The primary measures included; the Cobb angle, the Sørensen test for assessing back muscle endurance, and the trunk forward flexion test for assessing back flexibility. The secondary outcome measure was the Scoliosis Research Society-22 (SRS-22) questionnaire for evaluating the Quality of Life (QoL). All measures were assessed at baseline and after the intervention. Results: The CS group showed remarkable results in all measures; Cobb angle, the Sørensen test, trunk forward flexion test, and the total score of SRS-22, compared to ASC one except for the mental health domain of the SSR-22 showed a non-significant difference between the groups post-treatment. Post-treatment, the self-image and function domains showed a non-significant change in the ASC group. Conclusion: The core stabilization program is superior to active-self correction exercises in the shortterm treatment of mild adolescent idiopathic scoliosis.
Keywords
Adolescent idiopathic scoliosis, Core stabilization, Active self-correction, Cobb angle, Spinal flexibility, Back endurance, QoL.
Introduction
Scoliosis is a complex three-dimensional torsional deformity of the spine and trunk with a lateral curvature, vertebral rotation, and possibly a reduced kyphotic and lordotic normal curve [1]. Idiopathic Scoliosis (IS) is the most common type of scoliosis, representing 80%-90% of all types, and refers to the scoliosis of the unspecified origin or disease with multifactorial etiology [2,3]; genetic, hormonal, neuromuscular, skeletal, biomechanical, environmental and/or lifestyle factors [4]. Idiopathic scoliosis might appear at any time from childhood to adulthood. The prevalence of Adolescent IS (AIS) is about 2.5% in the general population [5]; however, the prevalence is found to be wider (0.93% to 12%) in the adolescent with a Cobb angle of more than 10°, with a female-male ratio of about 1.3:1 when the Cobb angle between 10° to 20° [6].
The combination of many factors influences the risk of curve progression, gender, age, and curve degrees at presentation. The higher risk appears in females and children aged 10–12 years with a Cobb angle >25° at presentation [5,6]. The improper mechanical force system acting on the spine in AIS can lead to physiological and biomechanical changes along the trunk segment and cause several complications; postural asymmetry, loss of spinal flexibility with muscle imbalance, back pain, cosmetic deformity, particularly changes in chest geometry and symmetry of the trunk, elevation of the ribs and the scapula, and psychological deficits which can all negatively impact the individual self-satisfaction and quality of life (QoL) [3,7].
In 2016, the international Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) stated in its guidelines that the goals of conservative treatment of IS include both morphological and functional objectives to reduce the curve progression, eliminate pain, improve the patient breathing, cosmetic appearance, and QoL. Conservative treatment is considered to be effective when the Cobb angle is <40° and typically involves exercise therapy, braces, and spinal adjustment therapy. Physiotherapeutic scoliosis-specific exercises (e.g., schroth method), other general exercises (e.g., strengthening, stretching, mobilization) and machine-assisted exercises are all found to be effective in the treatment of mild to moderate AIS [3,5,8].
Core Stabilization (CS) exercise has been suggested as an effective treatment for increasing spinal strength and stability in AIS. Improvement in curve angle, pain, chest mobility, and postural alignment has been shown after CS exercises in children and adults with scoliosis. CS exercise evolves training of the deep trunk muscles to build the balance between internal and external forces, acting over the back and control the trunk in both static and dynamic positions. This approach integrates respiratory control and rib cage position with spinal, scapular, and neck-head positions [9-11].
Active Self-Correction (ASC) exercises are defined as the performance of active motions to achieve the possible correction of spinal deformity. The ASC program is a rehabilitative technique designed according to the characteristics of the scoliotic curve and includes strengthening of deep spinal muscles; while maintaining postural selfcorrection and stretching of back and limb muscles [12,13]. Reviewing the literature, each CS and ASC program was combined with other conservative treatments and positively revealed improved spinal curvature, mobility, strength, and neuromuscular imbalance [3,11]. However, and to our knowledge, no study compares the efficacy of the two approaches in subjects with AIS. For that reason, the present study aimed to compare the effects of core stabilization and active self-correction exercises in treating adolescents with mild idiopathic scoliosis.
Subjects and Methods
Study design
A prospective randomized comparative study was conducted between June 2020 and March 2022 in the outpatient clinic of Zagazig university hospital. All participants and their parents were fully informed about the aim and methods used in the study. In their agreement to their children’s participation in the study, a written informed consent form was obtained from all parents. The study was approved by the institutional review board of the Zagazig university (ZU-IRB No. #6608-14-12-2020), registered on the PACTR website (PACTR 2022201788162241), and followed the declaration of Helsinki standards.
Enrollment
An orthopedic surgeon referred thirty adolescents with IS to the outpatient clinic of Zagazig university hospital. Before enrollment, subjects’ eligibility to participate in the study was assessed.
