Research Article - Biomedical Research (2017) Volume 28, Issue 1
Does preoperative neutrophil-to-lymphocyte ratio have a value in predicting recurrence in bladder tumour after intravesical BCG treatment?
Ahmet Camtosun, Huseyin Celik*, Ramazan Altintas, Ibrahim Topcu, Cemal TasdemirDepartment of Urology, Inonu University School of Medicine, Malatya, Turkey
Accepted date: April 4, 2016
Abstract
The purpose of this study was to evaluate the prognostic value of the ratio of preoperative neutrophil to lymphocyte after intravesical BCG treatment in non-muscle invasive bladder cancer (NMIBC). The data of 89 patients, operated for urothelial carcinoma and treated with BCG after the diagnosis of NMIBC between 2007 and 2014, were reviewed retrospectively. Preoperative complete blood counts and first cystoscopic examination findings of the patients were examined. Median follow-up was 28.7 months. Tumour recurrence was detected in 33 patients (Group 2) of 89 patients. There was no tumour recurrence in 56 patients (Group 1). Neutrophil/lymphocyte ratio, MPV and CIS incidence were significantly increased in Group 2. This study showed that, preoperative high neutrophil/lymphocyte ratio, MPV and CIS occurrence can be used as independent criteria to predict tumour recurrence after intravesical BCG treatment in NMIBC.
Keywords
Cancer, Lymphocyte, BCG, Neutrophil, MPV.
Introduction
Bladder cancer is the most common cancer of urinary tract and the seventh most frequent among all cancers. The incidence is 9-27/100000 and 2-6/100000 and mortality is 3-8/100000 and 1-3/100000 in men and women, respectively [1,2]. Non-muscle invasive bladder tumours (NMIBC) have low progression rate and longer life expectancy when compared to the muscle invasive tumours. Five-year recurrence rate is 70% in high grade NMIBCs, whereas it is 15-40% and progression rate is less than 5% in low grade tumours. Recurrence within 5 years is related with 50% muscle invasion in high grade NMIBC’s [3].
After resection of high grade NMIBC, intravesical Bacille Calmette-Guerin (BCG) instillation is the most effective method to prevent the progression of tumour, but in the selected cases or patients who do not respond to BCG therapy, radical cystectomy is the recommended treatment option. Other current intracavitary agents are not as effective as BCG [4]. The anti-tumour mechanism of BCG depends on the local immune response to BCG that activates the MHC Class 2 antigen, T cells, macrophages, natural killer cells (NK) and B cells on the urothelial cells of bladder wall and the local infiltration of bladder wall. After BCG administration, not only a local response but also a systemic response begins [5,6]. Inflammatory cells located next to the tumour especially play an important role in the alteration of the character of the inflammatory response according to the type of tumour. The most common seen tumour-associated alteration of systemic immune response is relative lymphopenia or thrombocytosis. Tissue neutrophils may be associated with poor prognosis. In addition, increased neutrophil/lymphocyte ratio (NLR) has been shown as a poor prognostic factor in malignancies [7].
About 1/3 of the patients benefit from the treatment, whereas1/3 of them don’t show any change and the last 1/3 has tumour progression which requires the radical cystectomy [8]. Many studies conducted that NLR has been found to provide predictive information about gastrointestinal tumours [5]. It has been found that this ratio also provides predictive information for renal cell carcinoma (RCC) [9]. In our study, we examined the availability of parameters of preoperative complete blood count to predict the tumour progression in the patients with bladder cancer that didn’t respond to intravesical BCG instillation therapy.
Materials and Methods
Between 2007 and 2014, data of the patients who had nonmuscle invasive bladder tumour diagnosed after transurethral resection were retrospectively examined. Pathological grades of tumours World Health Organization/International Society of Urological Pathology classification is determined based on. The patients received intravesical BCG induction and maintenance therapy scheduled as once a week for six weeks and once a month for 12 months, respectively, after diagnosis were included into the study. After the primary resection of tumour, cystoscopy+cytological examination were performed four times throughout the first year, twice a year for the subsequent 2 years and once a year after the fourth years for the follow-up. The patients with hematologic, infectious or chronic diseases were excluded in the current study. To have bladder tumour during cystoscopy and cytological control was considered as recurrence and inclusion criteria for this study. A new tumour formation of somewhere different from the primary site, advance in the stage or grade of tumour was accepted as progression of the tumour. Age, gender, occupational exposure, smoking habits, concomitant diseases, the number and location of the primary tumour, presence of carcinoma in-situ, tumour grade, pathological stage and preoperative complete blood count were retrospectively obtained from the data of the patients included to the study.
