Research Article - Current Pediatric Research (2018) Volume 22, Issue 1
Early urethral obstruction sequence in fetuses or fetal obstructive uropathy (FOU): A study of 15 cases.
Nadia Ben Jamaa1, Radhouane Achour2, Nesrine Ben Hadj Dahman2, Sarra Mestri1,3, Sihem Hmissa1,3, Moncef Makni1,3, Mohamed Tahar Yacoubi1,31Research Unit, UR 03-08/21, Faculty of medicine of Sousse, Tunisia.
2Emergency Department of Gynaecology and Obstétrics of Maternity and Neonatology Center, Faculty of Medicine of Tunis, El-Manar University of Tunis, Tunisia
3Department of Pathology of CHU Farhat Hached, Sousse, Tunisia.
- Corresponding Author:
- Achour Radhouane
Emergency Department of Maternity and Neonatology Center
Faculty of Medicine of Tunis, El-Manar University of Tunis, Tunisia
Tel: 21698549398
E-mail: radhouane.a@live.com
Accepted date: January 29th, 2018
Abstract
Introduction: Early urethral obstruction sequence (FOU) consists on urethral obstruction, renal anomalies, ureterovesical dilatation, deficient abdominal wall, undescent testis and oligohydramnios. This condition poses problems of prenatal diagnosis and evaluation of renal impairment, etiology, management and genetic counseling. Our purpose is to study the patterns of urethral obstruction, the relation between obstructive uropathy and fetal phenotype and the type of renal anomalies in a retrospective study of 15 fetuses with F.O.U. An autopsy was performed with the dissection of the lower urinary tract and a histological study of kidneys in each case. Results: The gestational age was ranged between 13 and 33 weeks. The sex ratio was 13/2. Prenatal findings were: urinary tract abnormalities and oligohydramnios in 9 cases, nonspecified malformations in 3 cases, hydrocephalus in 1 case. Karyotype was normal in all the cases. Medical termination of pregnancy was performed in all cases. Anatomic obstruction of the urethra was found in 8 cases with 3 patterns (Atresia: 3 cases, stenosis: 3 cases, Urethral valve: 2 cases). Anatomic obstruction was absent in 7 cases. Megacystis was present in 14 cases, thin vesical wall in 12 cases, megaureters in 6 cases, bilateral hydronephrosis in 5 cases, Renal cystic changes in all cases and dysplastic changes in 11 cases. Conclusion: Renal changes in F.O.U. depend on the duration of obstruction. Anatomic obstructions of the urethra should be systematically demonstrated since they are the major cause of this phenotype. Prenatal diagnosis is compulsory indicating medical termination of pregnancy in such conditions.
Keywords
Fetus, Urethral, Early obstruction.
Introduction
Early urethral obstruction sequence (FOU) consists on urethral obstruction, renal anomalies, ureterovesical dilatation, deficient abdominal wall, undescent testis and oligohydramnios. This condition poses problems of prenatal diagnosis and evaluation of the degree of renal impairment, etiology, management and genetic counseling. Our center is qualified level 3, the age of fetal viability is estimated at 27 weeks of amenorrhea or a fetal weight higher than or equal to 900 g. The law in Tunisia allows abortion up to a gestational age of 12 weeks of amenorrhea. The earlier the age of prenatal diagnosis (20 weeks), the easier the indication of medical termination of pregnancy and less psychological impact on the patient.
Our purpose is to study the patterns of urethral obstruction, the relation between obstructive uropathy and fetal phenotype and the type of renal anomalies.
Materials and Methods
Our study was retrospective about 15 fetuses with F.O.U. collected at the Department of Pathology of CHU Farhat Hached (Sousse, Tunisia). A fetopathological examination was performed with a dissection of the lower urinary tract and a histological study of kidneys in each case. We used Excel as a statistical tool to analyze the data. Our study was performed after consent of fetus’s parents and approved by the Ethic committee of our institution. We were supported, in this study, by the research unit UR 03/08/21 of the faculty of medicine of Sousse, in Tunisia.