Participants
Thirty patients of both sexes (19 females and 11 males) with AIS were included in the study and randomly assigned into two groups; CS (n=15) and ASC (n=15). To be included in the study, participants should be diagnosed as AIS, aged between 10 and 14 years, have mild scoliosis in which a primary curve magnitude ranging between 10° and 20° Cobb’s angle, have a Risser score below two, and be able to participate in the study [13-15]. Patients were excluded if they have any or combination of the followings; any diagnosable cause of scoliosis, leg-length discrepancy, lower limb deformities interfering with spinal curvature, congenital scoliosis, history of spinal surgery or correction, musculoskeletal or neurological disease, spinal pathology, cardiopulmonary, renal or vestibular diseases. Patients with any psychological or cognitive dysfunction that might interfere with performing the treatment exercises or the assessment were excluded [11,16].
Intervention
Patients in each group, CS (n=15) and ASC (n=15), received 60 minutes of supervised sessions three times per week regularly every other day for successive 12 weeks. Each therapeutic session started by warming up (10 minutes), followed by exercises (40 minutes), and terminated with cooling down (10 minutes). Warming up and cooling down exercises include stretching, strengthening, and breathing exercises. Patients were also instructed to perform daily exercises at home for 20 minutes with the help of parents when needed. A booklet illustrating the exercises was given to participants to ensure the accuracy of exercise performance. A video record of home performance was sent to the physiotherapist regularly to guarantee patient compliance with treatment.
Core Stabilization (CS) exercises
Core exercises started by training the core muscles local activation in static positions and gradually progressed to improve endurance and control in dynamic positions and functional tasks. First, the patient was trained to activate the core muscles in a static position to improve the proprioceptive awareness of the core area. As core awareness improved, the patient was asked to keep controlling the core area in a more dynamic pattern as follows; basic trunk curl from a crook lying position, bridging exercises, cat-camel exercises from a quadruped position, single and double-leg abdominal press, and quadruped arm/leg raises. Antero-posterior and lateral pelvic control exercises (tilt) from sitting and standing were also performed. Each exercise was repeated 10 to 15 times [11,13,17,18]. All exercises were supervised by the same qualified physiotherapist to ensure the accuracy of performed movements.
Active Self-Correction (ASC) exercises
The ASC exercises included; primary and contiguous spinal curves corrections in the frontal plane, controlled self-stretch in the sagittal plane, and finally, correction of the primary curve in the transverse plane [15,19,20]. Treatment was tailored and taught to each patient according to the presented spinal deformity. Correcting the thoracic curve required a selective vertebral oblique (bottom-up) deflection and sagittal correction with increasing kyphosis and preserving lordosis (Figure 1a). For correcting lumber scoliotic curves, vertebral lateral deflection and sagittal correction with increasing lordosis and reducing thoracolumbar kyphosis were performed (Figure 1b). To correct thoracolumbar curves, a selective vertebral oblique deflection and sagittal correction with increasing lordosis and reducing thoracolumbar kyphosis were practiced (Figure 1c). The aim of selective vertebrae deflections and sagittal corrections was the horizontal de-rotation of vertebrae [12]. Exercises were performed under the supervision of a qualified physiotherapist.
Outcome Measures
The study included four outcome measures, three primary measures, and one secondary measure evaluated before and after 12 weeks of rehabilitation.
The primary outcome measures included:
Cobb angle measurements: The Cobb method is a standard and an objective method with a high degree of reliability in quantifying the spinal curve magnitude, making decisions about the curve progression, and the need and effectiveness of treatment; conservative and surgical interventions, as well [21,22]. In the present study, the Cobb angle test was conducted by an orthopedic specialist according to the Cobb method [23] and the recommendations of SOROT 2012 [24] in that; thoracic and lumbar anterior and posterior radiographs were taken while the patient assumed the anatomical standing position. Blinded radiographic imaging was then performed for both groups before and after rehabilitation. The intersection of two lines represented the Cobb angle; the first line was parallel to the upper boundary of the top vertebra and the second line was on the bottom edge of the adjacent lower vertebra. The same procedure was applied to this radiographic protocol for all participants. Blinded radiographic imaging was performed for both groups before and after rehabilitation.
The Biering-Sørensen test: This test is a valid and reliable measure of back extensor muscle endurance [25-27]. The test was conducted from a prone lying position with a pillow under the patient’s lower abdomen while the upper back was outside the bed, and the iliac crests were aligned with the edge of the bed. Strapping was applied to stabilize the pelvis, knees, and ankles. The time the patient can maintain the upper body straight and horizontal, with the arms folded across the chest, was measured. The test was stopped after 240 seconds at maximum or if the subject could no longer maintain the test position.
Trunk forward flexion test: This test was used to evaluate spinal flexibility. It showed good validity, reliability, and responsiveness in evaluating total spinal mobility in clinical practice and trials [28]. First, back stretching was performed, then the test was conducted by asking the subject to bend the trunk forward from a standing position as maximum as possible, with extended knees. The distance between C7 to S2 vertebrae was measured using a measuring tape. The test was repeated twice, and the highest value was analyzed [14,29].
