Case Report - Biomedical Research (2017) Volume 28, Issue 12
Effects of the traditional Chinese auricular point therapy combined with relaxation training on patients with hypertension and anxiety
Liying Li1, Kewei Zhang2 and Na Shi3*
1Shandong Medical College, PR China
2Rehabilitation Medicine Department, Rizhao Central Hospital, PR China
3Rehabilitation Department, Linyi People‘s Hospital, 27, Dong Duan, Jiefang Road, Lanshan District, Linyi City, Shandong Province, PR China
Accepted on April 3, 2017
Abstract
Objective: To observe influences of the traditional Chinese auricular point therapy combined with relaxation training on patients with primary hypertension and anxiety.
Method: Conduct random allocation on 86 inpatients with primary hypertension and anxiety according to Pocock and Simon's minimization method; 43 patients in the observation group were treated with routine nursing, ear acupoint application therapy combined with regular relaxation training (2 times/d, 30 min/time, 2 weeks of continuous training); 43 patients in the control group were only treated with routine nursing. The SAS was adopted during admission and after 2 weeks of intervention to conduct effect evaluation and record blood pressure changes.
Results: The antihypertensive efficiency in the observation group was obviously higher than that of the control group. The difference had statistical significance (p<0.05). The blood pressure, total SAS score, psychogenic and somatic anxiety scores got improved obviously after intervention. The difference had statistical significance (P<0.01). Insomnia and mood of anxiety in somatic anxiety factors were improved obviously (P<0.05); the cardiovascular, respiratory and sensory systems in psychogenic factors were improved obviously (P<0.05).
Conclusion: The traditional Chinese auricular point therapy can lower blood pressure and improve anxiety.
Keywords
Traditional Chinese auricular point therapy, Relaxation training, Primary hypertension, Anxiety, Nursing.
Introduction
Hypertension is a kind of psychosomatic disease. Some report indicated that 37.5% people in China were diagnosed as primary hypertension and anxiety [1]. The research showed that the traditional Chinese auricular point therapy, as a good adjuvant therapeutic method, was characterized by fast and obvious effectiveness, less adverse effects, cheap price, good compliance and depressurization function [2-4]. At present, there are few researches on regular depressurization combined with auricular point therapy in treating patients with primary hypertension and anxiety in China [5]. This method was adopted in this paper with good effects.
Objects and Methods
Objects
86 inpatients with confirmed primary hypertension and anxiety were selected from the department of cardiology in our hospital from April, 2014 to August, 2016. Inclusion criteria: 1. the diagnosis of hypertension conforms to standards of Guidelines for Prevention and Control of Hypertension in China in 2005; that is, systolic blood pressure ≥ 140 mmHg (1 mmHg=0.133 kPa) and/or diastolic blood pressure ≥ 90 mmHg; 2. Total evaluation score of HAMA >14; 3. Patients have independent behavior capacity; 4. Informed consent. Inclusion criteria: 1. Patients with secondary hypertension; 2. Patients with serious hepatic or renal insufficiency or unstable vital signs; 3. Patients who cannot complete the survey due to mental or physical disability; 4. Patients who are allergic to tapes. Patients were divided into the observation group and the control group according to Pocock and Simon’s minimization and randomization method. The observation group was composed by 43 patients including 23 males and 20 females with age of 53.6 ± 8.3 and course of disease of 8.5 ± 0.6, of which there were 43 married patients and no single patients; 37 patients had health insurance and 6 patients paid medical fees by themselves; hypertension grade: 8 patients: grade 1; 7 patients: grade 2; 28 patients: grade 3; hypertension risk stratification: 5 patients: I; 5 patients: II; 24 patients: III; 9 patients: IV; education level: 4 patients: illiteracy; 22 patients: under university degree; 10 patients: above university level; occupation: 9 farmers; 23 workers; 7 businessmen; 4 cadres. The difference in gender, age, course of disease, marital status, hypertension grades and risk stratification, education levels and occupations etc. had no statistical significance (P>0.05) but with comparability [6,7].
