Research Article - Research and Reports in Gynecology and Obstetrics (2017) Research and Reports in Gynecology and Obstetrics (Special Issue 4-2017)
Effects of uterus-preserving surgical modalities on sexual functions in total prolapsus cases
Hasan Ç?lg?n*
Obstetric and Gynecology Department, Kafkas University, Kars, Turkey
- *Corresponding Author:
- Hasan Ç?lg?n
Obstetric and Gynecology Department
Kafkas University
Kars
Turkey
Tel: +905332279980
E-mail: munzurluhasan@yahoo.com
Accepted Date: November 22, 2017
Citation: Ç?lg?n H. Effects of uterus-preserving surgical modalities on sexual functions in total prolapsus cases. Res Rep Gynaecol Obstet. 2017;1(4):14-19
Abstract
Object?ve: To investigate sexual quality of life in uterine prolapse patients treated with hysteropexy while preserving the uterus in premenopausal period.
Materials and methods: This retrospective cohort study was conducted on 124 sexually active women whose age was between 30 and 45 and who were operated for prolapse by vaginal, abdominal, laparoscopic repair methods while preserving the uterus between May 2011 and April 2017. Women who willing to participate in the study, were filled an information form inquiring socio-demographic characteristics and Sexual Quality of Life Questionnaire-Female (SQLQ-F). Face-to-face survey method was used to assess the patient's satisfaction. Success was defined as prolapse below than stage 2, healing in preoperative symptoms, sexual relationship and post-operative pregnancy rate.
Results: One hundred and twenty four patients with pelvic organ prolapse stage 2-3 were included. The face-to-face questionnaire was conducted post-operatively 24 ± 9 months on average and quality of sexual life in the last six weeks were evulated by Sexual Quality of Life Questionnaire- Female (SQLQ-F). The SQLQ-F score of laparoscopic sacrohysteropexy was found higher than laparotomy and Sacrospinous ligament hysteropexy (p=0.011). There was found significantly difference in presence of vaginal dryness and dyspareunia among abdominal and vaginal way (p<0.001). The SQLQ-F score in women who had vaginal dryness was found lower than women who had not vaginal dryness in all surgical procedures, but significantly difference was only found in laparoscopic sacrohysteropexy group (p=0.027). There was no significantly difference found in the SQLQ-F score in women with and without dyspareunia according to the surgical procedures (p>0.05).
Conclus?ons: Sexual quality of life in laparoscopic hysteropexy is better than laparotomy and vaginal procedure. Vaginal dryness in vaginal hysteropexy negatively effects sexual quality of life. Uterus preservation options should be discussed with every premenopausal and sexually active patient before surgery for pelvic organ prolapse.
Keywords
Hysteropexy, Pelvic organ prolapse, Uterine preservation, Sexual quality of life
Introduction
Pelvic organ prolapse (POP) is a definition of anatomical change. Some such changes may well be considered within the range of normality for certain women. A diagnosis of POP ideally demands clear clinical evidence, starting with a woman having symptoms related to the “downward displacement” of a pelvic organ [1]. POP has significant negative impact on the quality of life, including physical discomfort, sexual and psychological problems and embarrassment. The estimated prevalence of any degree of genital prolapse in women between 20 and 59 years is about 30% [2]. The lifetime risk of undergoing surgery for pelvic organ prolapse is estimated to be about 11% and around 30% will undergo repeat surgery for a recurrence of the prolapse [3].
The goals of surgery for POP include restoration of normal anatomy, to maintain or restore urinary, bowel and sexual functions and to improve quality of life. The traditional treatment for uterine prolapse has been the vaginal hysterectomy, even in the absence of uterine disease. Hysterectomy alone does not address the deficiencies in pelvic support and does not correct the underlying pathophysiology, hence the higher incidence of recurrence and vault prolapse [4,5]. Hysterectomy also leads to unnecessary removal of a healthy organ with associated increased morbidity, blood loss and operating time [6,7]. Uterine conservation is important for women who wish to preserve fertility and is seemingly associated with improvements in sexuality, confidence and self-esteem of women [8]. Women may also request preservation of the uterus due to personal beliefs or to retain a sense of identity [9], hence recently there has been much interest in preserving the uterus during prolapse surgery [10] and an increasing number of women are requesting uterine conservation [11].