Results
We report 15 cases of fetal obstructive uropathy. The gestational age was ranged between 13 and 33 weeks. The sex ratio was 13/2. During the ultrasound scan, the prenatal findings were urinary tract abnormalities and oligohydramnios 9 cases; non-specified malformations in 3 cases and hydrocephalus in one case.
In all the cases, the Karyotype was normal and medical termination of the pregnancy was performed.
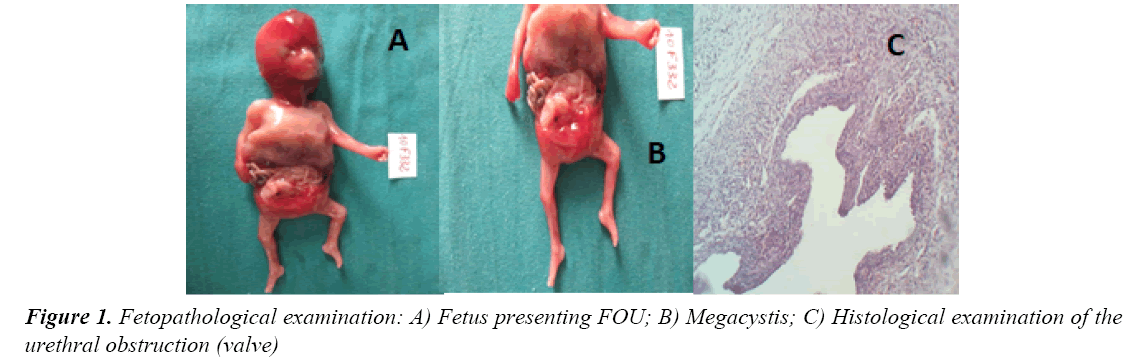
The fetopathological examination noted an anatomic obstruction of the urethra in 8 cases (53.4%) with 3 patterns an atresia in 3 cases (20%), a stenosis in 3 cases (20%) and an urethral valve in 2 cases (13.33%).The anatomic obstruction was absent in 7 cases (46.67%).
A megacystis was present in 14 cases (93.34%), a thin vesical wall in 12 cases (80%), megaureters in 6 cases (40%), a bilateral hydronephrosis in 5 cases (33.34%), renal cystic changes in all cases and dysplastic changes in 11 cases (73.34%). Renal cystic and dysplasic changes are detailed in Tables 1 and 2. Different other changes are listed in the Table 3.
| Fetal Age Number of cases |
<20 weeks N=8 |
>20 weeks N=7 |
|---|---|---|
| Cystic changes Absent to mild Moderate to severe |
5 3 |
2 5 |
Table 1: Renal cystic changes
| Fetal Age Number of cases |
<20 weeks N=8 |
>20 weeks N=7 |
|---|---|---|
| Dysplastic changes Absent to mild Moderate to severe |
3 5 |
6 1 |
Table 2: Dysplasic changes
| Type of Malformation | Number of Cases |
|---|---|
| Deformation complex | 8 |
| Pulmonary hypoplasia | 8 |
| Sexual ambiguity | 3 |
| Anorectal atresia | 2 |
| Gut malrotation | 1 |
| Hydrocephalia | 1 |
| Spina bifida | 1 |
| Laparoschisis | 1 |
| Diaphragmatic agenesis | 1 |
| Horse shoe kidney | 1 |
Table 3: Other changes
Discussion
Prune Belly syndrome is also known as Eagle-Barrett syndrome, first described by Finley et al. [1] in 1950, as a deficiency of the abdominal musculature with urinary tract abnormalities and cryptorchidism.
There are incomplete forms that need to be attached to this syndrome because of the characteristic urine lesions.
Currently most authors include all the signs originating from a urethral obstruction and definite the early urethral obstruction sequence characterized by severe bladder distension occurring at the end of the first trimester and can lead to renal dysplasia or hydronephrosis, oligohydramnios and pulmonary hypoplasia [2-5].
The pathogenesis of this sequence has been discussed, especially its relationship to both the abnormal development of the prostate and Prune Belly syndrome [6].
Some anomalies seen in this sequence such as pulmonary hypoplasia, Potter facials and limb abnormalities (clubfoot, arthrogryposis) are really the direct result of oligohydramnios [7]. In our study, we have reported 8 cases presenting these anomalies (53.34%).