Method
Questionnaire (general conditions): gender, age, residence, occupation, marital status, children’s health condition, history of hypertension, history of chronic disease, history of serious diseases among family members, permanent residence, fund source and contact information etc. [8,9].
HAMA: this scale covers 14 items including anxious mood, tension, fears, insomnia, intellectual, depressed mood, somatic (muscular), somatic (sensory), cardiovascular symptoms, respiratory symptoms, gastrointestinal symptoms, genitourinary symptoms, autonomic symptoms and behavior at interview. Each item has the full score of 4; the higher score means more serious anxiety. According to requirements of the manual, the HAMA scale can calculate the total score as well as somatic and psychogenic anxiety scores. The somatic anxiety covers seven dimensions including somatic (muscular system), somatic (sensory system), cardiovascular symptoms, respiratory symptoms, gastrointestinal symptoms, genitourinary symptoms and autonomic symptoms. The somatic anxiety score=total score of 7 dimensions/7; the psychogenic anxiety covers 7 dimensions including anxious mood, fears, insomnia, intellectual, depressed mood and behavior at interview. The psychogenic anxiety score=total score of 7 dimensions/7. Patients with the total score>14 must have anxiety. The higher total scores mean more serious degree of anxiety. HAMA is a common scale used by the department of psychiatry, whose reliability is 0.93. The reliability of various individual symptoms is 0.83~1.00 with validity of 0.36.
Intervention method
Patients in the observation group were treated with the ear acupoint application therapy except for conventional antihypertensive therapy and routine nursing (including health education and mental nursing) of those in the department of cardiology. Acupoint selection: Shenmen, heart point, liver point, Sanjiao and kidney point [10,11]. Routine disinfection on auricles: GY-I-type auricular point detector was used to seek for sensitive spots. Then 0.5 cm° × 0.5 cm tapes with cowherb seeds were applied on selected auricular points. The operator shall press the front and back of auricles via the thumb and forefingers from light to heavy until patients felt sore, numb and aching or main and collateral channels’ radiation conduction remains “arrival of Qi”. Press each acupoint for about 20 s every time, 3~4 times/d; change to another ear per 3 days. Patients in the control group were only treated with conventional antihypertensive therapy and routine nursing. The intervention time: 14~28 d [12,13].
Criteria of antihypertensive effects are as follows: Obvious effects: drop of diastolic blood pressure ≥ 10 mmHg till normal or ≥ 20 mmHg; if with high systolic pressure, then drop to normal too; with effects: drop of diastolic blood pressure<10 mmHg, but to normal or 10~19 mmHg; if with high systolic pressure, then drop till ≥ 30 mmHg; no effects: patients who fail to reach the above mentioned. The obvious effect and “with effect” sum up to total effective rate. Criteria of anxiety improvement: according to HAMA score-reducing rate (score-reducing rate=(scores before treatment-scores after treatment)/ scores before treatment × 100%), patients with HAMA score-reducing rate ≥ 75% or HAMA ≤ 7 were regarded as clinical recovery; 50%~74% was considered as obvious progress. 25%~49% was regarded as progress; <25% was treated as invalid. The recovery and obvious progress sum up to total effective rate.
Data collection method
The evaluation was conducted one time within 24 h after entering the group and at the day of discharge by two designated researchers who received related training before, of whom one was responsible for inquiry and the other was responsible for observation. They will complete rating independently. The researchers explained contents to patients elaborately due to their different education levels. The scale will be kept by archives in the hospital after checking.
Statistical method
The SPSS 20.0 was adopted to conduct statistical analysis. The total HAMA score and factor score were represented by ͞x ± s. The grouping T rest and paired T test were used at the time of measuring data after normal distribution and homogeneity test of variance. The χ2 test was used for enumerating data. P<0.05 indicated that differences had statistical significance.
