- Biomedical Research (2014) Volume 25, Issue 2
Effect of multimodal analgesia for postoperative pain on patients with lower limb fracture.
Laiyou Wen1,2*, Jianping Yang1, Jianzhong Miao2, Yongming Hu2, Ruiping Xue2 and Bing Huang21Department of Anesthesia, The First Affiliated Hospital of Soochow University, 215006, Suzhou, JiangSu Province
2Department of Anesthesiology of the Affiliated Jiangyin Hospital of Southeast University Medical College, 214400, JiangYin, JiangSu Province
- *Corresponding Author:
- Laiyou Wen
Department of Anesthesia
The First Affiliated Hospital of Soochow University
215006, Suzhou, JiangSu Province, China
Accepted date: February 03 2014
Abstract
The aim of the present study is to observe the effects of multimodal analgesia (MMA) for postoperative pain on patients with lower limb fractures. One hundred patients (American Society of Anesthesiology I~II, ASAI~II) with lower limb fractures, undergoing open reduction and internal fixation, under combined spinal and epidural analgesia (CSEA) were randomly divided into four groups: Control group (group C) and MMA groups I, II and III. All groups were administered IV fentanyl, for analgesia, after operation. The patients were followed up 6, 12 and 24h after operation and (visual analog scale) VAS score, fentanyl dose, pethidine frequency and adverse reactions were assessed. Results showed that, 12h, 24h VAS score, and 24h fentanyl dose of MMA group III were much lower than those of MMA groups I and II, while all of these were remarkably lower than those of group C (P<0.05). There were no statistically significant differences in pethidine frequency and adverse reactions at 24h among the four groups (P >0.05). It may be concluded that multimodal analgesia can effectively relieve postoperative pain in lower limb surgery.
Keywords
Multimodal analgesia (MMA), Lower limb fracture, Pain
Introduction
Besides the pain caused by the fracture itself, patients with lower limb fractures also suffer from postoperative problems like incision pain, limb swelling and activity limitation, which affect the quality of life of the patients [1]. Even though postoperative pain is gaining more and more attention nowadays, and lots of methods have been suggested which can help to ease pain [2], the effect is still not satisfactory. Up to 70% of the patients are not contented with the analgesic effect after operation, and another 25% to 55% experience changes from acute pain to chronic postoperative pain. The use of multimodal analgesia (MMA) is inevitable, since postoperative pain mechanism is complicated and no drug can act at all sites. MMA broadly refers to the combined use of different drugs or ways to ease pain [3]. Since at present there is no ideal MMA, we conducted this research to provide a reference for postoperative analgesia for future implementation of MMA on patients with lower limb fractures.
Materials and Methods
Clinical data
One hundred (62 males and 38 females) lower limb fracture patients (ASA I~II) with open reduction and internal fixation under combined spinal and epidural analgesia (CSEA), aged 18-65 years (46.74±16.48), with body mass 50-75 kg (64.65±11.72), duration of operation 65-88 min (73.62±12.49), and intraoperative blood loss 55-200 ml (112.48±54.64) were included in the study. Patients were randomly divided into four groups with 25 cases in each group. Fracture types: 17 cases of intertrochanteric fracture, 33 cases of femoral fracture, 21 cases of tibial fracture, 9 cases of fibular fracture, and 20 cases of combined tibia and fibula fracture.
Exclusion criteria includes: diabetes, drug abuse, hypertension, endocrine disorders, serious gastrointestinal ulcers, blood disorders, liver and kidney function abnormalities, non-steroidal anti-inflammatory drug allergy, history of aspirin induced asthma, enoxacin, lomefloxacin and norfloxacin drug users, severe psychological problems or history of mental illness who can not complete the investigation after surgery, drug dependence or allergy to any ingredient of analgesic drugs. There were no significant differences in gender, age, body mass, operative time, intraoperative blood loss, type of illness and exclusion criteria (P> 0.05), which were comparable among groups. The study was approved by the hospital medical ethics committee and was carried out with the informed consents of the patients.
Methods
Non-invasive blood pressure, electrocardiogram and pulse oximetry were monitored; oxygen was inhaled through nasal catheter at 1-2L/min; 200 - 300ml equilibrium liquid was infused into peripheral vein. L3-4 epidural spinal anesthesia was used with the patients in lateral position, by injecting 2-3ml 0.5% bupivacaine into the subarachnoid space and by implanting epidural catheters to control the anesthesia level under L12. If the block was incomplete, 1% lidocaine combined with 0.375% ropivacaine was infused into the epidural space. The anesthesia level was determined and accordingly different analgesic modalities were given to each group. For group C, patients were given IV and epidural saline injection, 10ml and 6ml respectively, both before and after the operation. Patients in MMA group I were given IV flurbiprofen 100mg plus epidural sufentanil 0.3ug/kg (diluted to 6ml with saline) before operation, and IV saline 10ml plus epidural saline 6ml after operation. Analgesic drugs in MMA group II were the same as for group I, but the only difference was that what was used before operation in group I were infused in group II after operation. Patients in MMA group III were injected IV flurbiprofen 50mg plus epidural sufentanil 0.15ug/kg (diluted to 6ml with saline) before surgery, and IV flurbiprofen 50mg plus epidural injections sufentanyl 0.15ug/kg (diluted to 6ml with saline) after surgery. PCIA mode of analgesia was implemented in all the four groups fentanyl 10ug/ml, plus tropisetron 5mg, total 100ml, drug load of fentanyl 50ug, infusion rate 2ml/ h, PCA volume 1ml with locking time 15min. IM injection of 50 mg of pethidine were given if patients feel pressing pain more than twice in a row.
