Research Article - Biomedical Research (2017) Volume 28, Issue 11
Efficacy of ATP-guided pulmonary vein isolation for atrial fibrillation: metaanalysis of evidence from randomized and non-randomized controlled trials
Yuanzheng Ye#, Xianhui Zhou#, Yaodong Li, Jianghua Zhang, Yanmei Lu, Qiang Xing, Qina Zhou, Ling Zhang, Wenhui Zhang, Wenkui Lv, Xinchun Cheng, Bingxin Chen, Baopeng Tang* and Yi Peng*
Heart Center, the First Affiliated Hospital of Xinjiang Medical University, Urumqi, PR China
#These authors contribute equally to this work
- *Corresponding Author:
- Baopeng Tang
Heart Center
The First Affiliated Hospital of Xinjiang Medical University, PR China
Yi Peng
Heart Center
The First Affiliated Hospital of Xinjiang Medical University, PR China
Accepted on March 30, 2017
Abstract
Aims: This study aims to systematically evaluate the efficacy of ATP guided Pulmonary Vein Isolation (PVI) for the treatment of paroxysmal Atrial Fibrillation (AF) and persistent AF.
Methods: A systematic search was performed on PubMed, EMbase, the Cochrane Library and Medline for Randomized Controlled Trial (RCT) and Non-Randomized Controlled Trials (Non-RCT) of ATP guided PVI treatment efficacy in AF patients until February 2016. RevMan 5.3 was used for metaanalysis.
Results: Finally, 3 RCTs and 9 non-RCTs were included. There was no difference in postoperative freedom from AF for paroxysmal AF patients in 2 non-RCTs; and no difference in postoperative freedom from AF for paroxysmal and persistent AF patients in 4 non-RCTs. The overall meta-analysis results showed that AF recurrence rate was higher in ATP group than that in conventional PVI group (P<0.05). Two RCTs showed no difference in postoperative recovery rate of pulmonary vein conduction between the two groups. For 1 year postoperative freedom from AF, 2 RCTs showed no difference between ATP guided and conventional PVI groups. However, 1 year postoperative freedom from AF was significantly higher in ATP guided PVI group than that in conventional PVI group in 4 non-RCTs (P<0.001). The overall meta-analysis results also showed that 1 year postoperative freedom from AF was significantly higher in ATP guided PVI group than that in conventional PVI group (P<0.01).
Conclusions: ATP is safe and effective in identification of occult conduction in PVI.
Keywords
Atrial fibrillation, ATP, Pulmonary vein isolation, Systematic review, Meta-analysis
Introduction
Atrial Fibrillation (AF) is the most common refractory arrhythmias. In Europe and United States AF treatment guidelines [1], catheter ablation treatment was recommended as first-line therapy for refractory AF. Pulmonary vein isolation (PVI) is the most widely used radiofrequency ablation treatment for AF [1]. Controlled clinical trials showed that PVI was more effective for AF patients [2,3] than that of drug therapy. However, the success rate of PVI is limited due to recovery of pulmonary vein conduction and second operation might be required for some patients [4,5].
Adenosine can identify occult pulmonary vein conduction [6]. Adenosine Triphosphate (ATP) is rapidly degraded into adenosine in human body, which can bind with the A1 receptor on atrial cardiomyocytes. This binding results in increased outward potassium currents on atrial cardiomyocytes and cell membrane hyperpolarization of atrial cardiomyocytes. The action potential duration and effective refractory period of atrial cardiomyocytes are shortened with prolonged vulnerability, which facilitates electricity conduction. Therefore, atrial arrhythmia could easily be induced, such as atrial premature beats and atrial fibrillation [7]. Recently, one Randomized Controlled Trial (RCT) showed that adenosine guided PVI was safe and effective [8]. However, two subsequent RCTs [9,10] showed that ATP guided PVI did not significantly improve the AF prognosis compared with that of conventional PVI. Therefore, this study systematically evaluated the efficacy of ATP guided PVI treatment for the paroxysmal and persistent AF in order to provide evidence for future surgical treatment selection.