The secondary outcome measure included
The Scoliosis Research Society-22 (SRS-22) questionnaire: This questionnaire is a valid and reliable tool for evaluating health-related QoL in people with AIS that showed fair to excellent test-retest reliability and internal consistency. The SRS-22 involves 22 items covering five domains; pain, function/activity, self-perceived image, mental health, and treatment satisfaction. Each domain consists of five items, except the treatment satisfaction, which included only two items. Each item is graded on a scale of one to five (worst to best), from which each domain score is calculated. Calculating the mean value of all domains yields a total score [30,31].
Sample size
Based on the previous study [17], a statistical power analysis was calculated using the OPEN-EPI program, with a power of 0.80, 95% Confidence Intervals (CIs), and α-level of 0.05. The number of participants required for the final analysis was calculated to be 15 for each group considering the primary outcome of the Cobb angle.
Randomization
After obtaining a signed informed consent form, patients were randomized into one of the two programs, CS or ASC, using a computer-generated randomization card. The cards were placed in sealed envelopes opened by a blinded and independent research assistant.
Blinding
The biostatistician and primary investigator; who obtained and assessed the outcome data were blinded to the treatment allocation. However, the physiotherapist; who conducted treatment and patients could not be blinded.
Data Management and Statistical Analysis
Statistical analysis was conducted using the Statistical Package for Social Studies (SPSS) version 25 for windows (IBM SPSS, Chicago, IL, USA). Demographic characteristics of subjects were compared by the unpaired t-test, while the chi-squared test compared sex distribution between groups. The Shapiro- Wilk test was used to evaluate the normal distribution of data. Levene’s test for homogeneity of variances was conducted to test the homogeneity between groups. Mixed MANOVA was used to compare the treatment effects on Cobb angle, Biering- Sørensen, trunk forward flexion, and SRS-22 within and between groups. Post-hoc tests using the Bonferroni correction were carried out for subsequent multiple comparisons. The significance level for all statistical tests was set at p<0.05.
Results
Demographic characteristics
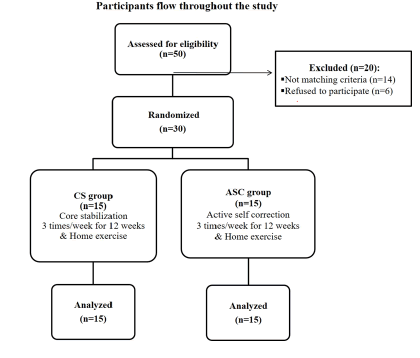
Fifty subjects with AIS were eligible for inclusion in the current study. Only thirty patients were included and randomized into the CS group (n=15) and ASC group (n=15). Figure 2 demonstrates participants’ flow throughout the study. At baseline, all subjects in both groups were matched in their demographic characteristics (p>0.05) (Table 1).
|
|
CS |
ASC |
p-value |
|---|---|---|---|
|
Mean ± SD |
Mean ± SD |
||
|
Age (years) |
11.5 ± 1.58 |
12.03 ± 1.94 |
0.41 |
|
Weight (kg) |
44.26 ± 2.93 |
44.36 ± 5.09 |
0.94 |
|
Height (cm) |
131.93 ± 9.21 |
130.26 ± 9.8 |
0.63 |
|
BMI (kg/m²) |
25.64 ± 2.88 |
26.27 ± 2.76 |
0.54 |
|
Sex |
|||
|
Females |
10 (30%) |
9 (60%) |
0.37 |
|
Males |
5 (70%) |
6 (40%) |
|
Table 1. Subjects’ demographic characteristics. All data were expressed as mean ± SD, except the sex distribution was expressed as nominal counts. CS: Core Stabilization; ASC: Active Self-Correction; SD: Standard Deviation; p-value: Probability Value; Level of significance: (p<0.05).
Effect of treatment on Cobb angle, back endurance, flexibility and QoL
A significant interaction of treatment and time (F=21.92, p=0.001, partial eta square=0.86) was found. A significant main effect of time (F=124.58, p=0.001, partial eta square=0.97) was detected while there was no significant main effect of treatment (F=1.79, p=0.13, =partial eta square 0.41).
Within-group comparison
There was a significant decrease in Cobb angle and a significant increase in Biering- Sørensen and trunk forward flexion tests in both the CS and ASC groups post-treatment compared with pre-treatment (p<0.001). The percent of change of Cobb angle, Biering- Sørensen, and trunk forward flexion tests in the CS group were 28%, 25.47%, and 57.43, respectively, while the ASC group was 15.48%, 13.18%, and 23.78%, respectively (Table 2).