Outcome measures
6h, 12h and 24hVAS score, 24h fentanyl dose, and 24h pethidine frequency (6h, 12h and 24h all refer to measurement after operation in this paper) were recorded, and adverse reactions were observed. VAS score is of 0 to 10 points, with 0 being painless, and 10 being the most painful. 24h fentanyl dose includes load, maintenance and additional dose. Pethidine frequency refers to the frequency of intramuscular injection of 50mg pethidine within 24h after operation, including multiple injections to the same patient. Adverse reactions include drowsiness, nausea, vomiting and itching, etc.
Statistical analysis
By using SPSS19.0 software to process, measurement
data was represented by mean plus& minus standard deviation
( ± s); comparison among groups was analysed
through variance; count data used chi-square test, of
which p<0.05 indicates that the difference is statistically
significant.
± s); comparison among groups was analysed
through variance; count data used chi-square test, of
which p<0.05 indicates that the difference is statistically
significant.
Results
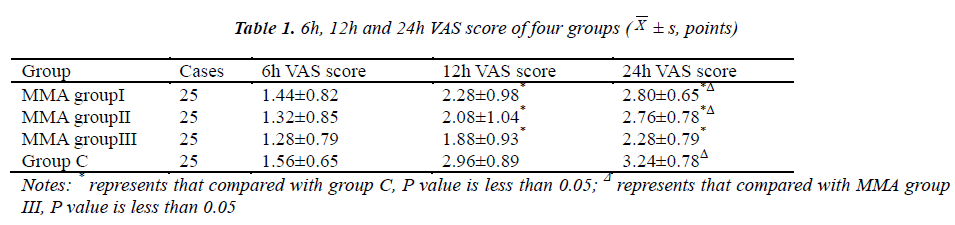
Comparison of VAS score after surgery
VAS scores at 12 and 24h after operation of MMA group I, II and III were markedly lower than those of group C (P<0.05), with statistically significant difference among the former three groups(P>0.05). 24h VAS score of MMA group III was much lower than those of MMA group I and II(P<0.05) (Table 1).
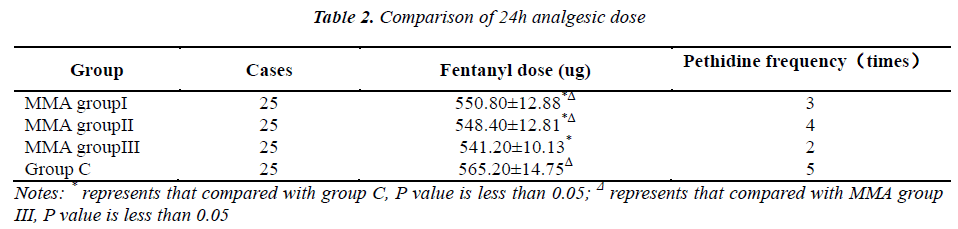
Analgesic dose within 24h after surgery
24h fentanyl dose of MMA group III was much lower than that of MMA group I and II, all of which were remarkably lower than that of group C (P<0.05). There was no statistically significant difference in 24h pethidine frequency among four groups(P>0.05) [See Table 2].
Adverse reactions
There were no cases of drowsiness or vomiting in any of the four groups. Cases of nausea in MMA group I, II, III and group C were 3, 2, 4 and 3 respectively. One patient from MMA group I and one from group III suffered itching, while no one in the other groups did. There was no statistically significant difference in adverse reactions among the four groups(P>0.05).
Discussion
Postoperative pain is a common complaint for lower extremity fracture patients, which can increase myocardial oxygen consumption and the risk of myocardial ischemia, prevent lung function recovery, suppress immune function and prolong hospitalization, thus affecting the quality of life of the patients. It may evolve into chronic pain and increase sufferings. Therefore, improvement of postoperative analgesia can help prognosis and rehabilitation in cases of lower limb fractures.
