Research Article - Gynecology and Reproductive Endocrinology (2017) Volume 1, Issue 1
Earlier Detection of Pregnancy with Serum Human Chorionic Gonadotropin Shows Excellent Prognostic Value in Gestation 4 Weeks after In Vitro Fertilization
Akiko Kawasaki1,2*, Hajime Okamoto2, Naoki Kita2, Yoko Ainoya2, Atsushi Wada2, Yukiko Wagatsuma3,Toyomi Sato11Department of Obstetrics and Gynecology, Faculty of Medicine, University of Tsukuba, Tsukuba, Ibaraki, Japan
2Department of Obstetrics and Gynecology, Tsukuba Gakuen Hospital, Tsukuba, Ibaraki, Japan
3Department of Clinical trial and Clinical Epidemiology, Faculty of Medicine, University of Tsukuba, Tsukuba, Ibaraki, Japan
- *Corresponding Author:
- Akiko Kawasaki
Department of Obstetrics and Gynecology
Faculty of Medicine
University of Tsukuba Tennoudai
Tsukuba
Ibaraki 305-8575
Japan
Fax/Tel: +81-29-853-3072/ +81-29-853-3073
E-mail: akawasaki@md.tsukuba.ac.jp
Accepted date: June 21, 2017
Citation: Kawasaki A, Okamoto H, Kita N, et al. Earlier Detection of Pregnancy with Serum Human Chorionic Gonadotropin Shows Excellent Prognostic Value in Gestation 4 Weeks after In Vitro Fertilization. Gynecol Reproduct Endocrinol -UK. 2017;1(1):16-20
DOI: 10.35841/2591-7994.1.1.16-20
Visit for more related articles at Gynecology and Reproductive EndocrinologyAbstract
Aim: To research whether the prognostic value of pregnancy outcome with a serum human chorionic gonadotropin (HCG) test is changed by 3 days earlier measurement in gestation 4 weeks after in vitro fertilization (IVF).
Methods: The study design is a retrospective analysis. Patients are women who underwent IVF in one institute. We investigated the difference in the prognostic value of serum HCG levels on day 16 and 19 from oocyte retrieval. Pregnancy outcomes are classified into biochemical pregnancy, miscarriage and ongoing pregnancy.
Results: In the serum HCG values on day 16, there was a significant difference among the three respective groups. In serum HCG values on day 19, there was a significant difference between the biochemical pregnancy group and miscarriage group, however there was no significant difference between the miscarriage group and ongoing pregnancy group. The AUC for prediction of ongoing pregnancy on day 16 was higher than the AUC on day 19.
Conclusion: The prognostic value of pregnancy outcome with serum HCG levels was decreased when the date of measurement was delayed only for 3 days.
Keywords
Human chorionic gonadotropin, Infertility, In vitro fertilization, Miscarriage, Pregnancy.
Introduction
Measurement of serum human chorionic gonadotropin (HCG) concentration is a standard method to detect pregnancies after in vitro fertilization (IVF). Radio immune assay or for HCG targeting the specific beta subunit of HCG dimer was established more than 30 years ago [1,2]. Today, more advanced assay methods are widely used in many medical institutes. While transvaginal ultrasound can detect pregnancies later than 4-5 weeks of gestation, measurement of serum HCG can detect them at later than 3 weeks of gestation because the HCG production from trophoblasts starts just after implantation [3].
Many studies reported that measurement of serum HCG or βHCG on a specific date after oocyte retrieval or embryo transfer is useful to differentiate normally progressing pregnancies from the abnormal course, and the measurement is useful to predict the clinical pregnancy outcomes [4-7]. For example, the serum HCG level is lower in ectopic pregnancies and miscarriages than in normal proceeding pregnancies, [4-7] and is higher in multiple pregnancies than in singleton pregnancies [8-9]. It is known that pregnancies achieved by IVF yield a relatively higher risk rate of miscarriages in the early pregnancy stage, ectopic pregnancies and multiple pregnancies than those achieved naturally [10]. The measurement of serum HCG in a pregnancy stage is beneficial for patients who underwent IVF for the early detection of these complications.
From previous studies, we know several factors that are possibly related to the serum HCG level after IVF. Several studies report that female age, [11] male infertility factor, [12] insemination method, [12] transferred embryos’ developmental stage, [13,14] and transferred embryo’s condition of frozen-thawed or fresh [15] are related to the serum HCG level. However, these opinions are not confirmed yet.