|
|
CS |
ASC |
MD |
95% CI |
||
|---|---|---|---|---|---|---|
|
Mean ± SD |
Mean ± SD |
Lower bound |
Upper bound |
p-value |
||
|
Cobb angle (degrees) |
||||||
|
Pre-treatment |
18.76 ± 3.57 |
19.06 ± 2.62 |
-0.3 |
-2.64 |
2.04 |
0.79 |
|
Post-treatment |
13.51 ± 3.36 |
16.11 ± 3.01 |
-2.6 |
-5 |
-0.21 |
0.03 |
|
MD (% of change) |
5.25 (28) |
2.95 (15.48) |
|
|
|
|
|
|
p=0.001 |
p=0.001 |
|
|
|
|
|
Biering-Sørensen (sec) |
||||||
|
Pre-treatment |
103.13 ± 11 |
99.13 ± 10.9 |
4 |
-4.19 |
12.19 |
0.32 |
|
Post-treatment |
129.4 ± 7.43 |
112.2 ± 9.8 |
17.2 |
10.69 |
23.71 |
0.001 |
|
MD (% of change) |
-26.27 (25.47) |
-13.07 (13.18) |
|
|
|
|
|
|
p=0.001 |
p=0.001 |
|
|
|
|
|
Trunk forward flexion (cm) |
||||||
|
Pre-treatment |
9.02 ± 2.26 |
9.25 ± 2.12 |
-0.23 |
-1.88 |
1.41 |
0.77 |
|
Post-treatment |
14.2 ± 2.21 |
11.45 ± 1.65 |
2.75 |
1.29 |
4.21 |
0.001 |
|
MD (% of change) |
-5.18 (57.43) |
-2.2 (23.78) |
|
|
|
|
|
|
p=0.001 |
p=0.001 |
|
|
|
|
Table 2. Means of Cobb angle, Biering- Sørensen (back endurance), trunk forward flexion (flexibility) tests post-treatment in the CS and ASC groups. SD: Standard Deviation; MD: Mean Difference; CI: Confidence Interval; p-value: Probability Value; Level of significance: (p<0.05).
Regarding the SRS-22, the CS group showed a significant increase in the total score and all domains of the questionnaire post-treatment compared with pre-treatment (p<0.001). There was a significant increase in the total score and most of the domains post-treatment in the ASC group. Only self-image and function domains did not show significant change after treatment (p>0.05) (Table 3).
| SRS-22 Domains | CS | ASC | MD | 95% CI | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Lower bound | Upper bound | p-value | ||
| Pain | ||||||
| Pre-treatment | 3.15 ± 0.29 | 3.28 ± 0.3 | -0.13 | -0.35 | 0.1 | 0.25 |
| Post-treatment | 3.62 ± 0.29 | 3.39 ± 0.23 | 0.23 | 0.03 | 0.43 | 0.02 |
| MD (% of change) | -0.47 (14.92) | -0.11 (3.35) | ||||
| p=0.001 | p=0.004 | |||||
| Self-image | ||||||
| Pre-treatment | 3.04 ± 0.25 | 3.02 ± 0.15 | 0.02 | -0.14 | 0.17 | 0.85 |
| Post-treatment | 3.2 ± 0.25 | 3.08 ± 0.14 | 0.12 | -0.04 | 0.27 | 0.14 |
| MD (% of change) | -0.16 (5.26) | -0.06 (2) | ||||
| p=0.001 | p=0.054 | |||||
| Function | ||||||
| Pre-treatment | 3.08 ± 0.28 | 3.13 ± 0.2 | -0.05 | -0.23 | 0.14 | 0.61 |
| Post-treatment | 3.33 ± 0.23 | 3.23 ± o.25 | 0.1 | -0.08 | 0.28 | 0.27 |
| MD (% of change) | -0.25 (8.12) | -0.1 (3.19) | ||||
| p=0.001 | p=0.07 | |||||
| Mental health | ||||||
| Pre-treatment | 3.06 ± 0.22 | 3.14 ± 0.28 | -0.08 | -0.27 | 0.12 | 0.44 |
| Post-treatment | 3.21 ± 0.21 | 3.27 ± 0.21 | -0.06 | -0.22 | 0.1 | 0.45 |
| MD (% of change) | -0.15 (4.9) | -0.13 (4.14) | ||||
| p=0.001 | p=0.002 | |||||
| Satisfaction | ||||||
| Pre-treatment | 4.18 ± 0.29 | 4.12 ± 0.20 | 0.06 | -0.14 | 0.24 | 0.57 |
| Post-treatment | 4.48 ± 0.22 | 4.27 ± 0.24 | 0.21 | 0.03 | 0.38 | 0.02 |
| MD (% of change) | -0.3 (7.18) | -0.15 (3.64) | ||||
| p=0.001 | p=0.001 | |||||
| Total score | ||||||
| Pre-treatment | 3.31 ± 0.12 | 3.34 ± 0.13 | -0.03 | -0.13 | 0.06 | 0.43 |
| Post-treatment | 3.56 ± 0.12 | 3.45 ± 0.13 | 0.11 | 0.02 | 0.21 | 0.01 |
| MD (% of change) | -0.25 (7.55) | -0.11 (3.29) | ||||
| p=0.001 | p=0.001 | |||||
Table 3. Mean scores of the SRS-22 questionnaire in the CS and ASC groups. CS: Core Stabilization; ASC: Active Self-Correction; SD: Standard Deviation; MD: Mean Difference; CI: Confidence Interval; p-value: Probability Value; Level of Significance: (p<0.05).
