Research Article - Biomedical Research (2017) Volume 28, Issue 21
Effects of thermal therapy combined with pamidronate disodium on pain associated with bone metastases: A randomized control trial (RCT) study
Fanlei Kong*, Zhihong Nie, Zhongpo Liu, Shibin Hou and Jiangfeng Ji
Department of Spine Surgery, Xingtai people’s hospital, Xingtai, China
Accepted on September 14, 2017
Abstract
Background: This is a Clinical Randomized Trail (RCT) to explore the metastatic bone pain treatment effect of hyperthermia combined with pamidronate disodium, for improving the quality of life who suffered from the metastatic bone disease.
Method: A total of 60 patients with metastatic bone pain were divided into two groups, 30 patients in each group: the patients in treatment group were treated with hyperthermia combined with pamidronate disodium, and the patients in control group were treated with pamidronate disodium only. The effect of treatment and the quality of life was observed in the fourth week.
Results: The effective rate of treatment group and the control group were 93.33% and 63.33% respectively, and the difference in the two groups was significance (χ2=8.235, P=0.016), the NCCN score of life quality showed that, the quality of life in two groups was improved after treatment, and the degree of improvement was more significant in treatment group. Then it was showed that the alkaline phosphatase levels in two group were all declined after treatment (P=0.021).
Conclusion: The treatment effect of hyperthermia combined with pamidronate disodium is better than that treated with pamidronate disodium only. We can consider the combination of hyperthermia with pamidronate disodium as a method to treat metastatic bone pain in clinical practice.
Keywords
Pamidronate disodium, Metastatic bone pain, Hyperthermia.
Introduction
Cancer-related pain is caused by the interactions of various factors, and considered as one of the most uncontrollable problems for cancer patients. To improve the life quality and outcomes of cancer patients [1], treatment of cancer-related pain is listed as one of the four key concerns of WHO’s comprehensive cancer control plan. Bone is the third most susceptible target organ of distant cancer metastases, which is only after liver and lung. In principle, every cancer can spread to bone, thus inducing cancer-related pain. The pathogenesis of bone metastasis is unique and complex. It is reported that about 70% of advanced breast cancer and prostate cancer spread to bone. Another 15%-30% of bone metastases occur to lung cancer and colorectal cancer [2]. Bone metastasis usually predicts a poor prognosis.
Thermal therapy is an emerging treatment for cancer after surgery, chemotherapy, radiotherapy and biotherapy [3]. Inducing the formation of precipitates in the tissues through thermal energy, thermal therapy increases the tumor temperature to a high level that inhibits the growth and causes the death of tumor cells. Thermal therapy can promote tumor cell apoptosis, inhibit tumor angiogenesis and migration, and enhance the patients’ immunity. Moreover, thermal therapy increases patients’ sensitivity to radiotherapy and chemotherapy while alleviates the side effects of radiotherapy and chemotherapy [4,5].
Pamidronate disodium as a bisphosphonate can help to strengthen bone weakened by cancer by preventing the morphological changes of osteoblasts caused by hydroxyapatite dissolution. In this way the osteoblast activity is inhibited and bone destruction is mitigated. Pamidronate disodium can also inhibit the activity of various mediators, thus reducing osteoblast activity and inhibiting bone resorption indirectly and relieving the pain [6].
Either thermal therapy or pamidronate disodium alone is proved effective against bone metastases in clinic, but the combined use of the two is rarely reported. This study investigated the treatment effect of thermal therapy combined with pamidronate disodium for pain associated with bone metastases, aiming to provide reference for pain relief of patients with metastatic bone diseases.
Subjects and Methods
Subjects
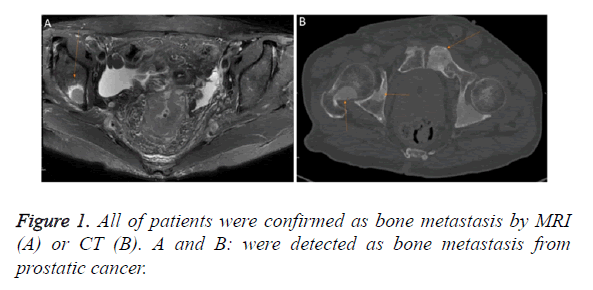
From November 2015 to April 2016, 60 inpatients of moderate to severe pain associated with bone metastasis at Xingtai People’s Hospital were included. There were 37 males and 23 females aged 30-81 y old. All of them were confirmed as bone metastases by CT or MRI scans (Figure 1). No radiotherapy or chemotherapy was given 4 weeks before the experiment. The expected survival was longer than 3 months. These cases had no intellectual or mental disorders. This study was conducted with approval from the Ethics Committee of the Xingtai people’s hospital. Written informed consent was obtained from all participants’ guardians.