Methods
Search strategy
A systematic search was performed on PubMed, EMbase, the Cochrane Library and Medline for RCT and Non-Randomized Controlled Trials (non-RCT) of ATP guided PVI treatment efficacy in AF patients until February 2016 using key words of “atrial fibrillation” AND (“adenosine” OR “ATP”) and “pulmonary vein isolation”. To reduce publication bias, all references of included studies were identified and reviewed.
Inclusion and exclusion criteria
The inclusion criteria were 1) clinical trials published in English; 2) adult patient with symptomatic or clinical diagnosed AF without surgical intervention; 3) ATP guided PVI as experiment group, conventional PVI as control group. The outcome measurements were 1) postoperative freedom from AF in patients with and without occult conduction; 2) postoperative pulmonary vein conduction recovery rate; 3) 1- year postoperative freedom from AF.
Exclusion criteria were 1) duplicate publications; 2) articles with incomplete results; 3) dissertations or reviews; 4) patients with ATP or antiarrhythmic drug intolerance, bronchial asthma, severe ischemic angina, persistent tachycardia, renal insufficiency, heart failure, left ventricular ejection fraction<40%, left atrial diameter>55 mm, acute myocardial infarction in the past 6 months, or severe heart valve disease.
Data substraction and evaluations
Two independent investigators were entrusted to screen the articles, extract information and evaluate study quality. The disagreement was resolved by discussion or a third investigator was involved. The following information was extracted: 1) general information, such as study name, authors’ name, publication date and trial site; 2) study general characteristics, such as the number of cases; 3) outcome measurements, such as treatment successful rate. The study quality was evaluated using Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [11] as following: 1) randomization method; 2) allocation concealment; 3) blinding for the patients as well as among the investigators; 4) assessment of the blinding implementation; 5) data integrity; 6) reporting integrity; and 7) other bias. All studies were evaluated as "Yes", "No", "unclear (N/A)" for the above criteria. Detailed randomization methods were described in the quality evaluation table.
Statistical analysis
RevMan 5.3 was used for meta-analysis. Quantitative data was expressed as Relative Risk (RR) and 95% Confidence Interval (CI). The Chi square test was used for study heterogeneity evaluation. If no heterogeneity was detected (P>0.1, I2<50%), fixed effects model was used; otherwise (P ≤ 0.1, I2 ≥ 50%), the heterogeneity factors were explored using subgroup analysis. If there was only statistical heterogeneity or method heterogeneity between the two study groups, random effect model was used. If the heterogeneity was significant (I2 ≥ 75%) or data source could not be identified, descriptive analysis was used. A P value less than 0.05 was considered as statistically significant.
Results
Characteristics of literature search and included studies
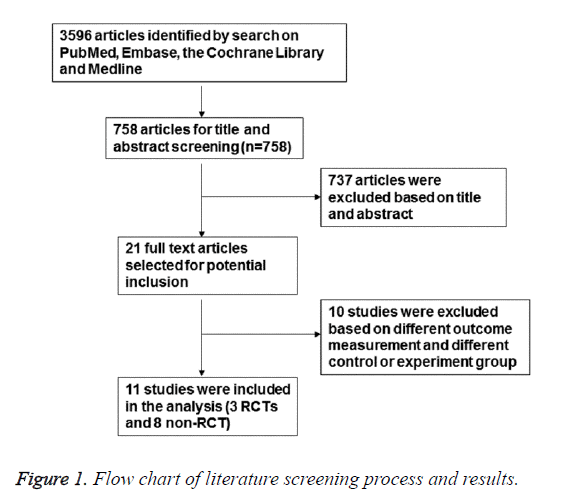
There were 3596 articles identified, and 758 remained after reviewing the titles and abstracts. After removing illegible studies, 11 studies were finally included [8-10,12-19]. The flowchart of screening process was shown in Figure 1.