Laboratory Data
Haemoglobin (Hb) levels, white blood cell count (WBC), neutrophil, lymphocyte and platelet counts, mean platelet volume (MPV), red blood cell distribution width (RDW)were obtained using Beckman coulter LH780 and Beckman coulter LH750 (California-USA) analyser. NLR and Platelet/ lymphocyte ratio (PLR) values were obtained via dividing the absolute neutrophil and platelet counts to absolute lymphocyte count, respectively.
Statistics
Statistical analysis was obtained using the SPSS (Statistical Package for Social Sciences, SPSS Inc., Chicago) software package version 9.0. Continuous data were expressed as mean ± SD. The categorical variables were summarized as percentages. The comparison of the groups was done via using Chi-square test for the categorical variables, Student t test for the independent samples and Mann-Whitney U test for the continuous variables. Pearson or Spearman correlation tests were performed in the correlation assessment.
In logistic regression analysis, p<0.10 adjusted p values for the variables identified as potential risk markers were included in the full model. Multivariate stepwise logistic regression analysis was performed by modelling the potential risk markers were eliminated p value of <0.05 was considered statistically significant and the confidence interval was 95%. Analysis was carried out in two variants. NLR and PLR before the procedure and a categorical variable in the second model are the first model have been considered as a continuous variable.
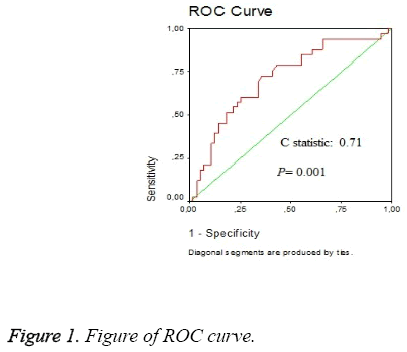
Additional cut-off point discovery evaluation was performed using receiver operating characteristic curve analysis. Survival analysis was performed using Kaplan-Meier survival curves and differences were compared by log-rank test. p<0.05 was considered statistically significant as shown in Figure 1.
Results
Total of 89 patients met the criteria for the present study (4 female, 85 male) was evaluated retrospectively. The mean age of the patients was 65 (ranged from 39 to 83). The mean follow-up period was 28.7 (12-78) months. The patients were divided into two groups according to the presence of the recurrence and progression (seen in 31 men and 2 women) and absence of these (54 men and 2 women) after BCG treatment. As shown in Table 1, there was no significant difference in terms of age, gender, tumour stage, tumour grade and tumour size between two groups (p=0.35 and p=0.58, p=0.15 and p=0.39, p=0.07; respectively). During follow-up, the tumour of 9 patients became muscle-invasive. The pathological evaluation of three patients was noted as muscle invasive without the signs of invasion at the tumour base, and the rest was reported as non-muscle invasive bladder tumours. Radical cystectomy had been offered to the patients with muscle invasive tumour but none of them accepted this surgery. After initial transurethral resection, no macroscopic tumour was detected in any, during follow-up. Pathologies of the first 3 of these patients had come to muscle-invasive and tumour base was reported as negative. It's one of the patients was 4 months of diagnosis underwent radical cystectomy and pathology was reported as pT2 No. Other first pathology of the patients who underwent radical cystectomy pTa- High Grade (HG) 1 patient, 2 patients pTa-HG+CIS, the CIS+pT1-HG 2 patients, 1 patient and CIS pTa-Lowe Grade.