The World Health Organization defines sexual health as "the enrichment and empowerment of personality, communication, and affection in a positive way through the consideration of sexual life as physical, spiritual, mental, and social as a whole [12].
Although sexuality is not a vital necessity for sustaining one's individual existence, it is important for the individual to increase the quality of life. Sexual well-being is defined as the presence of general well-being in sexual functioning and satisfaction with sexual functioning. Changes that occur with prolapse can affect the quality of sexual life by affecting female sexual health. Together with prolapse, the female body image may be negatively affected and may also lose interest in sexuality with respect to the ending of feminine functions. The bodily factors affecting the quality of sexual life are related to the changes in one's body [13].
The most studied approaches to hysteropexy are the vaginal sacrospinous ligament hysteropexy and the abdominal sacrohysteropexy, which have similar objective and subjective prolapse outcomes compared with hysterectomy and apical suspension. Pregnancy and delivery have been documented after vaginal and abdominal hysteropexy approaches.
The objectives of this article were to explore anatomic and functional outcomes and to investigate the quality of sexual life in women undergoing hysteropexy by any surgical method.
Material and Methods
124 patients who underwent uterine preservation surgery for pelvic organ prolapse between january 2011 and april 2017 were included in the study. Before operation, Papanicolaou smear were obtained from all women and women with a normal uterus as documented by a pelvic examination and routine endometrial sampling can undergo conservation of the uterus as part of the prolapse repair, assuming the risks and benefits of hysteropexy. Before studying, hormone assays were performed to demonstrate that the patients were in the premenopausal period. Hysteropexy have been carefully reviewed by the physician and patient and the patient gives informed consent. Before the data was collected, the purpose of investigating was explained to the participant and informed consent was obtained. Only volunteers were included in the study. Information was provided on the fact that the data will be kept confidential and used only for scientific purposes, when they were uncomfortable with the questions, they could give up filling the information form, and they should not write the name-surname on the information forms. Patients operated for prolapse were called by phone between April and July 2017 and control examinations were performed. In abdominal pathway applications after entering the wrist; the peritoneum was opened over the sacral promontory and right pelvic sidewall between the ureter and rectum toward the pouch of Douglas. Each broad ligament at the level of the cervicouterine junction was also opened through the avascular area and the bladder dissected distally. Then, in laparotomy procedure uterus was suspended from the sacral promontory using a bifurcated polypropylene type-1 monofilament macroporous non-absorbable mesh (Ethicon, USA), which, prior to sacral fixation, was wrapped around the cervix, via the broad ligament windows created. The two arms of the mesh were transfixed anterior to the cervix with three non-absorbable polyester 2-0 sutures (Ethibond ExcelTM; Ethicon). In laparoscopic procedure; anterior peritoneum in the cervico-isthmic region was dissected and 5 mm of Mersilene tape (Ethicon, USA) was tightly fastened to the front of the myometrium in the cervicoismic area without uterine vessels dissipating laterally. The sacrospinous hysteropexy was preformed unilaterally, in all cases to the right ligament. Two non-absorbable Polypropylene Sutures (Prolene 1 Ethicon, USA) were placed through the sacrospinous ligament and the posterior side of the cervix. For evulating patients sexual satisfaction Sexual Quality of Life Questionnaire-Female (SQLQ-F),developed by Symonds et al. in 2005 were used [14]. In the six likert type, each item of the 18-item scale is answered by considering the quality of sexual life in the last six weeks. In the study 1 to 6 points system (1=Totally agree, 2=I agree in a big way, 3=Partially agree, 4=Partially disagree, 5=Strongly disagree, 6=Never agree) was used. Before the total score was calculated, points 1st, 5th, 9th, 13th, 18th were reversed and the total score from the scale was converted to 100. The high score on the scale indicates that the quality of sexual life is good. In order to assess in isolation the effects of the hysteropexy on the quality of the sexual life the cases with concomitant vaginal surgery were excluded.