The basic characteristics of the included studies and quality assessment
The basic characteristics of the included studies were shown in Table 1. The included studies were prospective RCTs, cohort studies and case control studies. Surgical procedures were ATP guided PVI and conventional PVI. AF types included paroxysmal AF and persistent AF. There were no differences in age between the groups, and follow up time ranged from 3 months to 1 year. The methodological quality evaluation results were shown in Table 2. Random number table or computer generated random numbers were used in 3 RCTs. However, the concealment grouping was not mentioned. Because that the treatment method was surgery, the blind method was not used.
| Article | Study type | Compared groups | AF Type | Age | N | Follow-Up | Freedom from AF |
|---|---|---|---|---|---|---|---|
| Macle [8] | Prospective randomized controlled trial | Dormant conduction | Paroxysmal AF | 58.4 ± 9.7 | 137 | 368 ± 43 d | 58 |
| No dormant conduction | 58.9 ± 10.9 | 115 | 64 | ||||
| Ghanbari [9] | Prospective randomized controlled trial | ATP given | Paroxysmal AF | 59.7 ± 8.7 | 61 | 278.6 ± 211.9 d | 59 |
| ATP not given | 58.9 ± 10.7 | 68 | 65 | ||||
| Kobori [10] | Prospective randomized controlled trial | ATP given | Paroxysmal AF+Persistent AF | 58.6 ± 8.6 | 737 | 330-450 d for 12 m | 641 |
| ATP not given | 68.5 ± 8.8 | 683 | 563 | ||||
| Gula [12] | Prospective cohort | Adenosine transient reconnection | Paroxysmal AF | 56.7 ± 9.2 | 25 | 12 m | 19 |
| No Adenosine transient reconnection | 47 | 35 | |||||
| Miyazaki [13] | Prospective cohort | ATP reconnection | Paroxysmal AF | 56.7 ± 9.2 | 39 | 12 m | 20 |
| No ATP reconnection | 61.4 ± 11.2 | 70 | 51 | ||||
| Arentz [14] | Prospective cohort | Adenosine-induced reconnection | Paroxysmal AF+Persistent AF | 54 ± 10 | 13 | 12 m | 5 |
| No adenosine reconnection | 16 | 7 | |||||
| Hachiya [15] | Retrospective cohort | ATP reconnection | Paroxysmal AF+Persistent AF | 56 ± 9 | 34 | 6.1 ± 3.3 | 23 |
| No ATP reconnection | 48 | 37 | |||||
| ATP not given | 54 ± 9 | 170 | 102 | ||||
| Matsuo [16] | Retrospective cohort | ATP dormant PV conduction | Paroxysmal AF+Persistent AF | 54.3 ± 9.6 | 139 | 29.7 ± 13.0 | 87 |
| No ATP dormant PV conduction | 54.2 ± 10.9 | 94 | 62 | ||||
| Tritto [17] | Prospective cohort | Adenosine-induced reconnection | Paroxysmal AF+Persistent AF | 55 ± 8 | 16 | 6.3 ± 2.4 | 11 |
| No adenosine reconnection | 13 | 9 | |||||
| Kumagai [18] | Retrospective cohort | ATP given | Paroxysmal AF+Persistent AF | 58 ± 11 | 106 | 16 ± 5.2 | 81 |
| ATP not given | 59 ± 10 | 106 | 16 ± 6.9 | 66 | |||
| Matsuo [19] | Retrospective cohort | ATP given | Paroxysmal AF+Persistent AF | 53.9 ± 9.1 | 54 | 19.9 ± 6 | 43 |
| ATP not given | 52.7 ± 10.1 | 94 | 56 | ||||
| Zhang [20] | Retrospective cohort | ATP given | Paroxysmal AF | 57.4 ± 6.3 | 39 | 6 m | 30 |
| ATP not given | 261 | 176 | |||||
| Note: AF: Atrial Fibrillation. | |||||||
Table 1. General characteristics of included studies.
| Included studies | Randomization method | Concealment | Blind method | Data integrity | Selective reporting of results | Other bias | |
|---|---|---|---|---|---|---|---|
| Patients and investigators | Evaluators | ||||||
| Macle [8] | Computer generated random numbers | N/A | No | No | Yes | Yes | N/A |
| Kobori [10] | Random number table | N/A | No | No | Yes | Yes | N/A |
| Ghanbari [9] | Random number table | N/A | No | No | Yes | Yes | N/A |
| Note: N/A indicates unclear. | |||||||
Table 2. The methodology quality evaluation.