Between-group comparison
At pre-treatment, results revealed a non-significant difference in all measures (p>0.05). Post-treatment, the results revealed a significant decrease in Cobb’s angle (p<0.05) and a significant increase in Biering-Sørensen test (p<0.001), trunk forward flexion test (p<0.001), total score of SRS-22 (p<0.01), pain and satisfaction domains of the SRS-22 (p<0.05) in favor of the CS group. However, there was no significant difference in selfimage, function and mental health between groups (p>0.05) (Tables 2 and 3).
Discussion
This study aimed to compare the effects of core stabilization, and active self-correction exercises on adolescents with mild idiopathic scoliosis. To the authors’ knowledge, no study compared the effects of two programs on AIS; however, both interventions were recommended by the SOSORT-2016 as effective conservative treatments in idiopathic scoliosis [3].
Our results showed significant improvement in each group, however; the CS group showed remarkable results in all measures (Cobb angle, forward-flexion test for spinal flexibility, Sørensen test for back endurance, and SSR-22 for QoL) compared to the ASC group except for the mental health domain of the SSR-22 which showed non-significant difference between groups post-treatment. These findings could support that the CS program is superior to the ASC one in the short-term treatment of AIS.
The improvement differences between the two groups may be attributed to the mechanism of working and the effects of each exercise program.
In the ASC program, the patients autonomously perform a series of movements of global body realignment to reduce the scoliotic curves. Self-correction training has to be performed in three planes which could be sometimes difficult for the patient [20]. However, in the CS program, a specified selective activation of core stabilizers, especially multifidus, transverse abdominus, and paraspinal muscles, was performed by enhancing co-contraction between the superficial and deep spinal muscles to provide global and local stability. This neuromuscular coordination improves neuromotor control, spinal alignment, and trunk position in static posture and functional activities. In other words, the CS exercises work concerning the concept of motor control and learning. The core exercises facilitate motor learning by recruiting the muscles in isolation, which activates the motor pathways and enhances the subject’s motor awareness [32,33]. With repeated practice, feed forward and feedback mechanisms of motor control can be developed. Therefore, improving sensory awareness of the core area and trunk allows the patient to realign and maintain a correct posture of his trunk [9,34,35].
Findings of the present study revealed a significantly improved Cobb’s angle in both groups; however, this improvement was in favor of the CS group. The Cobb angle is considered an important measure of scoliotic curve progression and helps making management decisions [6,36]. Findings of the present study revealed a significantly improved Cobb angle in both groups; however, this improvement was in favor of the CS group. Exercise therapy is found to be effective in relatively mild scoliosis with a Cobb angle ranging between 10° and 20° [3]. As all participants in the present study had a single mild scoliotic curve; categorized according to the SOSORT classification in 2016, with a mean angle of 18.76 ± 3.57 and 19.06 ± 2.62 for CS and ASC groups, respectively, this could explain the significant reduction of the Cobb angle in both groups. Concerning the effect of exercise on Cobb’s angle, the developed neuromuscular activation of trunk stabilizers after CS training reduces the vertebral rotation associated with scoliosis and reeducates the muscles to stabilize the curve against rotation [11,37].
Although the vertebral rotation was not measured in this work, the mentioned effects of the CS program might explain the discrepancy of results between the two groups regarding their curve progression measured by Cobb angle. Several studies revealed the positive impact of the CS program on scoliosis. A meta-analysis conducted by Li et al. concluded the effectiveness of core-based exercise in reducing Cobb angle in short-term treatment [38]. Our results agreed with the study of Ko et al. which revealed the significant effect of 12- week core stabilization exercises on reducing Cobb’s angle in children with AIS compared to the control group [14]. Another study conducted by Gür et al. reported that a 10 week CS training combined with traditional exercises reduced the thoracic and lumbar Cobb angles in AIS compared with traditional exercise alone [11]. Moreover, Park et al. reported that a 10-week CS exercise program could reduce the Cobb angle for male college students with scoliosis compared with a home-based exercise program [39].
In contrast to our results, Yagci et al. reported a non-significant difference in the Cobb angle after applying the combined CS with bracing compared to the Scientific Exercise Approach to Scoliosis (SEAS); which is based on the ASC program in the short-term treatment of AIS [13]. However, the results of Negrini et al. agreed with ours; in that they found the SEAS was significantly effective in reducing Cobb angle in comparison to the conventional physiotherapy in mild AIS (mean Cobb angle is 15 ± 6) [16]. This discrepancy in results between the mentioned studies could be related to the difference in sample criteria; moderate AIS with double curve deformity in Yagci et al. and mild AIS with a single curve in our study and in that of Negrini et al. Another study conducted by Monticone et al. 2014 also reported positive effects of combing the ASC with a task-oriented approach on reducing Cobb angle in AIS [12].
Another finding in this work was the evident improvement of back flexibility and spinal muscle endurance in the CS group compared to the ASC one. Scoliosis can impair spinal flexibility and mobility since it causes a spinal deformity of variant degrees [40]. For that reason, 2016-SOSORT guidelines reported improving spinal flexibility and mobility as very important goals in scoliotic rehabilitation [3]. In this work, back flexibility and spinal muscle endurance showed better improvement in the CS group compared to the ASC one. While applying the CS program, the patient was trained to selectively activate spinal muscles in static posture and functional activity [9,33], which was supposed to improve our participants' general spinal flexibility and mobility. Concerning the concept of motor control, spinal stability and mobility are highly correlated and dependent on the coordinated activity of all spinal muscles surrounding the lumbar area [41].