Patients who have current or past concomitant medical conditions including depression, irritable bowel syndrome, hypertension, endometriosis, pelvic inflammatory disease, angina, diabetes, multiple sclerosis, underwent additional surgery during the hysteropexy and have not completed fifteen months after surgery and with stage IV uterovaginal prolapse or cervical elongation were excluded. A total of 18 cases were excluded from the study because 14 of them had additional surgical modalities in addition to hysteropexy, and 4 of them did not reach the 15-month follow-up period.
The study was approved by the hospital’s Research and Ethics Committee (80576354-050-99/53, 01/03/2017). The data were analyzed for those who had completed at least fifteen months follow-up and patient satisfaction was measured by the Patient Global Impression of Improvement (PGI-I). The calculation of aggregated results is based on objective outcome measures.
Statistical analysis
The process involved descriptive statistics and the descriptive data were presented as mean ± standard deviation, median and ratio. In evaluating the data; single sample Kolmogorov Smirnov test for normal distribution suitability of quantitative variables, Kruskal Wallis Test was used for comparison of SQLQ-F scores between surgical modalities. Non-parametric Mann-Whitney U test was used to compare the mean of the data among the groups. P<0.05 was considered significant. Statistical Package for Social Sciences (SPSS) for Windows 20 (SPSS for Windows, SPSS, Chicago) was used for statistical analysis.
Results
During the study period of 6 years, there were a total of 142 pelvic organ prolapse cases diagnosed and treated by any modality of hysteropexy in premenopausal period for uterus protective surgery in our university hospital and 124 cases were eligible for study. The mean age and BMI of patients were 38 ± 6.3 and 27.1 ± 4.3 respectively. It was determined that the vast majority of patients did not use cigarettes (82.4%) and alcohol (96.8%).
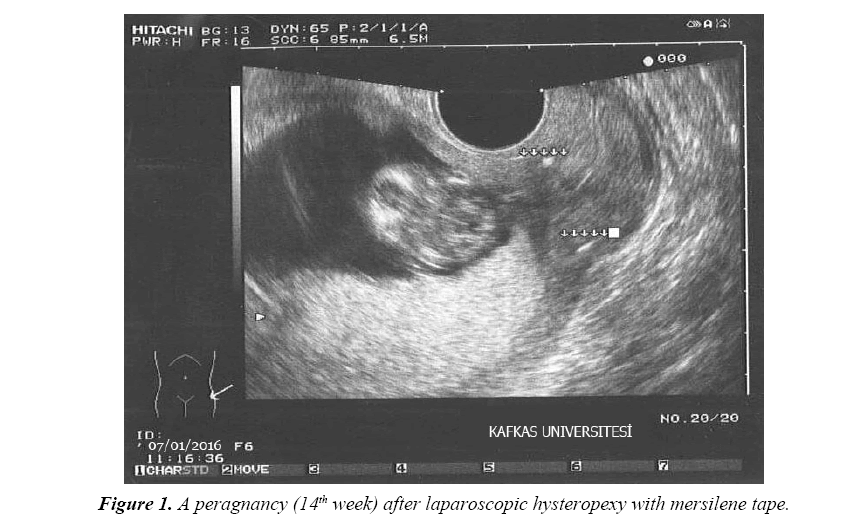
Twelve patients had a pregnancy after operation in average of 24+9 month follow-up. Seven were in laparoscopic, two were in laparoscopic sacrohysteropexy and three were in sacrospinous hysteropexy. The average birth week was 34.4 ± 5. In 88.9% of cases, pregnancy reached 34 weeks and over. Intrauterine mort fetus was detected at 29th week in one of the cases, where mesh was used for hysteropexy (in laparotomy group). All patients who were pregnant after surgery, required delivery by scheduled caesarean section. The mesh around the cervix is comparable with abdominal cervical cerclage and cervical dilatation would be impossible in labour. Although potential difficulty with caesarean section due to mesh was a concern, a well formed lower segment had developed above the mesh (Table 1 and Figure 1).
