Research Article - Biomedical Research (2017) Volume 28, Issue 17
Effectiveness and safety of ancillary device for endoscopic submucosal dissection
Yang Xu, Weiqing Shi, Xueting Zhang, Hanqin Zhang, Teng Yang, Aitong Li and Ranyun Zhou*
Department of Gastroenterology, 307 Hospital, Beijing, PR China
Accepted on August 16, 2017
Abstract
Objective: Endoscopic Submucosal Dissection (ESD) can be used to resect gastrointestinal diseases, but ESD costs long procedure time. It was reported that the rulers can serve as an ancillary device for shortening the procedure time. Thus, we aimed to identify a ruler assisted method performed by endoscopic nurses to shorten ESD procedure time and improve safety.
Methods: A total of 30 patients indicated for ESD in our hospital from January 2016 to May 2016 were prospectively enrolled and randomly divided into control and experimental group, which received routine and ruler assisted intervention, respectively. We compared the demographic and clinical characteristics, procedure time and perioperative complications between two groups, analyzed the application of ancillary device assisted ESD.
Results: There were 12 male and 3 female patients in control group. The diameter of the resected lesions was over 2.5 cm, and the maximal circumference was 9 cm. In experimental group, there were 6 male and 9 female patients. The diameter of the resected lesions was also over 2.5 cm, and the maximal circumference was 11 cm. The procedure time ranged from 45 to 90 min in control group, which ranged from 30 to 80 min in experimental group. There were no significantly statistical differences on the size of the resected specimen between the two groups. No obvious bleeding and perforation were observed.
Conclusions: Our prospective data proved that the ruler assisted endoscopic device for ESD is safe and effective in shortening procedure time and avoiding mucosal injuries and complications.
Keywords
Ancillary device, Efficacy, Safety, Endoscopic submucosal dissection (ESD).
Introduction
In recent years, great progress has been made on endoscopic technique, which facilitates the application of endoscopy in treating gastrointestinal diseases [1-3]. Endoscopic Submucosal Dissection (ESD) can be used to resect early cancer in gastrointestinal tract, and enable the en bloc resection of the lesion [4]. However, ESD is associated with long procedure time. The main possible reason may be that it takes a relatively long time to insert the device due to the long channel, no markers for measuring the insertion and uncertain speed and length of the insertion during the process of ESD. Previous researches have reported that the rulers can serve as an ancillary device for measuring the length of the endoscopic channel [5,6]. However, whether this ruler assisted method can be used for ESD has been rarely investigated. Thus, in this paper we aimed to identify an intervention method performed by the endoscopic nurses to shorten the ESD procedure time and improve the safety by introducing a ruler as an ancillary device, which can measure the distance from the entrance to the exit of the biopsy channel before ESD. We compared the procedure time and perioperative complications, analyzed the application of ancillary device assisted ESD.
Patients and methods
Patients
A total of 30 patients indicated for ESD in our hospital from January 2016 to May 2016 were prospectively enrolled. There were 18 men and 12 women. The age ranged from 34 to 72 and the average age was 52.5 y old. There were 7 patients with flat adenoma in colon, 3 patients with laterally spreading tumor in ileocecum, 5 patients with giant flat polyp in rectum, 12 patients with gastric stromal tumor and 3 patients with early gastric cancer. All the patients underwent ultrasound, which indicated the lesion was limited to mucosal muscularis or submucosa, the border was clear, muscularis propria was not involved, and the mucosa was lifted after injection. If the patients had contraindications for endoscopic procedures, they were excluded from the study.
This study was approved by the Ethic Committee of 307 Hospital. All the patients gave their written informed consent.
Grouping
The patients were randomly divided into control group (n=15) and experimental group (n=15) by using random number method. The two groups were treated by routine procedure and intervention procedure, respectively. The preoperative and postoperative treatments were the same in both groups.