This study is intended to analyze how the prognostic value of the serum HCG concentration is altered in only 3 days difference in gestation 4 weeks after oocyte retrieval day in a single institute study with a retrospective method. The purpose of this research is to indicate that several days’ earlier judgment of pregnancy after IVF can help to know the pregnancy prognoses with a measurement of serum HCG levels.
Method
This study was approved by the local ethics committee of Tsukuba Gakuen Hospital. Subjects were patients who underwent IVF at Tsukuba Gakuen Hospital from January 2010 to December 2013. All patients provided written informed consents with guarantees of confidentiality before starting the treatment. We excluded patients who were diagnosed as ectopic pregnancies or multiple pregnancies in extracted samples. Additionally, we excluded patients who were injected with external HCG after oocyte retrieval for the purpose of luteal support.
Serum HCG measurement was performed on day 16 after oocyte retrieval in 67 patients (D16) and on day 19 in 74 patients (D19). Patients visited our hospital between day 16 and day 19 after oocyte retrieval for pregnancy judgment randomly. Because the sampling numbers of day 17 and day 18 were small as less than 50 cases, we chose day 16 and day 19 groups for the object of this study. Pregnancy was indicated by a serum HCG level of ≥5 IU/ L. Serum HCG concentrations were measured using enzyme immunoassay (E test “TOSOH” II , TOSOH Corporation, Tokyo).
IVF protocols include methods described in the previous studies [16-19]. Pituitary down-regulation was performed with a gonadotropin-releasing hormone (GnRH) agonist nasal spray 900 μg in a day from a mid-luteal phase of the previous cycle (long protocol), the same dose of GnRH agonist on day 2-4 of the ovarian stimulation cycle (short protocol) or GnRH antagonist protocol. GnRH antagonist was started when a leading follicle reached 14 mm (flexible protocol) or the sixth day of FSH injection (fixed protocol). Controlled ovarian stimulation was achieved with human menopausal gonadotropins (HMG), recombinant FSH (rFSH) or clomiphene citrate on day 2 to 4 of the cycle. The response to stimulation was monitored with a transvaginal ultrasound. When the size of a leading follicle reached the diameter of at least 18 mm, 10000 IU of HCG was injected. We trans-vaginally aspirated the follicles 33 hours after HCG injection.
Fertilization was performed by conventional IVF (cIVF), intracytoplasmic sperm injection (ICSI) with ejaculated spermatozoa (cICSI) or ICSI with testicular spermatozoa (TESEICSI). Embryo transfer (ET) of fresh embryos took place at 2 to 6 days after oocyte retrieval. For a luteal support, intramuscular progesterone injection 50 mg/day, or trans-vaginal progesterone 400 mg/day were used at least until the day of pregnancy judgment. Frozen-thawed ETs were performed in controlled cycles with external ovarian steroid hormone. Patients were given GnRH agonist nasal spray 900 μg/day starting in a midluteal phase of the preceding cycle. They were administered transdermal 17β-estradiol 2.16 mg/48 hours more than 2 weeks from the second day of menstruation in the ET cycle.
After an adequate endometrium proliferation was acquired, GnRH agonist was stopped and intramuscular progesterone injection or trans-vaginal progesterone was started at least until the day of pregnancy judgement after ET, and continued longer when the pregnancy was detected.
All patients underwent ultrasound examination at 5 to 6 weeks of gestation. We categorized three groups of pregnancy prognoses. Biochemical pregnancy (BP) was defined when no gestational sac was detected after serum HCG positive. Miscarriage (MC) was defined as pregnancy terminated until 9 weeks gestation with or without of detection of fetal heart beats. Ongoing pregnancy (OP) was defined as cases continued ≥10 weeks with fetal heart beats.
Statistical Analysis
SPSS ver. 21 and JMP11 for windows was used for statistical analysis. The serum HCG value was demonstrated as nonnormal distribution with Shapio-Wallis test. Since they were still shown as non-normal distribution after logarithmic conversion, they were proved to show strong non-normal distribution. Accordingly, the non-parametric method was adopted for statistical analysis. The Mann-Whitney U test was adopted for 2 groups’ comparison and Kruskal-Wallis H test for 3 groups’ comparison. Since the age distribution of the patients was normal, Student’s t test was adopted. χ2-test was used to compare categorical values. A P-value of <0.05 was considered statistically significant.
