Letter to Editor - Biomedical Research (2022) Volume 33, Issue 8
Early aging in COVID-19 survivors.
1Research Department, Medical College, Aga Khan University, Stadium Road, Karachi, Pakistan
2Department of Cardiology, Punjab Institute of Cardiology, Lahore, Pakistan
- Corresponding Author:
- Dur-e-Najaf
Research Department
Medical College
Aga Khan University
Stadium Road, Karachi
Pakistan
To the Editor, The global pandemic, SARS-CoV-2, was first detected in Wuhan, China on 8th December 2019 and then caused havoc in devastating horizons. This novel virus that primarily spreads through droplets of saliva and nasal discharge of infected individuals has propelled scientific community worldwide to understand the pathogenesis of its varying clinical manifestations. Symptoms have ranged from mild to severe as the virus continues to target multiple systems of the human body. This global threat comes with a particular risk for elderly and those with pre-existing conditions, though the age selectivity of SARS-CoV-2 is still being fully understood.
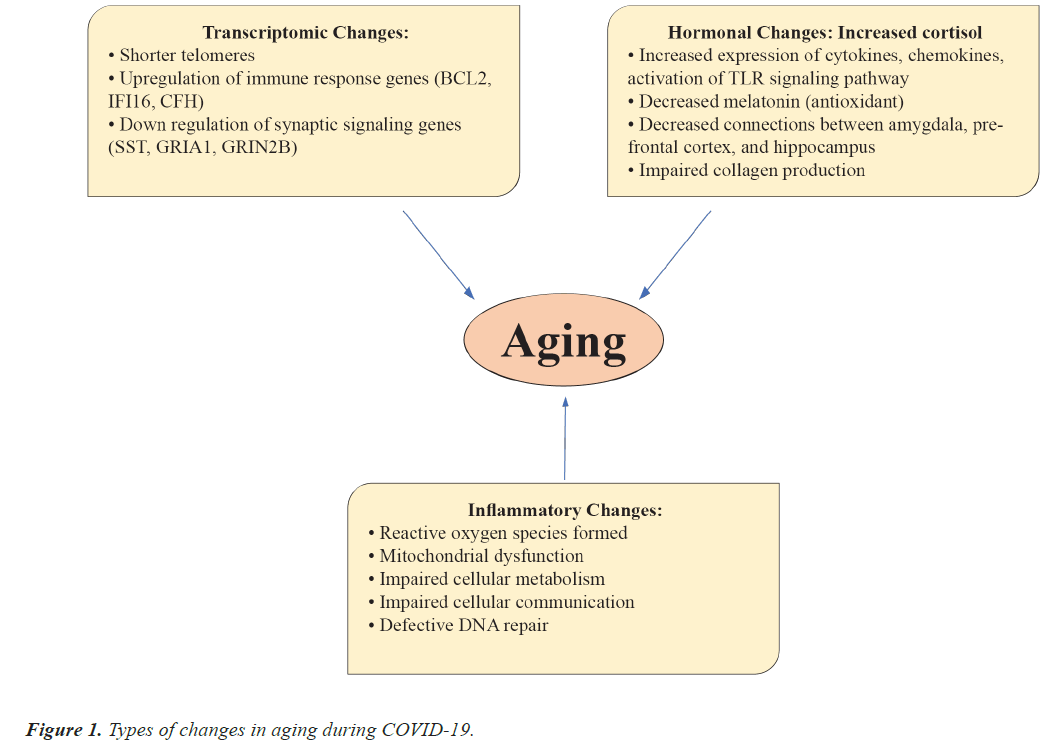
Of many recently made striking discoveries regarding the COVID-19, the pathogenesis and molecular biology of accelerated aging, a phenomenon influenced by both exogenous and endogenous stressors, in individuals with severe SARS-CoV-2 is of prime significance [1]. Epigenetics may help us understand the degenerative states of aging including cellular death, tissue inflammation and metabolic dysfunction due to the impaired mitochondrial function, cellular communication, DNA repair etc., [2].
SARS-CoV-2 binds to ACE2 receptors to gain entry into host cells and ultimately leads to reduce expression of ACE2 and IFN- gamma responses, which permits enhanced viral propagation. Rapid viral replication promotes cell death and damage causing an increased production of DAMPs (Damage Associated Molecular Patterns) and PAMPs (Pathogen Associated Molecular Patterns) [3]. A signalling pathway in response activates NF-κB transcription of many pro-inflammatory cytokines IL-6, IL-1β, IL-2, IL-8, IL-17, Granulocyte (G)-Colony-Stimulating Factor (CSF), Granulocyte-Macrophage (GM)-CSF, C–X–C motif Chemokine Ligand (CXCL)10, C-C motif Chemokine Ligand (CCL)2, CCL3 and TNF. These changes correlated with normal aging where basal levels of pro-inflammatory cytokines are elevated [4].