Using the random number table method, patients were divided into treatment group and control group, with 30 cases in each group. The treatment group had 10 cases of breast cancer, 5 cases of lung cancer, 6 cases of liver cancer, 3 cases of prostate cancer, 3 cases of colorectal cancer, 1 case of esophageal cancer, and 2 cases of ovarian cancer. The control group had 8 cases of breast cancer, 7 cases of lung cancer, 5 cases of liver cancer, 4 cases of prostate cancer, 4 cases of colorectal cancer, 1 case of esophageal cancer, and 1 case of ovarian cancer. Comparison using χ2 test indicated no significant difference in age, the gender ratio, pain score during treatment and tumor type distribution between the two groups.
The control group received intravenous injection of 60 mg of pamidronate disodium diluted with 0.9% normal saline to 500 ml for over 4 h once daily. The injection was performed twice weekly, with 4 weeks as one cycle. The treatment group received radiofrequency therapy at the target position for 60 min each time, twice weekly for 4 w, treated with SR1000II thermal therapy device (Figure 2) using real-time virtual sonography system and guided by ultrasound [7]. After radiofrequency ablation, needle ablation is performed at the needle tip to prevent postoperative bleeding and tumor growth along the needle path. The treatment effect was evaluated at the end of 4 w. The above procedures were performed in strict accordance with the instructions. Any events occurring during the treatment were recorded.
Outcome evaluation
Pain scoring was performed using visual analog scale. Grade 0 (0 point) indicated no pain; grade 1 (1-3 points) indicated mild, bearable pain and that the patients could rest normally; grade 2 (4-6 points) indicated moderate but almost unbearable pain and that the patients needed to take pain killers to go to sleep; grade 3 (7-10 points) indicated severe, unbearable pain and that the patients could hardly go to sleep even after taking the pain killers.
Pain relief evaluation
Marked effect was defined as pain relief by 2 grades and above; moderate effect was defined as pain relief to some extent, with neither relief nor aggravation; no effect was defined if the pain was initially relieved but later restored to the previous intensity.
Statistical analysis
Statistical analyses were conducted using IBM SPSS 19.0 software. Counts were expressed as frequencies (percentages) and compared by using the chi-square test between the two groups. Measurements were expressed as mean ± standard deviation and compared by using independent samples t-test between the two groups. Paired sample t-test was used for intra group comparisons between and after treatment. Pain grading used Mann-Whitney test. P<0.05 indicated significant difference.
Results
Comparison of baseline information between the treatment group and control group
The treatment group had 16 males and 14 females, and the control group had 21 males and 9 females. The chi-square test indicated no significant difference in the gender ratio between the two groups (χ2=1.763, P=0.184). There was no significant difference in age between the two groups using the independent two-sample t-test (t=1.587, P=0.118); neither was there significant difference in pain score between the two groups before treatment (χ2=0.272, P=0.873) (Table 1).
| Index | Treatment group (n=30) | Control group (n=30) | χ2/t, Mann-Whitney test | P |
|---|---|---|---|---|
| Gender (male) | 16 | 21 | 1.763 | 0.184 |
| Age | 54.20 ± 4.68 | 59.70 ± 4.01 | 1.587 | 0.118 |
| Pain grading | ||||
| Painless (grade 0) | 0 | 0 | ||
| Mild pain (grade 1) | 6 | 7 | ||
| Moderate pain (grade 2) | 15 | 13 | ||
| Severe pain (grade 3) | 9 | 10 | 0.272 | 0.873 |
| Tumor types | ||||
| Breast cancer | 10 | 8 | ||
| lung cancer | 5 | 7 | ||
| Liver cancer | 6 | 5 | ||
| prostatic cancer | 3 | 4 | 1.266 | 0.974 |
| colorectal cancer | 3 | 4 | ||
| Esophagus cancer | 1 | 1 | ||
| Ovarian cancer | 2 | 1 |
Table 1. Comparison of baseline information between the two groups.