Results
Table 1 shows baseline characteristics and prognoses in the D16 and D19 groups. Between these groups, significant differences were not shown by the average age of patients, numbers of embryo, insemination methods, stages of transferred embryos, presence of male infertility factor, fresh embryos or frozen embryos and pregnancy prognoses. Serum HCG values showed significant differences between D16 group and D19 group.
| Parameters | D16 (n=67) | D19 (n=74) | total (n=141) | P-value |
| Age (years) | 34.7 ± 4.6 | 35.2 ± 4.3 | 34.9 ± 4.4 | a0.480 |
| Number of embryos | ||||
| SET | 56 (45.5%) | 67 (54.5%) | 123 (100%) | b0.216 |
| DET | 11 (61.1%) | 7 (38.9%) | 18 (100%) | |
| Type of insemination | ||||
| cIVF | 38 (48.1%) | 41 (51.9%) | 79 (100%) | b0.983 |
| cICSI | 24 (47.1%) | 27 (52.9%) | 51 (100%) | |
| TESE-ICSI | 5 (45.5%) | 6 (54.5%) | 11 (100%) | |
| Stage of embryos | ||||
| Cleaved | 6 (42.9%) | 8 (57.1%) | 14 (100%) | b0.713 |
| Blastcyst | 61 (48.0%) | 66 (52.0%) | 127 (100%) | |
| Male factor | ||||
| positive | 34 (51.5%) | 32 (48.5%) | 66 (100%) | b0.373 |
| negative | 33 (44.0%) | 42 (56.0%) | 75 (100%) | |
| Type of embryos | ||||
| Fresh | 9 (64.3%) | 5 (35.7%) | 14 (100%) | b0.186 |
| Frozen | 58 (45.7%) | 69 (54.3%) | 127 (100%) | |
| Prognosis | ||||
| BP | 11 (40.7%) | 16 (59.3%) | 27 (100%) | b0.428 |
| MC | 17 (42.5%) | 23 (57.5%) | 40 (100%) | |
| OP | 39 (52.7%) | 35 (47.3%) | 74 (100%) | |
| sHCG (IU/ml) | 328.8 (148.7-515.9) | 1087.0 (259.6-1887.5) | 489.5 (152.9-1176.4) | c0.000 |
| a Student’s t test; b χ2 analysis; c Mann-Whitney U test | ||||
Table 1: Baseline characteristics and prognosis in the D16 and the D19 groups. Age is expressed as mean ± standard deviation, sHCG is expressed as median (interquartile range), while other data are expressed as frequency.
Table 2 shows serum HCG values in subgroups of expected confounding factors. Significant differences were not shown in HCG values related to patient ages, types of insemination, stages of embryo, male factors and fresh or frozen ET.
| n (%) | sHCG (mIU/ml) | P-value | |
| Age | |||
| ≤ 34 | 63 (44.7%) | 515.9 (165.1-993.5) | b0.235 |
| 35-39 | 58 (41.1%) | 619.5 (182.3-1398.2) | |
| 40 ≤ | 20 (14.2%) | 306.4 (72.3-944.5) | |
| Type of insemination | |||
| cIVF | 79 (56.0%) | 517.9 (131.7-1325.1) | b0.634 |
| cICSI | 51 (36.2%) | 515.9 (172.0-1146.2) | |
| TESE-ICSI | 11 (7.8%) | 433.7 (36.3-1076.1) | |
| Stage of embryos | |||
| Cleaved | 14 (9.9%) | 471.0 (251.1-834.6) | a0.473 |
| Blastocyst | 127 (90.1%) | 517.9 (148.7-1258.7) | |
| Male factor | |||
| positive | 75 (53.2%) | 453.2 (148.7-1070.4) | a0.281 |
| negative | 66 (46.8%) | 560.7 (150.8-1422.7) | |
| Type of embryos | |||
| Fresh | 14 (9.9%) | 471.0 (334.9-616.8) | a0.420 |
| Frozen | 127 (90.1%) | 528.2 (131.7-1289.6) | |
| a Mann-Whitney U test; b Kruskal-Wallis H test | |||
Table 2: HCG values in subgroups for confounding factors. Serum HSG is expressed as median (interquartile range).