The postoperative freedom from AF
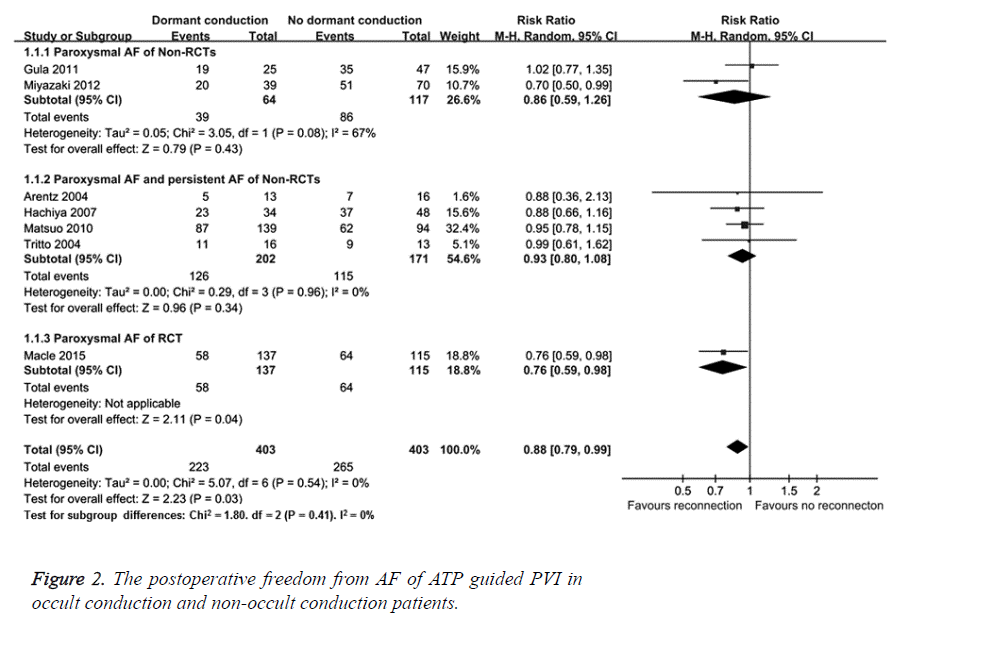
The postoperative freedom from AF in patients with and without occult conduction was analysed after ATP guided PVI. There were 6 non-RCTs [12-17] and one RCT [8] that reported the postoperative freedom from AF after ATP guided PVI for occult and non-occult conduction AF patients. Therefore, subgroup analysis was used based on study type and whether patients were with paroxysmal AF. Random effects model meta-analysis was conducted. As shown in Figure 2, two non- RCTs [12,13] showed that there were no significant differences in postoperative freedom from AF between occult and non-occult conduction AF patients with paroxysmal AF (RR=0.86, 95% CI (0.59, 1.26), P=0.43). Four non-RCTs [14-17] showed that there were no significant differences in postoperative freedom from AF between occult and non-occult conduction AF patients with persistent and paroxysmal AF between the two groups (RR=0.93, 95% CI (0.80, 1.08), P=0.34). However, one RCT [8] showed that the postoperative AF recurrence rate of ATP guided PVI was higher in occult conduction group compared with that in non-occult conduction group (RR=0.76, 95% CI (0.59, 0.98), P=0.04). The overall result showed that the postoperative AF recurrence rate of ATP guided PVI group was higher compared with that of conventional PVI group (RR=0.88, 95% CI (0.79, 0.99), P=0.03), indicating that ATP is effective in identification of occult conduction.