Evaluation of pain relief
The treatment lasted for 4 w. Comparison of the pain management effect after 2 w of treatment showed that the response rate was 83.33% in the treatment group vs. 53.33% in the control group, indicating significant difference (χ2=6.459, P=0.040). Comparison after 4 w of treatment showed that the response rate of the treatment group increased to 93.33% and that of the control group was 63.33%, also indicating significant difference (χ2=8.235, P=0.016) (Table 2).
| Group | Significant | Effective | Invalid | Effective rate (%) | χ2 | P |
|---|---|---|---|---|---|---|
| 2 w | 6.459 | 0.040 | ||||
| Treatment group | 8 | 17 | 5 | 83.33 | ||
| Control group | 4 | 12 | 14 | 53.33 | ||
| 4 w | 8.235 | 0.016 | ||||
| Treatment group | 11 | 17 | 2 | 93.33 | ||
| Control group | 6 | 13 | 11 | 63.33 |
Table 2. Comparison of pain relief between the two groups after 2 and 4 w of treatment.
Comparison of serum alkaline phosphatase (ALP) levels
The serum ALP level was compared between the two groups before and after treatment using independent two-sample t-test. The result showed that there was no significant difference in serum ALP levels between the two groups before or after treatment (Table 3). Paired sample t-test was used to compare the ALP level within each group before and after treatment. It was found that the serum ALP level decreased significantly in each group after treatment (Table 4).
| Alkaline phosphatase | Treatment group | Control group | t | P |
|---|---|---|---|---|
| Before treatment | 189.01 ± 42.12 | 180.57 ± 40.43 | 0.792 | 0.432 |
| After treatment | 128.00 ± 24.83 | 131.42 ± 26.63 | 0.541 | 0.609 |
Table 3. Comparison of serum ALP levels between the two groups before or after treatment.
| Alkaline phosphatase | Before treatment | After treatment | t | P |
|---|---|---|---|---|
| Treatment group | 189.01 ± 42.12 | 128.00 ± 24.83 | 8.044 | 0.000 |
| Control group | 180.57 ± 40.43 | 131.42 ± 26.63 | 6.683 | 0.000 |
Table 4. Comparison of serum ALP levels within each group before and after treatment.
NCCN score
Patients’ life quality was assessed using the rating scale enclosed in 2008 NCCN Guidelines for Adult Cancer-Related Pain. Seven aspects were assessed, namely, daily activity, emotion, walking ability, ability to work or do housework, relation with others, sleep and life enjoyment. The scoring was done on a scale from 0-10; the lower the score, the higher the life quality. The two groups differed insignificantly in life quality before treatment (t=0.175, P=0.862); however, the life quality showed significant difference between the two groups after treatment (t=2.368, P=0.021). As to intragroup comparison, there was significant difference after treatment in either group (P<0.05) (Table 5).
| Score | Treatment group | Control group | t | P |
|---|---|---|---|---|
| Before treatment (0 w) | 49.92 ± 8.99 | 50.29 ± 7.44 | 0.175 | 0.862 |
| After treatment (4 w) | 32.11 ± 8.98 | 37.72 ± 9.38 | 2.368 | 0.021 |
| t* | 8.818 | 7.294 | ||
| P* | 0.000 | 0.000 |
Note: t value and P value indicated intragroup difference between the two groups; t* and P* indicated significant difference within each group after treatment.
Table 5. Intragroup and intergroup comparisons of patients’ life quality before and after treatment.
Discussion
Bone metastatic disease has become one of the most common cancers and the management of the associated pain is a major evaluation indicator of life quality of these patients. Conventional treatments for bone metastases include radiotherapy, chemotherapy and bisphosphonates [8-10], each of which has a different working mechanism and limitations.
Pamidronate disodium is a second-generation bisphosphonate that can be absorbed onto the surface of bone trabeculae, thus preventing osteolysis and inhibiting the maturation and migration of the osteoblasts. Experiment showed that pamidronate disodium can effectively inhibit hydroxyapatite dissolution, thus affecting osteoblast activity, inhibiting bone resorption and relieving the pain. The general response rate of pamidronate disodium for treating the pain associated with bone metastases is 59%-84.6% [11]. In this study, the response rate was 63.33% after the use of pamidronate disodium alone for 4 w, which is quite satisfactory.