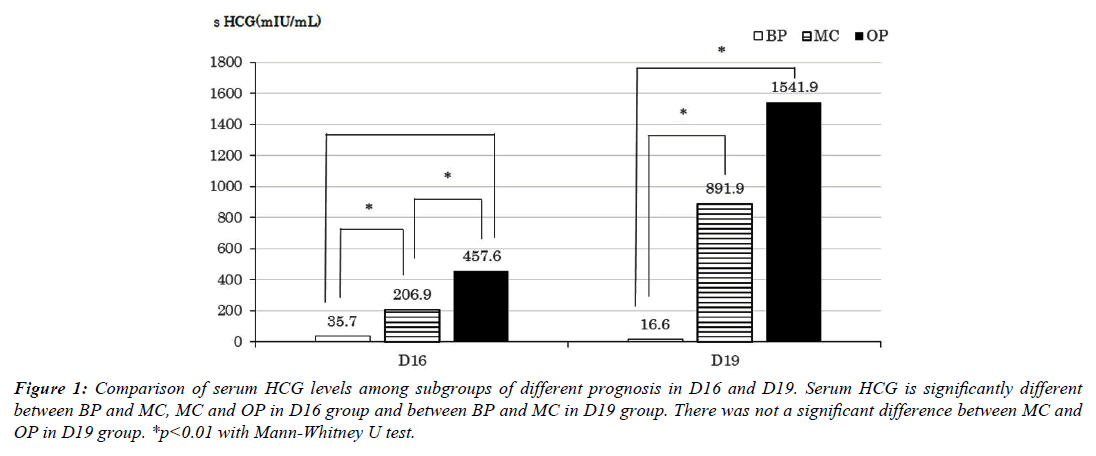
Figure 1 shows a comparison of serum HCG levels among subgroups of different prognoses in the D16 and D19 group. In the D16 group, serum HCG values were significantly different between BP and MC and between MC and OP. In the D19 group, serum HCG values were significantly different only between BP and MC.
Figure 1: Comparison of serum HCG levels among subgroups of different prognosis in D16 and D19. Serum HCG is significantly different between BP and MC, MC and OP in D16 group and between BP and MC in D19 group. There was not a significant difference between MC and OP in D19 group. *p<0.01 with Mann-Whitney U test.
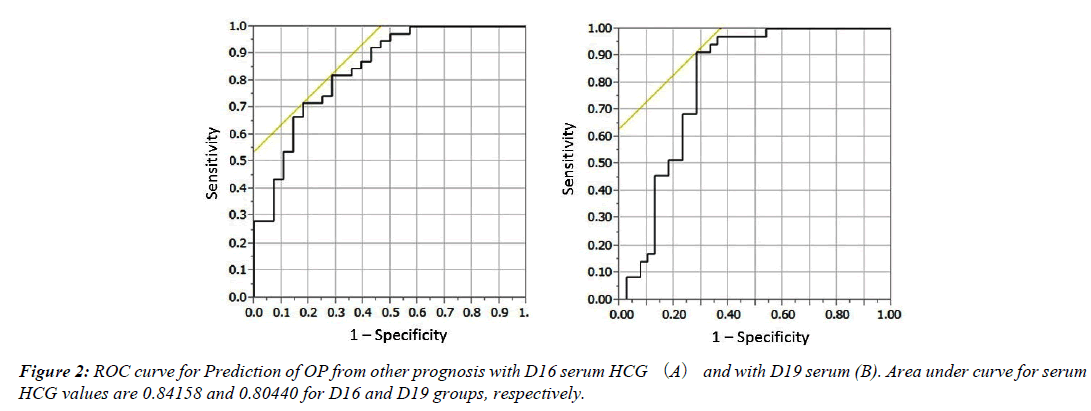
Furthermore, we investigated the predictive value of pregnancy prognoses from serum HCG level in the D16 and the D19 group using ROC in Figure 2. AUCs between OP and other groups are 0.84158 in the D16 group and 0.80440 in the D19 group. AUCs between BP and others groups are 0.92370 in the D16 group and 0.97306 in the D19 group. All four AUCs were statistically significant. In the comparison of AUCs, the predictive value of OP was superior in the D16 group to the D19 group.
Additionally, we calculated positive predictive values in respective cases with cut off values for optimal sensitivity and specificity (Table 3). The positive predictive value of OP in the D19 group was inferior to the value in the D16 group.
| aAUC | cut off value | bPPV | |
|---|---|---|---|
| BP in D16 | 0.92370 | 58.2 IU/L | 90.0% |
| BP in D19 | 0.97306 | 88.1 IU/L | 88.2% |
| OP in D16 | 0.84158 | 337.1 IU/L | 84.8% |
| OP in D19 | 0.80440 | 947.7 IU/L | 74.4% |
| a area under curve; b positive predictive value | |||
Table 3: Statistic values for BP and OP in D16 and D19 groups.