Postoperative recovery rate of pulmonary vein conduction
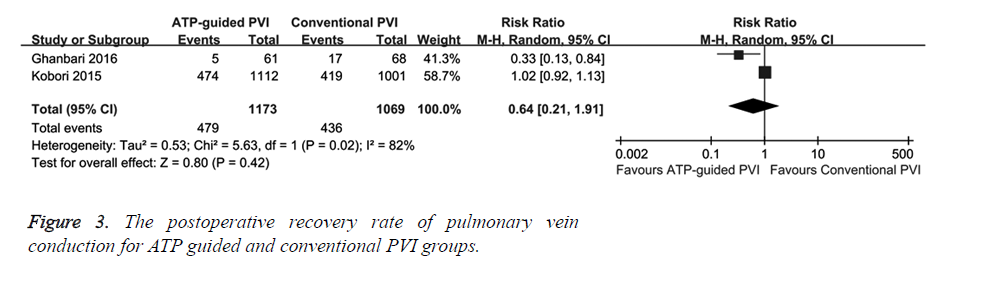
The effect of ATP guided PVI and conventional PVI on postoperative recovery rate of pulmonary vein conduction was evaluated. Two RCTs reported the postoperative recovery rate of pulmonary vein conduction and it showed that there was no significant difference between ATP guided and conventional PVI groups (RR=0.64, 95% CI (0.21, 1.91), P=0.42) (Figure 3). This result indicates that ATP has no obvious effect on pulmonary vein conduction recovery.
The 1-year postoperative freedom from AF
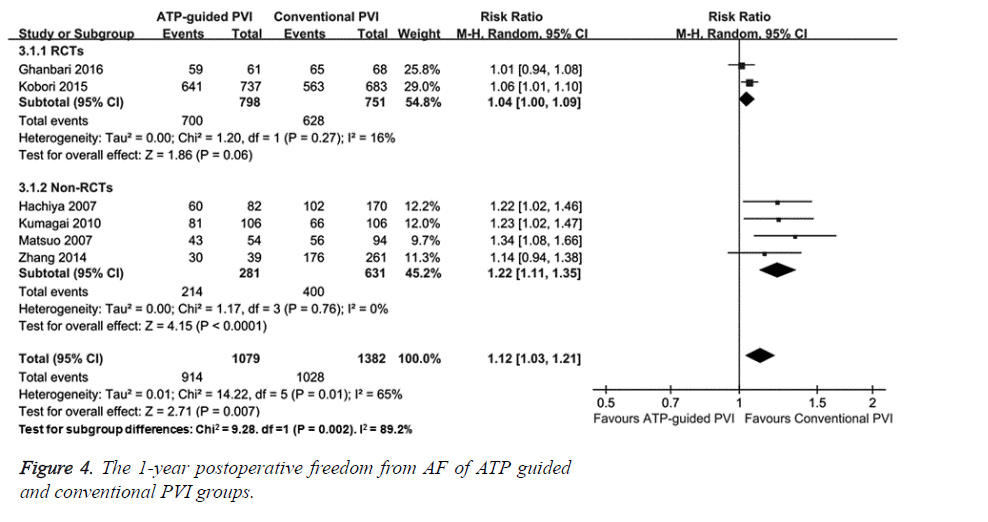
To determine the efficacy of ATP guided PVI and conventional PVI, AF patients were followed up for 1 year and 1-year postoperative freedom from AF was observed. Two RCTs [9,10] showed that there was no significant difference in 1 year postoperative freedom from AF between ATP guided and conventional PVI groups (RR=1.04, 95% CI (1.00, 1.09), P=0.27) (Figure 4). Four non-RCTs [15,18-20] showed that postoperative freedom from AF was higher in ATP guided PVI group than that in conventional PVI group (RR=1.22, 95% CI (1.11, 1.35), P<0.0001). The overall meta-analysis results demonstrated that ATP guided PVI group had higher postoperative freedom from AF than conventional PVI group (RR=1.12, 95% CI (1.02, 1.22), P=0.01). This data suggests that ATP guided PVI has better efficacy than conventional PVI.