Table 1. Rate of the laparoscopic, abdominal, vaginal procedure and success of pregnancy.
| Surgical method | Number (n=124) | % | Number (n=124) | % | Pregnancy number (n=124) | % | |
|---|---|---|---|---|---|---|---|
| Abdominal (sacrohysteropexy) | 86 | 69.4 | laparoscopic | 52 | 42 | 7 | 13.5 |
| laparotomy | 34 | 27.4 | 2 | 5.8 | |||
| Vaginal | 38 | 30.6 | sacrospinous hysteropexy | 38 | 30.6 | 3 | 7.8 |
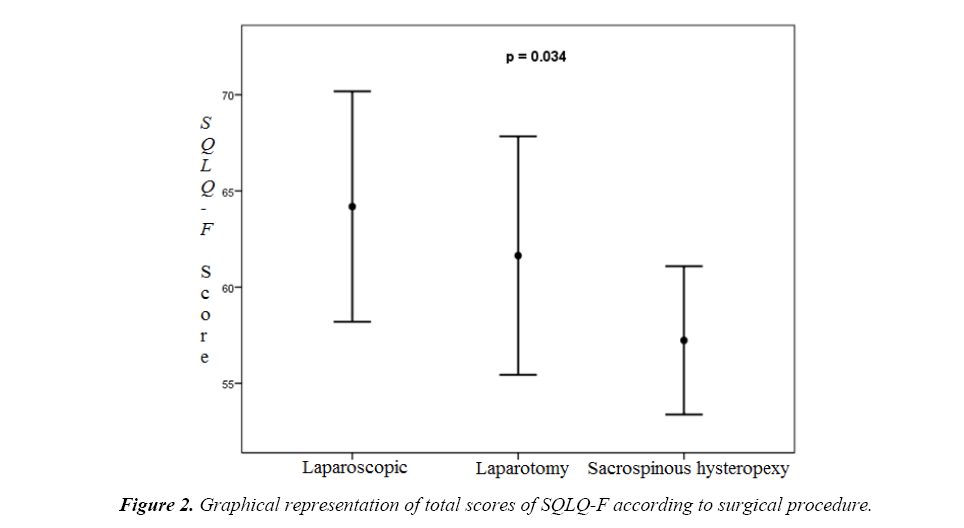
There was a statistically significant difference in the total score of SQLQ-F between the surgical procedures (p=0.034). laparoscopic hysteropexy SQLQ-F total score was higher than sacrospinous hysteropexy (p=0.011). There was no significant difference between laparoscopic hysteropexy and laparotomy hysteropexy (p=0.220) and between laparotomy hysteropexy and sacrospinous hysteropexy (p=0.322) ( Table 2 and Figure 2).
Table 2. Comparisons of age and total score of SQLQ-F between surgical procedure.
| Laparoscopic (n=52) | Laparotomy (n=34) | Sacrospinous hysteropexy (n=38) | p | |
|---|---|---|---|---|
| Age | 37.9 ± 6.2 | 38.2 ± 6.5 | 37.7 ± 6.1 | 0.837 |
| SQLQ-F total score | 65.2 ± 23 | 62.7 ± 16.1 | 58.3 ± 18.1 | 0.034 |
(Mean ± standard deviation, statistically significant P <0.05) (n: number of cases)
There was a significant difference in terms of the presence of vaginal dryness among the surgical procedures in the study (p<0.001). According to this, the most severe vaginal dryness complaint was experienced in sacrospinous hysteropexy. There was a significant difference between the surgical procedures in terms of the presence of dyspareunia (p<0.001). According to this, the most severe dyspareunia complaint was experienced in sacrospinous hysteropexy procedure (Table 3).