Discussion
This study indicated that the only 3 days difference in timing of pregnancy judgment produces the power of prediction of pregnancy prognoses. In day 16 judgment, the serum HCG level predicted the pregnancy prognoses BP, MC and OP, while in the day 19 judgment, the predictive power especially for distinguish OP from BP and MC was decreased.
Similarly to this research, several studies reported that measurement of serum HCG on day 14 and day 20 after oocyte retrieval or the measurement on day 14 or day 21 showed excellent predictive power for pregnancy prognoses [16,17]. Another study reported that the measurement from day 11 to on day 21 after oocyte retrieval indicated excellent predictive power of prognoses, while the measurement on day 14 may balance the accuracy of prediction.18 In more recent large scale studies, day 15 or 17 after oocyte retrieval showed an excellent predictive value for pregnancy prognoses [6,7]. Our research is unique from the standpoint of providing evidence that the measurement of serum HCG on day 16 yields stronger predictive power than the measurement on day 19.
According to previous studies, some confounding factors possibly influence serum HCG levels. Patient aging possibly decreases serum HCG levels, [11] and an insemination method of ICSI or the presence of a male infertility factor may decrease the levels [12]. The developmental stage of embryos is a candidate of these factors because blastocyst transfer may increase the levels [13,14]. The condition of embryos is also a candidate because frozen-thawed ET may increase the level compared to fresh ET [15]. Therefore, we showed those factors have no obvious influence on the serum HCG level in this study with the analysis shown in Table 2.
This research proved that 3 days’ earlier pregnancy judgment at 4 weeks of gestation after oocyte retrieval produced a higher prognostic value in a relatively small number of patients. As this research was performed in a single institute and the serum HCG was measured with the same enzyme immune assay system in the same laboratory unit, we could eliminate the error caused by the difference in examination systems. In our study, as the number of cases is small and the design is retrospective study, the influence of confounding factors cannot be completely eliminated. In order to decrease a disadvantage of the data sampling procedure, large scale studies and multi-variant analysis are needed to confirm the validity of the result.
In this research, we considered biochemical pregnancy as one pregnancy prognoses. In natural pregnancy, embryo growth often stops just after implantation, so they are not usually regarded as miscarriages as one category of abnormal pregnancy [19]. However, arrests of embryo growth at early pregnancy stage before the confirmation of gestational sac are possibly a phenomenon similar to miscarriages. Accordingly, we thought it beneficial to analyze BP as one type of pregnancy prognoses.
It is important to inform patients of the prediction of pregnancy outcome in the early stage after IVF. While early judgment of pregnancy can decrease the load of meaningless treatment, patients reportedly have strong mental stress before pregnancy prognoses is determined [20]. It is useful for patients’ mental support if serum HCG measurement has an excellent predictive ability for pregnancy prognoses.
However, one must avoid misjudgment from pursuing early diagnosis of pregnancy prognoses. IVF patients usually require luteal support for several weeks to maintain the pregnancy [21]. Discontinuing luteal support due to misjudgment can lead to unsuccessful childbirth.
One previous study indicated the efficacy of earlier pregnancy judgment less than 14 days after retrieval of eggs [22]. Should patients change the medicine for their own chronic severe disease with a high possibility of causing a fetal malformation to a more harmless medicine just after conception, early diagnosis of pregnancy until 4 weeks gestation is important. However, hurried judgment of pregnancy prognoses may cause a mistake. In spite of an extremely low HCG level in gestational 4 weeks, implantation delays may rarely bring continuous pregnancy. The final diagnosis of pregnancy prognoses should not be decided by a single measurement of serum HCG. Repeated measurements with a careful observation of clinical courses of fetal growth are necessary. More investigations are needed to confirm the safety and efficacy of early pregnancy judgment earlier than 16 days after oocyte retrieval.
In conclusion, in order to predict pregnancy prognoses, a serum HCG measurement on day 16 is more effective than on day 19 after oocyte retrieval. Larger scale studies and prospective controlled studies are needed to exclude confounding factors and confirm the result of this study.
Acknowledgements
We would like to thank our embryologist, Mrs. Yukiko Hara, who has generously been working at both Tsukuba Gakuen Hospital and the University of Tsukuba to support our laboratory work.
References
- Ayala AR, Nisula BC, Chen HC, et al. Highly sensitive radioimmunoassay for chorionic gonadotropin in human urine. J Cin Endocrinol Metab 1978;47:767-773.