ESD procedures
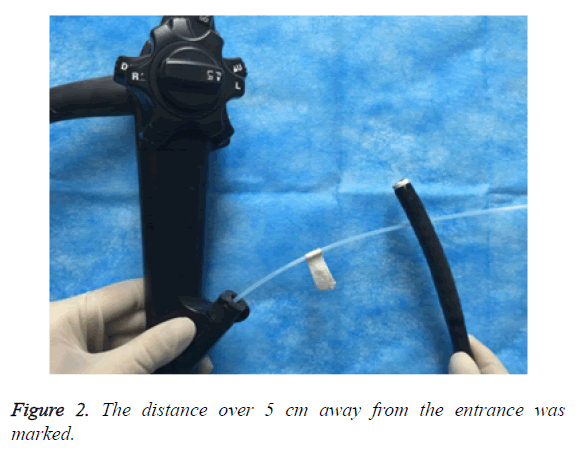
Before ESD, all the patients underwent related examinations. The whole ESD procedures were as follows: labelling, submucosal injection, circumferential pre-cut, dissecting and closing. In control group, routine procedures were performed. The endoscopic nurses cooperated with the endoscopist to complete the process of ESD. The device was independently selected by the endoscopists based on their habits and patients’ status. If the complications including bleeding and perforation occurred, the endoscopist and endoscopic nurses took timely measures. In experimental group, the patients were treated by intervention ESD. Before ESD, the distance from the entrance to the exit of the biopsy channel was measured (Figure 1), and marked on the wall. The effective upper and lower gastrointestinal endoscopy was 1100 cm and 1330 cm. The disposable devices including flex knife, Dula knife, IT knife, hot biopsy forceps were measured, and the distance at 5 cm away from the entrance was marked (Figure 2). During ESD, when the device was over 5 cm away from the entrance of the channel, the insertion could be quickening and no mucosal injury and perforation occurred. If the distance was within 5 cm, the insertion should be slowed down in order to avoid unnecessary mucosal injuries and exact localization of the device. The nurses should observe closely and remind the endoscopists during the procedures.
Statistical analysis
All the statistical analysis was conducted using SPSS17.0 software (SPSS Inc., Chicago, IL, USA). The continuous and categorical data were presented as mean (range) and percentage, respectively. The differences of these data were tested by using independent student t-test and chi-square test when applicable. A two tailed P value less than 0.05 was considered to be statistically different.
Results
Demographic and clinical characteristics
There were 12 male and 3 female patients in control group. The diameter of the resected lesions was over 2.5 cm, and the maximal circumference was 9 cm. In experimental group, there were 6 male and 9 female patients. The diameter of the resected lesions was also over 2.5 cm, and the maximal circumference was 11 cm. There were no statistically significant differences on the gender, age, the location and size of the lesions between the two groups (all P>0.05) (Table 1).
| Experimental group (n=15) | Control group (n=15) | P value | |
|---|---|---|---|
| Age (y) | 34-71 | 35-72 | 0.672 |
| Gender (n) | |||
| Female | 9 | 3 | 0.211 |
| Male | 6 | 12 | |
| Lesion location for ESD (n) | |||
| Stomach | 7 | 8 | 0.342 |
| Colon | 5 | 5 | |
| Rectum | 3 | 2 | |
| Maximal resected circumference (cm) | 11 | 9 | 0.781 |
Table 1. Demographic and clinical characteristics.
Efficacy and safety analysis
The procedure time ranged from 45 to 90 min in control group, which ranged from 30 to 80 min in experimental group (Table 2). There were no significantly statistical differences on the size of the resected specimen between the two groups. No obvious bleeding and perforation were observed. These results indicated that by measuring and labelling the length of endoscopic device, the endoscopists could be aware of the speed of inserting the endoscopy, which can save the procedure time and avoid unnecessary intragenic mucosal injuries.
| Experimental group (n=15) | Control group (n=15) | P value | |
|---|---|---|---|
| Procedure time (min) | 30-80 | 45-90 | 0.034 |
| Mucosal injuries (n) | 0 | 5 | - |
| Bleeding (n) | 0 | 3 | - |
| Perforation (n) | 0 | 0 | - |
Table 2. Efficacy and safety analysis.