Results
Comparison of efficacy of therapies in two groups
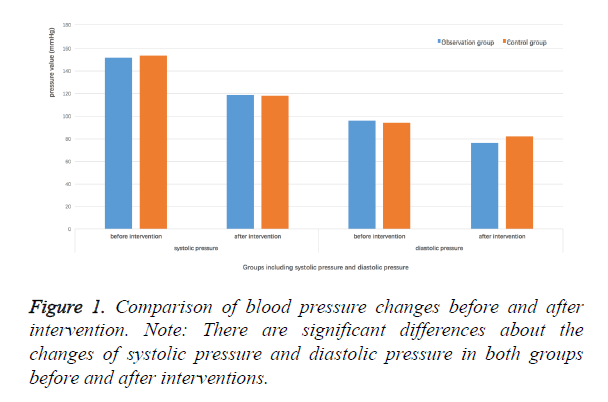
The amplitude of depressurization in the observation group was more obvious than that of in control group after treatment. The observation group has 29 patients with obvious effects, 8 patients with effects and 6 patients with no effects, while the control group had only 10 patients with obvious effects, 5 patients with effects and 28 patients with no effects. The antihypertensive effective rate in the observation group (86.0%) was obviously higher than that of the control group (34.9%). The difference had statistical significance (P<0.01). Comparison of blood pressure changes before and after intervention (Figure 1).
HAMA scores of two groups before and after treatment
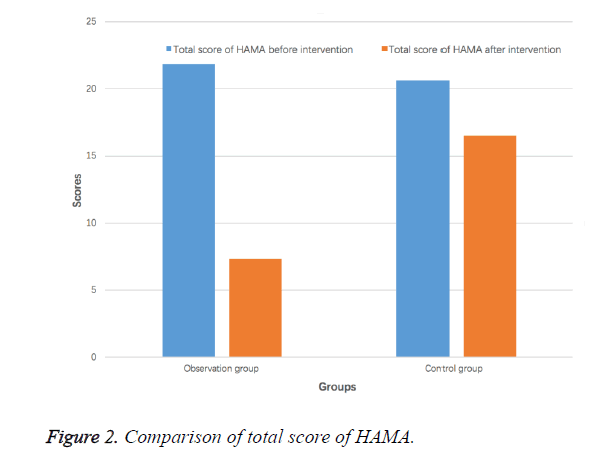
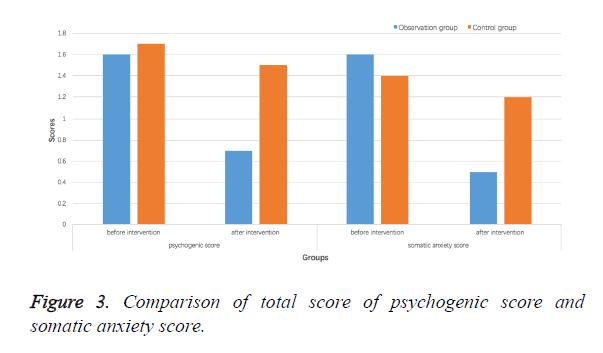
The total HAMA scores and various factor scores in the observation and control groups were decreased after treatment. The total score, psychogenic anxiety score and somatic anxiety score were decreased obviously compared with those before treatment and in the control group. The difference had statistical significance (P<0.01); 24 patients in the observation group were healed; 5 patients made obvious progress; 14 patients made some progress; there was no patient who made no progress, while no patients were healed in the control group; only 4 patients made obvious progress; 8 patients made some progress; 31 patients made no progress. The anti-anxiety effective rate in the observation group (62.2%) was obviously higher than that in the control group (9.1%). The difference had statistical significance (P<0.01). The concrete results, see Figures 2 and 3; concerning psychogenic anxiety factors, the number of score-reducing patients in the observation group was superior than top two items in the control group including insomnia (75.6% vs. 24.9%) and anxious mood (53.1% vs. 23.8%). Concerning somatic anxiety factors, the number of sore-reducing patients in the observation group was superior than top three items in the control group including cardiovascular symptoms (76.3% vs. 34.5%), respiratory symptoms (62.7% vs. 24.7%) and sensory systems (53.4% vs. 37.4%). The difference had statistical significance after χ2 test (P<0.05).