Table 3. Comparison of the presence of vaginal dryness and dyspareunia between surgical procedures.
| Total | Laparoscopic (n=52) | Laparotomy (n=34) | Sacrospinous hysteropexy (n=38) | p | ||
|---|---|---|---|---|---|---|
| Vaginal dryness complaint | No | 76 (61.3%) | 44 (84.6%) | 21 (61.7%) | 20 (52.6%) | <0.001 |
| Yes | 48 (38.7%) | 8 (15.4%) | 13 (38.2%) | 18 (47.4%) | ||
| Dyspareunia complaint | No | 72 (58.1%) | 43 (82.7%) | 16 (47.0%) | 16 (42.1%) | <0.001 |
| Yes | 52 (41.9%) | 9 (17.3%) | 18 (53.0%) | 22 (57.9%) | ||
(Mean ± standard deviation, statistically significant P <0.05) (n: number of cases)
When we look at the comparison of the total score of SQLQ-F between the presence of vaginal dryness and the surgical procedures, it was determined that those who complained of vaginal dryness had a lower total score of SQLQ-F. However, there was a significant difference only in sacrospinous hysteropexy group (p=0.027).
When we look at the comparison of SQLQ-F total score between the presence of dyspareunia and surgical procedures; it was observed that those with dyspareunia complaints had a lower total score of SQLQ-F. However, no significant difference was found between surgical procedures (p>0.05) (Table 4).
Table 4. Comparison of the presence of vaginal dryness and dyspareunia between the surgical procedures and the total score of the SQLQ-F.
| SQLQ-F Total score | Vaginal dryness complaint | Dyspareunia complaint | ||||
|---|---|---|---|---|---|---|
| No | Yes | p | No | Yes | p | |
| Laparoscopic | 65.0 ± 23.4 | 61.2 ± 20.5 | 0.340 | 65.5 ± 23.1 | 64.0 ± 21.2 | 0.673 |
| Laparotomy | 66.2 ± 19.3 | 59.0 ± 16.6 | 0.178 | 59.0 ± 16.6 | 58.9 ± 17.7 | 0.955 |
| Sacrospinous hysteropexy | 61.1 ± 21.2 | 54.1 ± 17.5 | 0.027 | 57.7± 24.7 | 54.2 ± 17.5 | 0.415 |
(Mean ± standard deviation, statistically significant P <0.05) (n: number of cases)
No major intra-or post-operative complication occurred. Success rate of the laparoscopic, abdominal, vaginal procedure aimed to repair uterine prolapse was 88.4% (46/52), 88.2% (30/34), 86.8% (33/38) respectively with mean point C at -6 to -7 (range (-1)-(-9)). So our total success rate was 87.9%. 15 patients (12.1% of women) who underwent any uterine conservative surgery for a mean follow-up of 24 months postoperatively had uterine descensus of Pelvic Organ Prolapse Quantification System (POP-Q) stage II or greater. Seven patients with recurrence of prolapse who have symptoms of prolapse needed further surgery to treat the recurrence (4.7% of women). Ninety-two percent of women were satisfied with the decision to preserve their uterus.
Discussion
Today, most women with POP prefer uterine sparing surgery due to the changes in lifestyle, beliefs, pregnancy desire, and understanding the role of the uterus and cervix in sexual function. Therefore, the need for newer surgical procedures that involve less invasive surgery, reduced intraoperative and postoperative risks, and a faster healing time in POP surgery have gained importance. Vaginal, abdominal, laparoscopic, and robotic methods are defined in uterine preserving surgery but there is not yet a consensus on which of them should be chosen. In choosing the proper technique, the patient's general status, accompanying disease, correct indication, and the surgeon's experience are all important.