Discussion
ESD has been widely applied in treating gastrointestinal mucosal lesions [7-9]. The success of ESD was determined by the characteristics of the lesion and the infiltration depth, as well as the endoscopic skills of the endoscopists [10,11]. In addition, the cooperation of endoscopic nurses and endoscopists also plays a vital role in ESD, and the close cooperation could greatly shorten the ESD procedure time [12-15].
During ESD, the endoscopists can push the endoscopy hard and quicken the insertion, but this mode may always neglect the length of the inserted endoscopy, which can pull the mucosa and lead to bleeding, perforation and even death. In this study, the endoscopic nurses measured and labelled the length of the endoscopy before ESD by using rulers as an ancillary device, which help the endoscopists be informed of the length. This technique can optimize the current ESD procedure. The advantages were listed as follows. First, the ruler assisted endoscopic device can help the endoscopists accurately localize the lesions and deliver the endoscopy much more safely, precisely and objectively. Second, the application of the ruler assisted endoscopic device for ESD is able to enable the quick passage of the biopsy channel and shorten the procedure time. Third, the ruler assisted endoscopic device could effectively reduce the risk of mucosal injuries, bleeding and perforation by accurate localization.
Based on the present study, our prospective data proved that the ruler assisted endoscopic device for ESD is safe and effective in shortening the procedure time and reducing the occurrence of mucosal injuries, bleeding and perforation. This conclusion may be further validated in large scale randomized controlled clinical trial.
Conflict of Interest
None.
References
- Jang JY. The Past, present, and future of image-enhanced endoscopy. Clin Endosc 2015; 48: 466-475.
- Graham DG, Banks MR. Advances in upper gastrointestinal endoscopy. F1000 Res 2015; 4.
- Cho JH. Advanced imaging technology other than narrow band imaging. Clin Endosc 2015; 48: 503-510.
- Barret M, Bordacahar B, Beuvon F. Self-assembling peptide matrix for the prevention of esophageal stricture after endoscopic resection: a randomized controlled trial in a porcine model. Dis Esophagus 2017; 30: 1-7.
- Kaz AM, Anwar A, O'Neill DR. Use of a novel polyp “ruler snare” improves estimation of colon polyp size. Gastrointest Endosc 2016; 83: 812-816.
- Nakatani H, Abe K, Miyakawa A. Three-dimensional measurement endoscope system with virtual rulers. J Biomed Optics 2007; 12: 051803.
- Perrod G, Pidial L, Camilleri S. ADSC-sheet transplantation to prevent stricture after extended esophageal endoscopic submucosal dissection. J Vis Exp 2017.
- Han Y, Guo J, Sun S. Acellular dermal matrix for esophageal structure prevention after endoscopic submucosal dissection in a porcine model. Gastrointest Endosc 2017.
- Aoki S, Sakata Y, Shimoda R. High-density collagen patch prevents stricture after endoscopic circumferential submucosal dissection of the esophagus: a porcine model. Gastrointest Endosc 2017; 85: 1076-1085.
- Wang H, Zhang H, Wang C. Expanded endoscopic therapy criteria should be cautiously used in intra-mucosal gastric cancer. Chin J Cancer Res 2016; 28: 348-354.
- Perrod G, Rahmi G, Pidial L. Cell sheet transplantation for esophageal stricture prevention after endoscopic submucosal dissection in a porcine model. PLoS One 2016; 11: e0148249.
- Nagami Y, Shiba M, Tominaga K. Hybrid therapy with loco regional steroid injection and polyglycolic acid sheets to prevent stricture after esophageal endoscopic submucosal dissection. Endosc Int Open 2016; 4: 1017-1022.
- Lua GW, Tang J, Liu F. Prevention of esophageal strictures after endoscopic submucosal dissection: A promising therapy using carboxy methyl cellulose sheets. Dig Dis Sci 2016; 61: 1763-1769.
- Kobayashi S, Kanai N, Tanaka N. Transplantation of epidermal cell sheets by endoscopic balloon dilatation to avoid esophageal re-strictures: initial experience in a porcine model. Endosc Int Open 2016; 4: 1116-1123.
- Takase K, Aikawa M, Okada K. Development of novel treatment with a bio-absorbable esophageal patch for benign esophageal stricture. Dis Esophagus 2015; 28: 728-734.