The CS program is more than back strengthening exercise; it improves trunk muscles endurance through the motor relearning principles provided through the proprioceptive neuromuscular control of a coordinated movement of the core area and, consequently, positively impacts spinal endurance and mobility. Our results agreed with some studies that reported that the CS program was superior to the traditional back strengthening exercises in improving back flexibility and endurance [35,42,43]. Furthermore, Ko et al. revealed a significant difference in the muscle strength and flexibility between the CS group and the control one in patients with AIS [14]. Park et al. also reported improved trunk muscle strength after the CS program compared to a home-based exercise program in adult males with functional scoliosis [39].
Another observation in the present study was the significantly improved QoL in both groups. The CS group showed a remarkable difference in the total and domain scores of the SRS-22 questionnaire, excluding the domain of mental health, which showed no difference between groups post-treatment. The self-image and function domains did not significantly differ in the ASC group post-treatment. Studies reported that the QoL is significantly affected in patients with idiopathic scoliosis. The appearance and aesthetic self-perception caused by spinal deformity result in physical and psychological consequences and thus negatively impact the QoL of people with idiopathic scoliosis. Therefore, correction of trunk deformity is an important goal in the conservative treatment of scoliosis [44,45].
Results of the QoL in this work were consistent with other reports [38,46]. A recent meta-analysis study supported the use of core-based exercise as a safe, conservative treatment, showing no adverse events to improve the QoL of people with scoliosis [38]. Furthermore, a review study conducted by Alanazi et al. also stated the effectiveness of core exercises in reducing pain and disability and improving the QoL in idiopathic scoliosis [46].
In the present study, the QoL was significantly improved in both groups. The CS group showed a remarkable difference in the post-treatment total and domain scores of the SRS-22 questionnaire, excluding the domain of mental health, which showed no difference between groups. The self-image and function domains did not significantly differ in the ASC group post-treatment in the ASC group. Results in this work were consistent with other reports, which also revealed a positive impact of variable non-invasive treatments on the QoL of scoliotic patients. A recent meta-analysis study supported the use of core-based exercise as a safe, conservative treatment, showing no adverse events to improve the QoL of people with scoliosis [38]. Furthermore, a review study conducted by Alanazi et al. also stated the effectiveness of core exercises in reducing pain and disability and improving the QoL in idiopathic scoliosis [46].
The results of SRS-22 in our work reflected the positive effect of CS on different domains influencing the patients’ QoL. The improved mental health could be related to the increased patient awareness of the disease, which can be actively achieved over time [47]. As the rationale behind each treatment program (CS and ASC) was not directly engaged in mental work, a reasonable interpretation of the similar results of both groups in this domain can be provided. The pain domain showed improvement in both groups, which was remarkable in the CS one. The improved pain and function domains in the CS group could be related to the neurophysiological and mechanical effects. CS exercises aim to improve the subject’s abilities to coordinate the muscle activities in isolation and during the performance of different functional functions activities. Generally, patients with back pain have overactive superficial spinal muscles and diminished activation of deep ones. Because the CS exercises enhance the coordination between superficial and deep spinal muscles, they can alter muscle performance and prevent and treat different musculoskeletal and spinal disorders. Following the CS program, increased back muscle endurance, spinal flexibility, and stability can directly reduce back impact reducing back pain [9,42]. Studies revealed the importance of improving back muscles endurance instead of strength in managing back pain [48,49]. The results of the pain domain in this study were convenient to other studies which reported the effect of CS on reducing pain in mild [11,47] and moderate [13] scoliotic curves. Based on the presented information, the obtained improvement in back endurance and spinal flexibility in an adolescent with a mild single scoliotic curve who participated in this work could explain the superior effect of CS to ASC on reducing pain in AIS.
The improved self-image and higher satisfaction rates in the CS group could be related to the improved spinal deformity, postural alignment, mobility, and stability reflected in function and the general aesthetics [47]. However, the ASC group in this work did not show any significant difference in self-image and function.
Contrary to our results, some studies reported no impact of the conservative treatment on QoL in patients with scoliosis [13]. The discrepancy in results between the present study and the others could be related to the application of different treatment protocols in which the patients were treated with a full-time application of a modified Boston brace and irregular physiotherapy for two years [50] instead of the active exercisen in this work. Another difference was the sample characteristics of a moderate scoliotic curve with a mean Cobb angle of 29.4° in Vasiliadis et al. instead of (18.76° ± 3.57°) and (19.06° ± 2.62°) in our study [50]. The work of Yagci et al. reported no significant difference between the two conservative programs; CS combined with bracing and SEAS on the QoL except for the pain domain, which only improved in the CS group. Yagci et al. conducted their study on subjects with moderate double scoliotic curves, which may explain the contradiction of their results to ours. However, their study's results obtained in the pain domain can support our results and prove the benefits of adding a CS program to scoliosis rehabilitation to effectively reduce pain [13].