As a single analgesic drug or modality cannot achieve optimal pain relief, MMA, by using a variety of analgesic drugs or modalities simultaneously with superimposed or synergetic action can achieve complete analgesic effect, while reducing the dose of a single drug and the risk of adverse reactions at the same time [4-6]. This study showed that MMA is better than a single postoperative analgesia, which manifested as much lower 12h, 24hVAS score and 24h fentanyl dose of MMA groups than those of group C, which is consistent with previous reports [7]. Preemptive analgesia, an important part of MMA [8], emphasizes preoperative analgesic treatment in time period, and acts as a protective analgesia focusing on how to prevent the development of pain sensitivity. It should cover all stages of stimulation to central excitation by noxious stimulus, so as to inhibit peripheral and central sensitization effectively and to block central plastic changes. It seems like longer covering time of preemptive analgesia and timing of delivery contribute to the result that 12h, 24h VAS score and 24h fentanyl dose of MMA group III were significantly lower than those of MMA groups I and II. There were no statistically significant difference of adverse reactions among four groups, indicating that flurbiprofen axetil and sufentanil are safe and reliable to be used for MMA.
Major analgesic drugs like opioids (including opioid receptor agonists and antagonists), α2 receptor agonists, non-steroidal anti-inflammatory drugs, NMDA antagonists and local anesthetics are also important ones for preemptive analgesia. Opioids are golden standard drugs for postoperative pain medication, and patient-controlled analgesia (PCA) could meet the individual needs of patients. As a result, this study selected patient-controlled intravenous analgesia with fentanyl. The spinal cord is considered as a primary center for pain integration as well as an important part where pain stimuli induce neuroplasticity changes. It contains a large number of opioid receptors, which could be stimulated to suppress the release of excitatory amino acid (EAA), and to inhibit the pain signal to be passed up [9]. Intravenous opioids are unable to block nociceptive neuronal excitability adequately, while intrathecal analgesia is excellent and has synergistic effects combined with local anesthetic [10]. Epidural sufentanil has been used in the study, since it has a strong analgesic effect and can unite with spinal opioid receptors through the epidural route resulting in preemptive analgesia. Flurbiprofen is a new non-steroidal intravenous targeting analgesic, which encases the esterified flurbiprofen within fatty microspheres and can target at incision to form a local high concentration to obtain an outcome of inhibiting prostaglandin synthesis, reducing inflammatory mediators production and inflammatory responses, as well as increasing pain threshold and lowering pain transmission of nerve endings [11]. Wang Y et al [12] claim that intravenous flurbiprofen has the effect of preemptive analgesia, so we chose flurbiprofen in this study as one of the drugs in MMA.
In conclusion, intravenous flurbiprofen and epidural sufentanil combined with patient controlled intravenous fentanyl after surgery has good analgesic effect on patients with lower limb fractures, which indicates the superiority of MMA. However, specific mechanism of pain is unknown, and the pain level can change with external stimuli, individual tolerance, psychology and some other factors, on the basis of which there is no unified ideal MMA modality, so pain mechanisms and new therapeutic drugs need to be further studied.
References
- Sugi MT, Davidovitch R, Montero N, et al. Treatment of lower-extremity long-bone fractures in active, nonambulatory, wheelchair-bound patients. Orthopedics 2012; 35: e1376-1382.
- Perkins FM and Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology 2000; 93: 1123-1133.
- Young A and Buvanendran A. Recent advances in multimodal analgesia. Anesthesiol Clin 2012; 30:91-100.
- Wildgaard K, Petersen RH, Hansen HJ, et al. Multimodal analgesic treatment in video-assisted thoracic surgery lobectomy using an intraoperative intercostals catheter. Eur J Cardiothorac Surg 2012; 41: 1072-1077.
- Mislovic B. Multimodal analgesia including infraclavicular block in perioperative management of upper extremity amputation in neonate. Paediatr Anaesth 2011; 12: 1272-1273.
- Michelson JD, Addante RA, Charlson MD. Multimodal analgesia therapy reduces length of hospitalization in patients undergoing fusions of the ankle and hindfoot. Foot Ankle Int 2013; 11: 1526-1534.
- Zukowski M and Kotfis K. The use of opioid adjuvants in perioperative multimodal analgesia. Anaesthesiol Intensive Ther 2012; 1: 42-46.
- Trabulsi EJ, Patel J, Viscusi ER, et al. Preemptive multimodal pain regimen reduces opioid analgesia for patients undergoing robotic-assisted laparoscopic radical prostatectomy. Urology 2010; 5: 1122-1124.
- Sittl R, Irnich D, Lang PM. Update on preemptive analgesia : Options and limits of preoperative pain therapy. Anaesthesist 2013; 10: 789-796.
- Bujedo BM, Santos SG, Azpiazu AU. A review of epidural and intrathecal opioids used in the management of postoperative pain. J Opioid Manag 2012; 3: 177-192.
- Hao J, Wang K, Shao Y, et al. Intravenous flurbiprofen axetil to relieve cancer-related multiple breakthrough pain: a clinical study. J Palliat Med 2013; 2: 190-192.
- Wang Y, Zhang HB, Xia B, et al. Preemptive analgesic effects of flurbiprofen axetil in patients undergoing radical resection of esophageal carcinoma via the left thoracic approach. Chin Med J (Engl) 2012; 4: 579-582.