A study conducted in Spain by Raul and colleagues has highlighted the presence of shorter telomerase lengths in patients with severe COVID-19 compared to those with milder symptoms and shorter course of infection. Telomeres are specialized sequences at chromosomal ends to maintain genomic stability [5]. Shortening and ultimate loss of telomeric chromosomal ends not only decreases cell regeneration but also accelerates the process of DNA damage and cell apoptosis, contributing to aging. In a preprint cohort study, the post-mortem findings of the human cortex of COVID-19 patients with age and sex matched controls were analyzed for transcriptomic changes [6]. Significant enrichment of several genetic ontology terms related to aging of human brain was noticed along with enhanced up regulation of immune response genes (BCL2, IFI16, CFH) and down regulation of genes involved in synaptic signalling (SST, GRIA1, GRIN2B) [6].
Another research work has hypothesized that increased stress levels (physical, emotional, and mental) interfere with hormones regulating the process of aging. High levels of cortisol under stress lead to enhanced expression of proinflammatory effects of cortisol resulting in increased expression of cytokines, chemokines, complement proteins and activation of TLR signalling pathway [7]. Furthermore, raised stress levels cause decreased sleep and decreased melatonin production, which has antioxidant properties necessary to repair and build collagen, a major building block of bones, skin, muscles, ligaments, and tendons [8]. Previous studies on animals have shown the lasting effects of stress on brain circuits and systems, amygdala, pre- frontal cortex and hippocampus, affecting different aspects of memory, cognition, and visuospatial processing [9]. Therefore, signs of aging seen in COVID-19 patients such as thinning of skin and hair, impaired cognition and learning, memory impairment may now be better understood in context of high stress levels [7-9].
This understanding of aging at the level of molecular biology calls for intervention to both prevent and decrease the acceleration of aging in individuals infected by SARS- CoV-2. Regulation of inflammatory markers, gene therapy for telomerase shortening, psychotherapy and reduced isolation to keep stress levels in check may be some ways forward to combat the accelerated aging seen in COVID-19 patients (Figure 1).
References
- Ferrucci L, Fabbri E. Inflammageing: Chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol 2018 15:9. 2018; 15: 505-522.
[Crossref] [Google Scholar] [PubMed]
- Zhu X, Chen Z, Shen W. Inflammation, epigenetics, and metabolism converge to cell senescence and ageing: the regulation and intervention. Signal Transduct Target Ther 2021; 6: 1-29.
[Crossref] [Google Scholar] [PubMed]
- Khanmohammadi S, Rezaei N. Role of Toll-like receptors in the pathogenesis of COVID-19. J Med Virol 2021; 93: 2735-2739.
[Crossref] [Google Scholar] [PubMed]
- Bartleson JM, Radenkovic D, Covarrubias AJ, Furman D, Winer DA, Verdin E. SARS-CoV-2, COVID-19 and the aging immune system. Nat Aging 2021; 1: 769-782.
[Crossref] [Google Scholar] [PubMed]
- Sanchez-Vazquez R, Guío-Carrion A, Zapatero-Gaviria A, Martínez P, Blasco MA. Shorter telomere lengths in patients with severe COVID-19 disease. Aging 2021; 13: 1-15.
[Crossref] [Google Scholar] [PubMed]
- Yang AC, Kern F, Losada PM. Broad transcriptional dysregulation of brain and choroid plexus cell types with COVID-19. Nature 2021; 595: 565-571.
[Crossref] [Google Scholar] [PubMed]
- Jones C, Gwenin C. Cortisol level dysregulation and its prevalence-Is it nature’s alarm clock?. Physiol Rep 2021; 8: e14644.
[Crossref] [Google Scholar] [PubMed]
- Adam EK, Quinn ME, Tavernier R, McQuillan MT, Dahlke KA, Gilbert KE. Diurnal cortisol slopes and mental and physical health outcomes: A systematic review and meta-analysis. Psychoneuroendocrinology. 2017; 83: 25-41.
[Crossref] [Google Scholar] [PubMed]
- Zerbes G, Kausche FM, Schwabe L. Stress-induced cortisol modulates the control of memory retrieval towards the dorsal striatum. Eur J Neurosci 2022; 55: 2699-2713.
[Crossref] [Google Scholar] [PubMed]