Discussion
PVI is only suitable for 85% to 90% of the paroxysmal AF with 35% to 45% second operation rate [2,21]. The most common reason for recurrent AF is the restoration of electrical conduction between the atrium and the pulmonary vein [20,22]. And, ATP can detect the occult pulmonary vein conduction [20,23]. A few non-RCTs [20,22] and one meta-analysis [23] have reported that ATP guided PVI may reduce the atrial arrhythmia recurrence for AF patients. One RCT [8] also showed that ATP could detect occult pulmonary vein conduction and subsequent re-dissection vein catheter ablation could improve the prognosis of AF.
The 6 non-RCTs [12-17] and one RCT [8] included in this study analysed the postoperative freedom from AF after ATP guided PVI in AF patients with occult and non-occult conduction. Two non-RCTs [12,13] showed that there were no significant differences in postoperative freedom from AF between occult and non-occult conduction groups for paroxysmal AF patients. Four non-RCTs [14-17] showed that there were no significant differences in postoperative freedom from AF between occult and non-occult conduction groups for paroxysmal and persistent AF patients. However, one RCT [8] showed that the postoperative AF recurrence rate of ATP guided PVI was higher in occult conduction group compared with that in non-occult conduction group. The overall meta-analysis result showed that the AF recurrence rate was higher in ATP guided PVI group compared with that of conventional PVI group. Our result was inconsistent with the meta-analysis results of non-RCTs. This inconsistence may result from the inclusion of RCTs, which is of fewer biases, more mature techniques and more reliable results. Therefore, this study suggests that ATP is effective for identification of occult pulmonary vein conduction and can improve the AF prognosis.
However, a subsequent large RCT [10] questioned the ATP detection technique. The 2113 patients were randomly assigned to ATP group and control group, and there was no significant difference of postoperative AF recurrence rate between the two groups after the 1-year follow-up [10]. This was in line with Ghanbari’s [9] research on ATP’s detection of occult pulmonary vein conduction. Because of the different results among RCTs and non-RCTs, subgroup analysis was used in this study. Two RCT [9,10] showed there was no significant difference in postoperative AF recurrence rate between ATP guided PVI group and conventional PVI group, while 3 non- RCTs [15,18,19] showed the AF prognosis was better in ATP group compared with that in conventional PVI group. Overall, the AF prognosis was better in ATP group compared with that in conventional PVI group with high heterogeneity (I2=71%). The heterogeneity may result from the different study design of RCTs and non-RCTs. The 3 non-RCTs [15,18,19] were all retrospective studies with selection bias for patients as well as for operators. ATP guided PVIs might all have been performed by more experienced operators. Another non-RCT [20] showed that there was no difference between the two groups, however, the atrial arrhythmia recurrence rate was significantly lower in ATP group receiving the second operation, compared with that of control group. In addition, the two recent RCTs [9,10] may have better surgical techniques and may reduce the selection bias in non-RCTs. Last but not least, the observation time of spontaneous recovery of pulmonary vein conduction, which is essential in identification of acute pulmonary vein conduction, is longer in RCTs. During the 1-year follow-up, the AF record is also inaccurate in that the follow-up is based on self-reported symptoms or 24 h ambulatory monitoring or phone call.
One RCT [8] showed that ATP detection of occult conduction might be routinely used for PVI with high safety and efficacy. However, its low postoperative AF recurrence rate was resulted from the second operation with no direct comparison with patients without ATP guided PVI. Two RCTs [9,10] showed no significant difference between the two groups for postoperative atrial arrhythmia recurrence rate.
This study is limited in the small number of RCTs and the bias in non-RCTs. Further RCTs with less selection bias and more objective follow-ups are needed. Our results showed that the AF prognosis was better in ATP guided PVI group. Therefore, overall, ATP is safe and effective in identification of occult conduction in PVI, however, whether ATP guided PVI could improve the AF prognosis requires further assessment.