- Armstrong EG, Ehrlich PH, Birkens S, et al. Use of a highly sensitive and specific immunoradiometric assay for detection of human chronic gonadotropin in urine of normal, nonpregnant and pregnant individuals. J Cin Endocrinol Metab 1984;59:867-874.
- Chen X, Li J, Jiang D, et al. A highly sensitive electrochemiluminescence immunoassay for detecting human embryonic human chorionic gonadotropin in spent embryo culture media during IVF-ET cycle. J Assist Reprod Genet 2013;30:377-382.
- Confino E, Demir RH, Friberg J, et al. The predictive value of hCG beta subunit levels in pregnancies achieved by in vitro fertilization and embryo transfer: an international collaborative study. Fertil Steril 1986; 45:526-531.
- Yamashita T, Okamoto S, Thomas A, et al. Predicting pregnancy outcome after in vitro fertilization and embryo transfer using estradiol, progesterone, and human chorionic gonadotropin beta-subunit. Fertil Steril 1989;51:304-309.
- Wu G, Yang J, Xu W, et al. Serum beta human chorionic gonadotropin levels on the day 12 after in vitro fertilization in predicting final type of clinical pregnancy. J Reprod Med 2014;59:161-166.
- Zhang Q, Yan J, Tang R, et al. Serum human chorionic gonadotropin level measured 17 days after oocyte retrieval can predict final clinical pregnancy outcomes in IVF/ICSI treatment cycles. J Reprod Med 2014;59:285-292.
- Bjercke S, Tanbo T, Dale PO, et al. Human chrionic gonadotrophin concentrations in early pregnancy after in-vitro fertilization. Hum Reprod 1999;14:1642-1646.
- Seeber BE. What serial hCG can tell you, and cannot tell you, about an early pregnancy. Fertil Steril 2012;98:1074-1077.
- Schenker JG, Ezra Y. Complications of assisted reproductive techniques. Fertil Steril 1994;61:411-422.
- Haavaldsen C, Fedorcsak P, Tanbo T, et al. Maternal age and serum concentration of human chorionic gonadotropin in early pregnancy. Acta Obstet Gynecol Scand 2014;93:1290-1294.
- Poikkeus P, Hiilesmaa V, Tiitinen A. Serum HCG 12 days after embryo transfer in predicting pregnancy outcome. Hum Reprod 2002;17:1901-1905.
- Kathiresan AS, Cruz-Almeida Y, Barrionuevo MJ, et al. Prognostic value of beta-human chorionic gonadotropin is dependent on day of embryo transfer during in vitro fertilization. Fertil Steril 2011;96:1362-1366.
- Oron G, Esh- Broder E, Son WY, et al. Predictive value of maternal serum human chorionic gonadotropin levels in pregnancies achieved by in vitro fertilization with single cleavage and single blastocyst embryo transfers. Fertil Steril 2015;103:1526-1531.
- RelJic M, Knez J, Vlaisavljevic V. Human chorionic gonadotropin levels are equally predictive for pregnancy outcome after fresh and vitrified- warmed blastocyst transfer. J Assist Reprod Genet 2013;30:1459-1463.
- Glatstein IZ, Hornstein MD, Kahana MJ, et al. The predictive value of discriminatory human chorionic gonadotropin levels in the diagnosis of implantation outcome in in vitro fertilization cycles. Fertil Steril 1995;63:350-356.
- Sugantha SE, Webster S, Sundar E, et al. Predictive value of plasma human chorionic gonadotrophin following assisted conception treatment. Hum Reprod 2000;15:469-473.
- Ochsenkühn R, Arzberger A, von Schönfeldt V, et al. Predictive value of early serum beta-hCG levels after single blastocyst transfer. Acta Obstet Gynecol Scand 2009;88:1382-1388.
- Annan JJ, Gudi A, Bhide P, et al. Biochemical pregnancy during assisted conception: a little bit pregnant. J Clin Med Res 2013;5:269-274.
- Lawler CC, Budrys NM, Rodgers AK, et al. Serum beta human chorionic gonadotropin levels can inform outcome counseling after in vitro fertilization. Fertil Steril 2011;96:505-507.
- Van der Linden M, Buckingham K, Farquhar C, et al. Luteal phase support for assisted reproduction cycles. Cochrane Database Syst Rev 2011;5:CD009154.
- Shapiro BS, Daneshmand ST, Restrepo H, et al. Serum HCG measured in the peri-implantation period predicts IVF cycle outcomes. Reprod Biomed Online 2011;25:248-253.