Discussion
Theoretical basis for traditional Chinese auricular point therapy; the auricular point therapy is the treasure of traditional Chinese medicine, whose theoretical basis include three aspects as follows: 1. Traditional Chinese medicine held ears are closely related to main and collateral channels as well as viscera. The disorder of organs and meridians is reflected on ears. The function activities of various organs can be adjusted by stimulating auricular points that are corresponding to organs and meridians [16]. 2. The auricular needles were emerging in Europe in 1950s. The French Doctor Nogier put forward an inversed auricular point diagram, which looked like an embryon. The internal organs as well as four limbs have their corresponding points and areas on auricles, which can be stimulated to activate vagus nerves, adjust functions of cardiovascular, respiratory, digestive, nervous and urinary systems etc. so as to cure diseases [17]. 3. The ear acupoint application therapy has certain psychological implications [18].
The traditional Chinese auricular point therapy can lower blood pressure and treat anxiety effectively. The hypertension is diagnosed as “headache” and “dizziness” etc. The pathogenesis is closely related to liver and kidney. The emotional depression will lead to liver disorder, while emotional arousal will cause liver-yang hyperactivity; or improper hygienism will cause kidney essence deficiency. The liver point can be used for soothing, clearing fire, calming endogenous wind and reducing excess together with Sanjiao; the kidney point can be used to nourish kidney-yin and liver. With three points together, it can reinforce deficiency and reduce excess by simultaneous treatment of principal and subordinate symptoms. Then the viscera become balanced and dizziness stops. The anxiety belongs to “depression syndrome” in the traditional Chinese medicine, which is mainly caused by heart-spleen deficiency, heart-kidney imbalance and liver depression of the fire due to tumultuous endeavour and negative thoughts. The heart controls mental activities. The heart point can tranquilize mind by nourishing the heart; the Shenmen point can clam nerves; the liver point can clear fire; the kidney point can nourish the liver and kidney; the Sanjiao point can regulate Qi flow; various points can be combined to eliminate evil, clam nerves and keep balance between Ying and Yang. The modern researches indicated that the hear point can strengthen the heart, regulate blood pressure and sooth the nerves etc. The liver point can disperse stagnated liver Qi for promoting bile flow, which can be used to treat angiopathy and regulate blood pressure etc. The kidney point can strengthen body and regulate vegetative nerve functional disturbance; the Shenmen has the functions of sedation, relieving dizziness, decreasing blood pressure and soothing nerves; the Sanjia is a reaction point of liver-qi invasion, whose response intensity is only second to the liver point. Various points can be combined to treat patients with primary hypertension and anxiety [19].
This research found that the decreasing amplitude of systolic pressure and diastolic blood pressure as well as the hypertensive effective rate in the observation group were obviously than those in the control group (P<0.01), which verified that the auricular point therapy had good effects on helping depressurization. The total HAMA score and various factor scores in the observation group was obviously lower than those in the control group (P<0.01); the psychogenic anxiety factors in the observation group was superior than top two items in the control group including insomnia and anxious mood. The somatic anxiety factors in the observation group were superior to those in top three items including cardiovascular symptoms, respiratory symptoms and sensory systems. Therefore, the mechanism of the auricular point therapy can improve sleep, correct anxious mood and reduce cardiovascular symptoms, respiratory symptoms and sensory symptoms [20].
Besides, the traditional Chinese auricular point therapy can not only treat anxiety and decrease blood pressure, which is especially applicable for patients with hypertension and anxiety as a rather good adjuvant therapy. However, though it has many advantages, its shortcomings should not be neglected. 1. It could not cure disease. Therefore, patients must receive regular treatment in the hospital regardless of its obvious effects against anxiety and hypertension as well as other advantages. 2. Its adverse effects cannot be neglected. For example, the Shenmen point calm and soothe the nerves, which can be used for insomnia and anxiety etc., but if with strong sedation, patients will have adverse effects such as drowsiness and slow intestine peristalsis etc. The sympathy point can adjust autonomic nervous functions and decrease blood pressure, while the clinical experience indicated that this point has diastolic functions etc.