However, pamidronate disodium used alone may take effect slowly and have a lower local control rate. Its combined use with radiotherapy is most common. Fan et al. [12] achieved a 92% response rate of pain relief for bone metastases by combining pamidronate disodium with chemotherapy, which was higher than the use of pamidronate disodium alone. Pamidronate disodium can be also used in combination with compound Radix sophorae flavescentis injection or 153 Samarium- Ethylenediamine Tetramethylene Phosphonic Acid (153 Sm-EDTMP) [13,14] and the treatment effect is generally good. However, the combined use of pamidronate disodium and thermal therapy is rarely reported for pain associated with bone metastases. In this study, the response rate was 93.33% for the combined use of pamidronate disodium and thermal therapy, which was significantly higher than that of using pamidronate disodium alone; moreover, intragroup comparison also indicated significant difference before and after treatment. The NCCN score can reflect psychological pain in cancer patients. According to NCCN score, both two groups achieved an improvement of life quality after treatment, and the improvement was more considerable in the treatment group. This means the combined treatment can be feasibly applied to treat the pain associated with bone metastases.
Under normal conditions, bone remodeling is a process of dynamic equilibrium. However, once the dynamic equilibrium is disrupted by bone metastases, the ALP level, as an indicator of bone remodeling, changes correspondingly [15,16]. Serum levels of ALP increased in patients with bone metastases. It is an important guideline for determining osseous metastases to detect the serums ALP in patients with malignancy regularly.
Intragroup comparison found a marked reduction in the ALP level after treatment in either group. However, no obvious difference in the reduction degree of ALP levels was observed between the two groups. This finding requires further collaboration by studies with larger sample size.
Thermal therapy can exert a thermal effect by inducing the formation of precipitates and by increasing the temperature in the tumor (40-44°C). Thus the tumor cells are killed by high temperature without harming the normal cells. This therapy can work synergistically with other therapies, thus magnifying the analgesic effect. Studies [17-19] have shown that the combined use of thermal therapy and radiochemotherapy can achieve a better analgesic effect than the use of radiochemotherapy alone. Because of this benefit, thermal therapy has been widely used as an adjuvant therapy for pain associated with bone metastases. Chemotherapy combined with thermal therapy can increase the tumor cell membrane permeability, thus facilitating the absorption of the chemotherapeutic drugs. High temperature induced by thermal therapy can promote blood circulation around the tumor so that the local concentration of drug in the tumor can increase [20]. However, not all tumor patients can accept thermal therapy as the treatment may cause a series of physiological changes [21]. Therefore, a proper choice of procedures and timing of thermal therapy and skilful operation are important for ensuring outcomes. However, the combined use of thermal therapy and pamidronate disodium is not evidence-based, and the current study only had limited sample size. More multi-center clinical trials with larger sample size are needed for consolidating the benefits of the combined use of thermal therapy. The limitation of this study is that the sample size is small and the clinical observation time is short, so we can expand the number of samples and long-term follow-up, in order to further verify the metastatic bone pain treatment effect of hyperthermia combined with pamidronate disodium.
Conclusion
A randomized controlled and blind clinical trial was conducted in this study. The research showed that the treatment effect of hyperthermia combined with pamidronate disodium is better than that treated with pamidronate disodium only. We can consider the combination of hyperthermia with pamidronate disodium as a method to treat metastatic bone pain in clinical.
Conflict of Interest
The authors declare that there is no conflict of interest to disclose.
References
- Matza LS, Fallowfield LJ, Chung KC, Currie BM, Van Brunt K, Patrick DL. Patient-reported outcome instruments used to assess pain and functioning in studies of bisphosphonate treatment for bone metastases. Support Care Cancer 2012; 20: 657-677.
- Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 2001; 27: 165-176.
- Matsumine A, Takegami K, Asanuma K, Matsubara T, Nakamura T, Uchida A, Sudo A. A novel hyperthermia treatment for bone metastases using magnetic materials. Int J Clin Oncol 2011; 16: 101-108.
- Kaur P, Hurwitz MD, Krishnan S, Asea A. Combined hyperthermia and radiotherapy for the treatment of cancer. Cancers (Basel) 2011; 3: 3799-3823.