Limitations
This study had some limitations. Firstly, the vertebral rotation was not measured in this work. Assessing vertebral rotation could provide a deeper explanation of the effect of the CS program on spinal deformity and could be recommended in future research. However, using the Cobb method in this work provided a valid and reliable measure for curve progression and spinal deformity. Secondly, patients’ compliance with the home program could not be fully guaranteed, although the patients’ video records were checked weekly. The long-term effects of the two programs were not evaluated in this work and would be recommended for further studies.
Conclusion
In the short-term treatment among adolescents with mild idiopathic scoliosis, core stabilization exercise was superior to the active-self correction program in improving the spinal deformity (Cobb angle), back muscle endurance, spinal flexibility, and quality of life.
Clinical Relevance
Improvements obtained in this study highlighted the importance of core stability and postural control assessment and treatment in the rehabilitation programs of adolescents with mild idiopathic scoliosis.
References
- Schlösser TP, van der Heijden GJ, Versteeg AL, et al. How 'idiopathic' is adolescent idiopathic scoliosis? A systematic review on associated abnormalities. PLoS One 2014 12; 9(5): e97461.
- Grivas TB, Vasiliadis E, Mouzakis V, et al. Association between adolescent idiopathic scoliosis prevalence and age at menarche in different geographic latitudes. Scoliosis 2006; 1:9. Published 2006 May 23.
- Negrini S, Donzelli S, Aulisa AG, et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord 2018; 13: 3.
- Fadzan M, Bettany-Saltikov J. Etiological theories of adolescent idiopathic scoliosis: Past and present. Open Orthop J 2017; 11: 1466-1489.
- Weinstein SL, Dolan LA, Cheng JC, et al. Adolescent idiopathic scoliosis. Lancet 2008; 371(9623): 1527-37.
- Lonstein JE. Scoliosis: Surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006; 443: 248-59.
- Wever DJ, Veldhuizen AG, Klein JP, et al. A biomechanical analysis of the vertebral and rib deformities in structural scoliosis. Eur Spine J 1999; 8(4): 252-60.
- Weiss HR. Physical therapy intervention studies on idiopathic scoliosis-review with the focus on inclusion criteria1. Scoliosis 2012; 7(1): 4.
- Akuthota V, Ferreiro A, Moore T, et al. Core stability exercise principles. Curr Sports Med Rep 2008; 7(1): 39-44.
- Vasseljen O, Unsgaard-Tøndel M, Westad C, et al. Effect of core stability exercises on feed-forward activation of deep abdominal muscles in chronic low back pain: A randomized controlled trial. Spine (Phila Pa 1976) 2012; 37(13): 1101-8.
- Gür G, Ayhan C, Yakut Y. The effectiveness of core stabilization exercise in adolescent idiopathic scoliosis: A randomized controlled trial. Prosthet Orthot Int 2017; 41(3): 303-310.
- Monticone M, Ambrosini E, Cazzaniga D, et al. Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J 2014; 23(6): 1204-14.
- Yagci G, Yakut Y. Core stabilization exercises versus scoliosis-specific exercises in moderate idiopathic scoliosis treatment. Prosthet Orthot Int 2019; 43(3): 301-308.
- Ko KJ, Kang SJ. Effects of 12-week core stabilization exercise on the Cobb angle and lumbar muscle strength of adolescents with idiopathic scoliosis. J Exerc Rehabil 2017; 13(2): 244-249.
- Zhou X, Li X, Wu Q, et al. Three-dimensional corrective exercise therapy for idiopathic scoliosis: Study protocol for a prospective non-randomized trial. BMC Musculoskelet Disord 2022; 23(1): 118.
- Negrini S, Donzelli S, Negrini A, et al. Specific exercises reduce the need for bracing in adolescents with idiopathic scoliosis: A practical clinical trial. Ann Phys Rehabil Med. 2019; 62(2): 69–76.
- Shin SS, Lee YW, Song CH. Effects of lumbar stabilization exercise on postural sway of patients with adolescent idiopathic scoliosis during quiet sitting. J Phys Ther Sci 2012; 24: 211–215.
- Kocaman H, Bek N, Kaya MH, et al. The effectiveness of two different exercise approaches in adolescent idiopathic scoliosis: A single-blind, randomized-controlled trial. PLoS One 2021; 16(4): e0249492.
- Negrini S, Zaina F, Romano M, et al. Specific exercises reduces brace prescription in adolescent idiopathic scoliosis: A prospective controlled cohort study with worst-case analysis. J Rehabil Med 2008; 40(6): 451-5.
- Pi?tek E, Kuczy?ski M, Ostrowska B. The effects of active self-correction on postural control in girls with adolescent idiopathic scoliosis: The role of an additional mental task. Int J Environ Res Public Health 2020; 17(5): 1640.
- Langensiepen S, Semler O, Sobottke R, et al. Measuring procedures to determine the Cobb angle in idiopathic scoliosis: A systematic review. Eur Spine J 2013; 22(11): 2360-71.