The aims of surgery for POP comprise restoration of normal anatomy, to sustain or restore urinary, bowel and sexual functions and to improve quality of life. Conservative treatment of uterovaginal prolapse (observation, pessary or pelvic floor physical therapy) in women with uterovaginal prolapse should be the first-line treatment for women planning an attempted pregnancy. However, hysteropexy can be considered in women who have severe prolapse or whose symptoms can not be corrected by conservative treatment.
Hysterectomy applied surgical methods have negative effects on uterine contractions, change of orgasm perception, vaginal shortening, injury of nerve endings and sexual function, as well as disrupting women's self-esteem or the psychology of women due to loss of woman's feelings [15]. The protection of the uterus in POP surgery have been shown to contribute positively the patient's self-esteem, the body shape, confidence and sexuality [8]. Constantini and colleagues observed a positive improvement in sexual function in both groups after sacrocolpopexy with or without hysterectomy in 107 patients. However, in patients who underwent uterine sparing surgery compared to hysterectomy group postoperative the postoperative Female Sexual Function Index (FSFI) showed a significant improvement in the total score and the desire, arousal and orgasm subgroups, but the median of the scores were significantly beter [16].
In this study, it was found that in laparoscopic group sexual life quality is better than sacrospinous hysteropexy. It was determined that the most intense vaginal dryness complaints occurred in the laparotomy group and the most severe dyspareunia complaints occurred in the sacrospinous hysteropexy group.
It has been determined that those who have complaints of vaginal dryness in the study have a lower total score of SQLQ-F but only in the sacrospinous hysteropexy group complaint of vaginal dryness affects the quality of sexual life. We attribute this to performing this technique unilaterally may disruption the anatomical position so by this way it can affects the quality of sexual life.
This study suggests that uncomplicated pregnancy to full term is possible following this technique and pregnancy has no harmful affect on apical support in women post-hysteropexy. More cases with longer follow-up are required to consolidate the data for pregnancy and hysteropexy.
One of the most commonly used methods to protect the uterus in pelvic organ prolapse is sacrospinous hysteropexy, and a large study evaluating this procedure showed a 84% satisfaction rate [17]. Studies using POP-Q measurements have evaluated objective or anatomical success as improvement of apical measurement represented by C-point. Quality of life and sexual function outcomes appear favorable after sacrospinous hysteropexy. Additionally, the sacrohysteropexy has been shown to have promising outcomes with results comparable with hysterectomy and sacrocolpopexy. While the data on the efficacy of sacrospinous hysteropexy are conflicting sacrospinous hysteropexy remains an alternative to vaginal hysterectomy in women who desire future fertility or uterine conservation. However, women with severe advanced prolapse desiring uterine conservation are at a high risk of recurrence and should consider alternative approaches to hysteropexy [18,19]. We investigated that similar subjective success rates could be achieved with laparoscopic and laparotomical sacroshysteropexy. Therefore, we suggested that laparoscopic procedure was comparable to conventional uterine protective techniques and in present study because of the no need for lateralization of the uterine vessels with the laparoscopic hysteropexy technique applied during the procedure, there was no major bleeding due to trauma of these vessels. One advantage of the laparoscopic hysteropexy operation was that there was no risk of slipping due to tissue passage (through myometrium).
Our study is retrospective and does not have a separate control group. This is the limiting feature of our work. On the other hand, it is not ethically appropriate to plan a prospective randomized controlled trial in cases that are candidates for hysteropexy. Another handicap of our work was that women with stage IV uterovaginal prolapse or cervical elongation were excluded because the available studies note a very high rate of prolapse recurrence in these patients and other was not independent assessor examining the patients postoperatively. This suggests that more long term data is needed to draw definitive conclusions of the long term efficacy and durability of hysteropexy.