Acknowledgements
None
Conflict of Interest
The authors declare no conflict of interests.
References
- Mugnai G, Chierchia GB, de Asmundis C, Sieira-Moret J, Conte G, Capulzini L, Wauters K, Rodriguez-Mañero M, Di Giovanni G, Baltogiannis G, Ciconte G, Saitoh Y, Julia J, Brugada P. Comparison of pulmonary vein isolation using cryoballoon versus conventional radiofrequency for paroxysmal atrial fibrillation. Am J Cardiol 2014; 113: 1509-1513.
- Wilber DJ, Pappone C, Neuzil P, De Paola A, Marchlinski F, Natale A, Macle L, Daoud EG, Calkins H, Hall B, Reddy V, Augello G, Reynolds MR, Vinekar C, Liu CY, Berry SM, Berry DA, ThermoCool AF Trial Investigators. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA 2010; 303: 333-340.
- Morillo CA, Verma A, Connolly SJ, Kuck KH, Nair GM, Champagne J, Sterns LD, Beresh H, Healey JS, Natale A. Radio frequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): a randomized trial. JAMA 2014; 311: 692-700.
- Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, Klein G, Natale A, Packer D, Skanes A, Ambrogi F, Biganzoli E. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol 2010; 3: 32-38.
- Ouyang F, Antz M, Ernst S, Hachiya H, Mavrakis H, Deger FT, Schaumann A, Chun J, Falk P, Hennig D, Liu X, Bansch D, Kuck KH. Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation 2005; 111: 127-135.
- Datino T, Macle L, Qi XY, Maguy A, Comtois P, Chartier D, Guerra PG, Arenal A, Fernandez-Aviles F, Nattel S. Mechanisms by which adenosine restores conduction in dormant canine pulmonary veins. Circulation 2010; 121: 963-972.
- Ren FX, Guo JH. Research progress on cardiac electrophysiology of adenosine triphosphate and adenosine. Zhong Hua Xin Lv Shi Chang Za Zhi 2000; 4: 155-157.
- Macle L, Khairy P, Weerasooriya R, Novak P, Verma A, Willems S, Arentz T, Deisenhofer I, Veenhuyzen G, Scavee C, Jais P, Puererfellner H, Levesque S, Andrade JG, Rivard L, Guerra PG, Dubuc M, Thibault B, Talajic M, Roy D, Nattel S, ADVICE trial investigators. Adenosine-guided pulmonary vein isolation for the treatment of paroxysmal atrial fibrillation: an international, multicentre, randomized superiority trial. Lancet 2015; 9994: 672-679.
- Ghanbari H, Jani R, Hussain-Amin A, Al-Assad W, Huether E, Ansari S, Jongnarangsin K, Crawford T, Latchamsetty R, Bogun F, Morady F, Oral H, Chugh A. Role of adenosine after antral pulmonary vein isolation of paroxysmal atrial fibrillation: Arandomized controlled trial. Heart Rhythm 2016; 13: 407-415.
- Kobori A, Shizuta S, Inoue K, Kaitani K, Morimoto T, Nakazawa Y, Ozawa T, Kurotobi T, Morishima I, Miura F, Watanabe T, Masuda M, Naito M, Fujimoto H, Nishida T, Furukawa Y, Shirayama T, Tanaka M, Okajima K, Yao T, Egami Y, Satomi K, Noda T, Miyamoto K, Haruna T, Kawaji T, Yoshizawa T, Toyota T, Yahata M, Nakai K, Sugiyama H, Higashi Y, Ito M, Horie M, Kusano KF, Shimizu W, Kamakura S, Kimura T. Adenosine triphosphate-guided pulmonary vein isolation for atrial fibrillation: the UNmasking Dormant Electrical Reconduction by Adenosine TriPhosphate (UNDER-ATP) trial. Eur Heart J 2015 7; 36: 3276-3387.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration 2011
- Gula LJ, Massel D, Leong-Sit P, Gray C, Fox DJ, Segal OR, Krahn AD, Yee R, Klein GJ, Skanes AC. Does adenosine response predict clinical recurrence of atrial fibrillation after pulmonary vein isolation? J Cardiovasc Electrophysiol 2011; 22: 982-986.