FOU is often lethal by mid to late fetal life, that’s why pregnancy termination was indicated in all cases in our study. It is generally sporadic with an incidence of 1/35000 to 1/50000 births; the true incidence is still underestimated. The sex ratio is 20 for most authors but it was 13/2 in our study (Figure 1).
Prenatal diagnosis is possible by obstetrical ultrasound which should theoretically allow the detection of congenital uropathies if performed between 15 and 20 weeks of gestation [8]. Therefore, the prenatal diagnosis of malformation of the urinary tract is often done later. It is important to detect these malformations early to avoid the deterioration of the renal parenchyma, as fetal surgery is proposed today [9,10]. In our study, we noted that renal cystic and dysplastic changes are more severe before 20 weeks of gestation.
It is now possible in utero to decompress the obstruction via percutaneous vesicoamniotic shunting or cystoscopic techniques [10-12]. In appropriately selected fetuses intervention may improve perinatal survival, but long-term renal morbidity amongst survivors remains problematic.
So that, the medical termination of pregnancy is the only way in most cases especially when irreversible kidney damage is suspected or when this sequence is associated with a malformation syndrome.
Conclusion
Renal changes in FOU depend on the duration of obstruction. Anatomic obstructions of the urethra should be systematically demonstrated since they are the major cause of this phenotype.
Prenatal diagnosis is compulsory indicating medical termination of pregnancy in such conditions.
References
- Finley BE, Bennett TL, Burlbaw J, et al. Development of the Eagle-Barrett (prune belly) syndrome and a thickened, poorly functional bladder wall after early second-trimester decompression of fetal megacystis. Ultrasound Obstet Gynecol 1993; 3: 284-286.
- Confer SD, Galati V, Frimberger D, et al. Megacystis with an anterior urethral valve: Case report and review of literature. J Pediatr Urol 2010; 6: 459-462.
- Wu S, Johnson MP. Fetal lower urinary tract obstruction. Clin Perinatol 2009; 36: 377-390.
- Pringle KC, Zuccollo J, Kitagawa H, et al. Renal dysplasia produced by obstructive uropathy in the fetal lamb. Pathology 2003; 35: 518-521.
- Kumar S, Fisk NM. Distal urinary obstruction. Clin Perinatol 2003; 30: 507-519.
- Popek EJ, Tyson RW, Miller GJ, et al. Prostate development in prune belly syndrome (PBS) and posterior urethral valves (PUV): Etiology of PBS-lower urinary tract obstruction or primary mesenchymal defect? Pediatr Pathol 1991; 11: 1-29.
- Kitagawa H, Pringle KC, Zucollo J, et al. Early fetal obstructive uropathy produces Potter's syndrome in the lamb. J Pediatr Surg 2000; 35: 1549-1553.
- Shigeta M, Nagata M, Shimoyamada H, et al. Prune-belly syndrome diagnosed at 14 week’s gestation with severe urethral obstruction but normal kidneys. Pediatr Nephrol 1999; 13: 135-137.
- Daïkha-Dahmane F, Dommergues M, Muller F, et al. Development of human fetal kidney in obstructive uropathy: Correlations with ultrasonography and urine biochemistry. Kidney Int 1997; 52: 21-32.
- Smith-Harrison LI, Hougen HY, Timberlake MD, et al. Current applications of in utero intervention for lower urinary tract obstruction. J Pediatr Urol 2015; 11: 341-347.
- Morris RK, Malin GL, Quinlan-Jones E, et al. The Percutaneous shunting in Lower Urinary Tract Obstruction (PLUTO) study and randomised controlled trial: Evaluation of the effectiveness, cost-effectiveness and acceptability of percutaneous vesicoamniotic shunting for lower urinary tract obstruction. Health Technol Assess 2013; 17: 1-232.
- Kim SK, Won HS, Shim JY, et al. Successful vesicoamniotic shunting of posterior urethral valves in the first trimester of pregnancy. Ultrasound Obstet Gynecol 2005; 26: 666-668.