Conclusion
According to our results, in laparoscopic hysteropexy sexual life quality was better than sacrospinous hysteropexy and in sacrospinous hysteropexy vaginal dryness affects the quality of sexual life negatively. In line with these results; application of lubricants and moisturizers to the vaginal area in the sacrospinous hysteropexy group, especially when the complaint of vaginal dryness affects the quality of sexual life, about 5-30 min before sexual intercourse to relieve vaginal instability. Women who require surgery to correct uterovaginal prolapse and who are seeking protection of the uterus should be recommended for hysteropexy as one of the options and should be consulted about the relatively low evidence of these procedures. They should be informed that the procedures has a successful rate in terms of the rate of anatomical treatment and resolution of symptoms after surgery.
In our study, hysteropexy was associated with more than 87.9% of good anatomic healing rates, so surgical correction of uterovaginal prolapse is a feasible alternative for women who need and want to protect their uterus due to various reasons. Uterine preservation apply from whichever way found to be a safe and effective treatment, even in cases with advanced uterine prolapse particularly for sexuel wellbing and desiring pregnancy.
References
- Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(2):165-194.
- Samuelsson EC, Victor FT, Tibblin G, et al. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. 1999;180:299-305.
- Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501-506.
- Marchionni M, Bracco GL, Checcucci V, et al. True incidence of vaginal vault prolapse. Thirteen years of experience. J Reprod Med. 1999;44(8):679-684.
- Rahmanou P, White B, Price N, et al. Laparoscopic hysteropexy: 1-to 4-year follow-up of women postoperatively. Int Urogynecol J. 2014;25(1):131-138.
- Fayyad AM, Siozos CS. Safety and one year outcomes following vaginally assisted laparoscopic uterine sacropexy (VALUES) for advanced uterine prolapse. Neurourol Urodyn. 2014;33(3):345-9.
- Zucchi A, Lazzeri M, Porena M, et al. Uterus preservation in pelvic organ prolapse surgery. Nat Rev Urol. 2010;7(11):626-633.
- Neuman M, Lavy Y. Conservation of the prolapsed uterus is a valid option: medium term results of a prospective comparative study with the posterior intravaginal slingoplasty operation. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(8):889-893.
- Gutman R, Maher C. Uterine-preserving POP Surgery. Int Urogynecol J. 2013;24(11):1803-1813.
- Gracia M, Perello M, Bataller E, et al. Comparison between laparoscopic sacral hysteropexy and subtotal hysterectomy plus cervicopexy in pelvic organ prolapse: a pilot study. Neurourol Urodyn. 2015;34(7):654-658.
- Korbly NB, Kassis NC, Good MM, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):e471-476.
- Pan American Health Organization (PAHO). Promotion of Sexual Health. Recommendations for Action, Guetamala. 2000.
- Gölba?? Z, Tu?ut N, ?entürk EA, et al. Prevalence of sexual dysfunction and some related factors in married women who applied to the gynecology policlinic. Cumhuriyet Medical Journal. 2014;36(4):1-10.
- Symonds T, Boolell M, Quirk F. Development of a questionnaire on sexual quality of life in women. J Sex Marital Ther. 2005;31:385-397.
- Thakar R, Sultan AH. Hysterectomy and pelvic organ dysfunction. Best Pract Res Clin Obstet Gynaecol. 2005;19:403-418.
- Constantini E, Porena M, Lazzeri M, et al. Changes in female sexual function after pelvic organ prolapse repair. Int Urogynecol J. 2013;24(9):1481-1487.
- Dietz V, Huisman M, de Jong JM, et al. Functional outcome after sacrospinous hysteropexy for uterine descensus. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):747-752.
- Lin TY, Su TH, Wang YL, et al. Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc. 2005;104(4):249-253.
- Dietz V, van der Vaart CH, van der Graaf Y, et al. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21(2):209-216.