- Miyazaki S, Kuwahara T, Kobori A, Takahashi Y, Takei A, Sato A, Isobe M, Takahashi A. Impact of adenosine-provoked acute dormant pulmonary vein conduction on recurrence of atrial fibrillation. J Cardiovasc Electrophysiol 2012; 23: 256-260.
- Arentz T, Macle L, Kalusche D, HociniM, Jais P, Shah D, Haissaguerre M. Dormant pulmonary vein conduction revealed by adenosine after ostial radiofrequency catheter ablation. J Cardiovasc Electrophysiol 2004; 15: 1041-1047.
- Hachiya H, Hirao K, Takahashi A, Nagata Y, Suzuki K, Maeda S, Sasaki T, Kawabata M, Isobe M, Iesaka Y. Clinical implications of reconnection between the left atrium and isolated pulmonary veins provoked by adenosine triphosphate after extensive encircling pulmonary vein isolation. J Cardiovasc Electrophysiol 2007; 18: 392-398.
- Matsuo S, Yamane T, Date T, Hioki M, Ito K, Narui R, Tanigawa S, Nakane T, Hama Y, Tokuda M, Yamashita S, Aramaki Y, Inada K, Shibayama K, Miyanaga S, Yoshida H, Miyazaki H, Abe K, Sugimoto K, Taniguchi I, Yoshimura M. Comparison of the clinical outcome after pulmonary vein isolation based on the appearance of adenosine induced dormant pulmonary vein conduction. Am Heart J 2010; 160: 337-345.
- Tritto M, De Ponti R, Salerno-Uriarte JA, Spadacini G, Marazzi R, Moretti P, Lanzotti M. Adenosine restores atrio-venous conduction after apparently successful ostial isolation of the pulmonary veins. Eur Heart J 2004; 25: 2155-2163.
- Kumagai K, Naito S, Nakamura K, Hayashi T, Fukazawa R, Sato C, Takemura N, Miki Y, Fuke E, Tanaka Y, Hori Y, Goto K, Iwamoto J, Aonuma K, Oshima S, Taniguchi K. ATP-induced dormant pulmonary veins originating from the carina region after circumferential pulmonary vein isolation of atrial fibrillation. J Cardiovasc Electrophysiol 2010; 21: 494-500.
- Matsuo S, Yamane T, Date T, Inada K, Kanzaki Y, Tokuda M, Shibayama K, Miyanaga S, Miyazaki H, Sugimoto K, Mochizuki S. Reduction of AF recurrence after pulmonary vein isolation by eliminating ATP-induced transient venous re-conduction. J Cardiovasc Electrophysiol 2007; 18: 704-708.
- Zhang J, Tang C, Zhang Y, Su X. Origin and ablation of the adenosine triphosphate induced atrial fibrillation after circumferential pulmonary vein isolation: effects on procedural success rate. J Cardiovasc Electrophysiol 2014; 25: 364-370.
- Calkins H, Reynolds MR, Spector P, Sondhi M, Xu Y, Martin A, Williams CJ, Sledge I. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol 2009; 2: 349-361.
- Miyazaki S, Kobori A, Hocini M, Shah AJ, Komatsu Y, Taniguchi H, Kusa S, Uchiyama T, Nakamura H, Hachiya H, Isobe M, Hirao K, Haissaguerre M, Takahashi A, Iesaka Y. Clinical utility of adenosine-infusion test at repeat atrial fibrillation ablation procedure. Heart Rhythm 2013; 10: 629-635.
- McLellan AJ, Kumar S, Smith C, Morton JB, Kalman JM, Kistler PM. The role of adenosine following pulmonary vein isolation in patients undergoing catheter ablation for atrial fibrillation: a systematic review. J Cardiovasc Electrophysiol 2013; 24: 742-751.