- Wang H, Li X, Xi X, Hu B, Zhao L, Liao Y, Tang J. Effects of magnetic induction hyperthermia and radiotherapy alone or combined on a murine 4T1 metastatic breast cancer model. Int J Hyperthermia 2011; 27: 563-572.
- Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J, Scagliotti GV, Sleeboom H, Spencer A, Vadhan-Raj S, von Moos R, Willenbacher W, Woll PJ, Wang J, Jiang Q, Jun S, Dansey R, Yeh H. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol 2011; 29: 1125-1132.
- Santiago FR, Garcia MDMC, Montes JLM, García MR, Fernandez JMT. Treatment of bone tumours by radiofrequency thermal ablation. Curr Rev Musculoskelet Med 2009; 2: 43-50.
- Goblirsch M, Lynch C, Mathews W, Manivel JC, Mantyh PW, Clohisy DR. Radiation treatment decreases bone cancer pain through direct effect on tumor cells. Radiat Res 2005; 164: 400-408.
- Yamada K, Kohno N. Efficacy of bisphosphonates for bone pain control. Nihon Rinsho 2007; 65: 152-156.
- Katakami N. Lung cancer with bone metastasis. Gan To Kagaku Ryoho 2006; 33: 1049-1053.
- Coleman RE. Bisphosphonates for the prevention of bone metastases. Semin Oncol 2002; 29: 43-49.
- Fan TM, Charney SC, de Lorimier LP, Garrett LD, Griffon DJ, Gordon-Evans WJ, Wypij JM. Double-blind placebo-controlled trial of adjuvant pamidronate with palliative radiotherapy and intravenous doxorubicin for canine appendicular osteosarcoma bone pain. J Vet Intern Med 2009; 23: 152-160.
- Chen L, Cai J, Wang S, Hu L, Yang X. Effect of Radix Sophorae Flavescentis on activity of CYP450 isoforms in rats. Int J Clin Exp Med 2015; 8: 21365-21371.
- Liu H, Zhan H, Sun D, Xu W, Ye X, Zhang H, Zhao C, Bao C, He G, Yin F. Analysis of multiple factors related to hematologic toxicity following 153Sm-EDTMP therapy. Cancer Biother Radiopharm 2007; 22: 515-520.
- Merk S, Hentschel M, Talazko J, Fischer R, Moser E. Unusual bilateral Tc-99m DPD uptake on bone scan. Clin Nucl Med 2003; 28: 929-930.
- Schindler F, Lajolo PP, Pinczowski H, Fonseca FL, Barbieri A, Massonetto LH, Katto FT, Del Giglio A. Bone and total alkaline phosphatase for screening skeletal metastasis in patients with solid tumours. Eur J Cancer Care (Engl) 2008; 17: 152-156.
- Ko SH, Ueno T, Yoshimoto Y, Yoo JS, Abdel-Wahab OI, Abdel-Wahab Z, Chu E, Pruitt SK, Friedman HS, Dewhirst MW, Tyler DS. Optimizing a novel regional chemotherapeutic agent against melanoma: hyperthermia-induced enhancement of temozolomide cytotoxicity. Clin Cancer Res 2006; 12: 289-297.
- Cohen EE, Ahmed O, Kocherginsky M, Shustakova G, Kistner-Griffin E, Salama JK, Yefremenko V, Novosad V. Study of functional infrared imaging for early detection of mucositis in locally advanced head and neck cancer treated with chemoradiotherapy. Oral Oncol 2013; 49: 1025-1031.
- Shoji H, Motegi M, Osawa K, Okonogi N, Okazaki A, Andou Y, Asao T, Kuwano H, Takahashi T, Ogoshi K. A novel strategy of radiofrequency hyperthermia (neothermia) in combination with preoperative chemoradiotherapy for the treatment of advanced rectal cancer: a pilot study. Cancer Med 2015; 4: 834-843.
- Yudina A, Moonen C. Ultrasound-induced cell permeabilisation and hyperthermia: strategies for local delivery of compounds with intracellular mode of action. Int J Hyperthermia 2012; 28: 311-319.
- Smith CJ, Myers CS, Chapple KM, Smith KA. Long-term follow-up of 25 cases of biopsy-proven radiation necrosis or post-radiation treatment effect treated with magnetic resonance-guided laser interstitial thermal therapy. Neurosurgery 2016; 79: 59-72.