References
- Muntingh A, Vand FC, Van Marwijk H. Effectiveness of collaborative stepped care for anxiety disorders in primary care: a pragmatic cluster randomised controlled trial. Psychother Psychosomat 2014; 83: 37-44.
- Steduto P. Actual evapotranspiration of a maize crop (Zea mays) as function of the canopy conductance. Rivista Di Agronomia 1993; 8: 145.
- Mcquade JL, Meng Z, Chen Z. Utilization of and attitudes towards traditional Chinese medicine therapies in a Chinese cancer hospital: a survey of patients and physicians. Evid Based Complement Alternat Med 2012; 2012: 504507.
- Jain M, Sharma N, Kalra S. To compare the effects of high and low frequency transcutaneous electrical nerve stimulation on acupuncture points in experimental pain threshold. Ind J Physiother Occup Ther 2011.
- Zhao L, Liu X, Chen J. Effects of anti-anxiety-depression treatment on depressurization in hypertensive patients with anxiety and depression. Med J Nat Defend Forces Southwest China 2013.
- Guo L, Huang L, Zhou X. Anxiety and depression influence the reduction of blood pressure in patients with initially diagnosed hypertension. Chin J Pract Nerv Dis 2014.
- Teng HU, Jiang Y, Tang HJ. Anxiety and depression among people with primary hypertension:A case-control study of prevalence and associated factors. Med J West China 2013.
- Cheruiyot G. Knowledge, attitudes and practices on diabetic retinopathy among patients attending the diabetes clinic at Kenyatta national hospital 2013.
- Wu L, He Y, Jiang B. Trends in prevalence, awareness, treatment and control of hypertension during 2001-2010 in an urban elderly population of China. Plos One 2015; 10: e0132814.
- Zheng LW, Chen Y, Chen F. Effect of acupressure on sleep quality of middle-aged and elderly patients with hypertension. Int J Nurs Sci 2014; 1: 334-338.
- Song C, Wang X. Clinical experience of needling ningshen point and ear acupoint to treat insomnia due to pathogenic fire derived from stagnation of liver-Qi. J Liaoning Univ Trad Chin Med 2013.
- Chen Y. Observation on the effect and nursing of acupoint sticking therapy combined with ear pressure beans in the treatment of vomiting of pregnancy. Chin Med Mod Dist Edu China 2016.
- Dan X. The clinical efficacy of conventional therapy combined with TCM mental nursing on the cervical spondylosis patients before and after menopausal. Sichuan Med J 2015.
- Taylor BC, Wilt TJ, Welch HG. Impact of diastolic and systolic blood pressure on mortality: implications for the definition of normal. J Gen Int Med 2011; 26: 685-690.
- Mizuno S, Matsuura K, Gotou T. Antihypertensive effect of casein hydrolysate in a placebo-controlled study in subjects with high-normal blood pressure and mild hypertension. Br J Nutr 2005; 94: 84-91.
- Wang X, Shi H, Shang H. Are Primo Vessels (PVs) on the surface of gastrointestine involved in regulation of gastric motility induced by stimulating acupoints ST36 or CV12. Evid Based Complement Alternat Med 2012; 2012: 787683.
- Lin YQ, Zheng M, Zhao BX. Three successful cases treated with moxibustion and embedding needle at auricular points. Zhongguo Zhen Jiu Chin Acupunt Moxib 2013; 33: 571-572.
- Jia YX, Xiao ZY. Observation on the clinical effect of ear acupoint press therapy with cowherb seed combined with psychological nursing care in the treatment of perimenopause syndrome. J Qilu Nurs 2009.
- Allice T, Enrietto M, Pittaluga F. Quantitation of cytomegalovirus DNA by real-time polymerase chain reaction in peripheral blood specimens of patients with solid organ transplants: Comparison with end-point PCR and pp65 antigen test. J Med Virol 2006; 78: 915-922.
- Francis JL, Weinstein AA, Krantz DS. Association between symptoms of depression and anxiety with heart rate variability in patients with implantable cardioverter defibrillators. Psychosom Med 2009; 71: 821-827.