- Carman DL, Browne RH, Birch JG. Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. J Bone Joint Surg Am 1990; 72(3): 328-33.
- https://www.scirp.org/(S(i43dyn45teexjx455qlt3d2q))/reference/ReferencesPapers.aspx?ReferenceID=573326
- Knott P, Pappo E, Cameron M, et al. SOSORT 2012 consensus paper: Reducing x-ray exposure in pediatric patients with scoliosis. Scoliosis. 2014; 9: 4.
- Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine (Phila Pa 1976) 1984; 9(2): 106-19.
- Latimer J, Maher CG, Refshauge K, et al. The reliability and validity of the Biering-Sørensen test in asymptomatic subjects and subjects reporting current or previous nonspecific low back pain. Spine (Phila Pa 1976). 1999 Oct 15;24(20):2085-9; discussion 2090.
- Coorevits P, Danneels L, Cambier D, et al. Assessment of the validity of the Biering-Sørensen test for measuring back muscle fatigue based on EMG median frequency characteristics of back and hip muscles. J Electromyogr Kinesiol 2008; 18(6): 997-1005.
- Perret C, Poiraudeau S, Fermanian J, et al. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch Phys Med Rehabil 2001; 82(11): 1566-70.
- Norkin CC, White DJ. Measurement of joint motion: A guide to goniometry. (3rd edn). Philadelphia, Davis Company 2003.
- Asher M, Min Lai S, Burton D, et al. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976). 2003; 28(1): 63-9.
- Asher MA, Lai SM, Glattes RC, et al. Refinement of the SRS-22 health-related quality of life questionnaire function domain. Spine (Phila Pa 1976) 2006; 31(5): 593-7.
- Barr KP, Griggs M, Cadby T. Lumbar stabilization: A review of core concepts and current literature, part 2. Am J Phys Med Rehabil 2007; 86(1): 72-80.
- Muthukrishnan R, Shenoy SD, Jaspal SS, et al. The differential effects of core stabilization exercise regime and conventional physiotherapy regime on postural control parameters during perturbation in patients with movement and control impairment chronic low back pain. Sports Med Arthrosc Rehabil Ther Technol 2010; 2: 13.
- Chan YL, Cheng JC, Guo X, et al. MRI evaluation of multifidus muscles in adolescent idiopathic scoliosis. Pediatr Radiol. 1999; 29(5):360-3.
- Coulombe BJ, Games KE, Neil ER, et al. Core stability exercise versus general exercise for chronic low back pain. J Athl Train 2017; 52(1): 71-72.
- Negrini S, Aulisa AG, Aulisa L, et al. 2011 SOSORT guidelines: Orthopaedic and Rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2012; 7(1): 3.
- Akuthota V, Nadler SF. Core strengthening. Arch Phys Med Rehabil 2004; 85(3 Suppl 1): S86-92.
- Li X, Shen J, Liang J, et al. Effect of core-based exercise in people with scoliosis: A systematic review and meta-analysis. Clin Rehabil 2021; 35(5): 669-680.
- Park YH, Park YS, Lee YT, et al. The effect of a core exercise program on Cobb angle and back muscle activity in male students with functional scoliosis: A prospective, randomized, parallel-group, comparative study. J Int Med Res 2016; 44(3): 728-34.
- Wu HD, Wong MS. Assessment of maximum spinal deformity in scoliosis: A literature review. J Med Biol Eng 2020; 40, 621–629.
- Ebenbichler GR, Oddsson LI, Kollmitzer J, et al. Sensory-motor control of the lower back: Implications for rehabilitation. Med Sci Sports Exerc 2001; 33(11): 1889-98.
- Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am 2003; 34(2): 245-54.
- Wang XQ, Zheng JJ, Yu ZW, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS One 2012; 7(12): e52082.
- Fortin C, Feldman DE, Cheriet F, et al. Validity of a quantitative clinical measurement tool of trunk posture in idiopathic scoliosis. Spine (Phila Pa 1976). 2010; 35(19): E988-94.
- Komeili A, Westover L, Parent EC, et al. Monitoring for idiopathic scoliosis curve progression using surface topography asymmetry analysis of the torso in adolescents. Spine J 2015; 15(4): 743-51.
- Alanazi MH, Parent EC, Dennett E. Effect of stabilization exercise on back pain, disability and quality of life in adults with scoliosis: A systematic review. Eur J Phys Rehabil Med 2018; 54(5): 647-653.
- Monticone M, Ambrosini E, Cazzaniga D, et al. Adults with idiopathic scoliosis improve disability after motor and cognitive rehabilitation: Results of a randomised controlled trial. Eur Spine J 2016; 25(10): 3120-3129.
- McGill SM. Low back stability: From formal description to issues for performance and rehabilitation. Exerc Sport Sci Rev 2001; 29(1): 26-31.
- Geneen LJ, Moore RA, Clarke C, et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev 2017; 4(4): CD011279.
- Vasiliadis E, Grivas TB. Quality of life after conservative treatment of adolescent idiopathic scoliosis. Stud Health Technol Inform 2008; 135:409-13.