| Characteristic | All patient N:89 |
Group-1 N:56 |
Group-2 (recurrent disease) N:33 | HR | P<0.05 |
|---|---|---|---|---|---|
| Age | 65 (39-83) | 65 (39-83) | 63 (41-81) | 0.97 (0.92-1.01) | 0.35 |
| Male Female |
85 (95.5%) 4 (4.5%) |
54 (96.4%) 2 (3.6%) |
31 (93.9%) 2 (6.1%) |
1.75 (0.23-13.23) | 0.58 |
| T stage Ta T1 T2 |
52 (58%) 34 (38.2%) 3 (3.3%) |
33 (58.9%) 23 (41%) - |
19 (57.5%) 11 (33.3%) 3 (9%) |
1.88 (0.81-4.39) | 0.15 |
| Grade High grade(HG) Lower grade(LG) |
73 (82%) 16 (18%) | 44 (78.5%) 12 (21.5%) | 29 (87.8%) 4 (12.2%) | 0.18 (0.02-1.53) | 0.39 |
| Ta-LG Ta-HG T1-LG T1-HG T2-HG |
9 (10.1%) 43 (48.3%) 7 (7.8%) 27 (30.3%) 3 (3.3%) |
6 (10.7%) 27 (48.2%) 6 (10.7%) 17 (30.3%) - |
3 (9%) 16 (48.4%) 1 (3%) 10 (30.3%) 3 (9%) |
||
| CIS yes no |
15 (16.8%) 74 (83.2%) |
5 (8.9%) 51 (91.1%) |
10 (30.3%) 23 (69.7%) |
4,43 (1.36-14.44) | 0.009 |
| Tumour size Tm 3cm≥ Tm<3cm |
16 (17.9%) 73 (82.1%) |
13 (23.6%) 42 (76. 4%) |
3 (8.8%) 31 (91.2%) |
0.40 (0.04-3.78) | 0.07 |
| NLR | 2.68 ± 0.22 | 3.44 ± 0.27 | 0.04 | ||
| NLR>2,5 | 48 (65.1%) | 23 (58.9%) | 25 (75.6%) | 4.48 (1.72-11.68) | 0.0021 |
| RDW | 14.43 ± 3.05 | 14.04 ± 1.81 | 0.51 | ||
| MPV | 8.93 ± 1.16 | 8.3 ± 0.7 | 0.52 (0.32-0.86) | 0.009 | |
| PLR | 177.20 ± 19.9 | 179.97 ± 9.7 | 0.91 | ||
| Smokers | 85 | 53 | 32 | ||
| Current smokers | 17 | 8 | 9 | ||
| Occupational exposure | 1 | - | 1 |
Table 1: Clinical characteristics of study cohort.
The average time to go to radical surgery, 10.8 ± 4.2 (3-36) was the month. Radical cystectomy was performed in 7 of them; however, the remaining 2 patients unsuitable for the surgery due to their age and general health status had radiotherapy. The mean time to recurrence in the 33 (34.3%) patients who experienced a recurrence was 10 months (range, 3-39 months). The rates of recurrence and progression were 34% and 1%, respectively. Moreover 27% of the patients who had tumour recurrence also had progression of the disease. The mean follow-up period for the patients was 21.8 ± 12.86 months (range, 4-72 months).
In comparison of the parameters of preoperative complete blood count (CBC) of two groups, NLR was found as significantly high in group 2 regardless of the presence of MPV and carcinoma in-situ (Table 2). Values of NLR and MPV of patients progressed to muscle invasive disease.
| Variable | OR | 95% Cl | P<0.05 |
|---|---|---|---|
| Cis | 5.30 | 1.41-19.93 | 0.013 |
| MPV | 0.56 | 0.33-0.96 | 0.037 |
| NLR>2,5 | 4.90 | 1.68-14.28 | 0.003 |
Table 2: Results of univariate and multivariate regression models.
Discussion
Up to now, several biomarkers have been developed to be used in bladder tumour, but a few of them are used in current practice. On the other hand none of them has high sensitivity and specificity to predict the prognosis of bladder tumour [10].
It was demonstrated in gastrointestinal and kidney tumours that preoperative NLR, which is easy to determine with a simple calculation and use in daily practice, has a value in predicting the disease-free survival of patients [11]. Not only in tumours, could this ratio also be used in chronic events or as an index of cellular immune response. Although NLR does not provide an accurate predictive value, it may give information about disease progression.
Cancer is known to have various effects on peripheral blood cells such as erythrocytes, leukocytes and platelets [11]. However, the cause of increase in number of neutrophils and monocytes remains unclear. That increase in number of leukocytes can partly be explained by cytokines [11]. In malignant tumours of epithelial origin and stomach, liver, colon, lung, pancreas, oesophagus, bladder and gallbladder the presence of chronic inflammation has been reported in many studies [12-14]. Although the underlying mechanism is unknown, it had been suggested that activated monocytes and neoplastic tissues are the reasons for toxic granular inflammation in neutrophils [15-17]. In addition, inflammatory effects of certain types of cancers and chronic diseases, and their effects on neutrophils are demonstrated in many studies [18,19].
Development and progression of epithelial malignancies, such as oesophageal cancer, intestine, stomach, prostate, thyroid, liver, breast and bladder cancers, triggers chronic inflammation, which leads to an increase in leukocyte counts [12-14]. Margalis et al. demonstrated that the count of neutrophil, monocyte and leukocyte in the patients with endometrial cancer was higher when compared with healthy individuals [14]. In the related studies, it was concluded that cyclooxygenase-2 (COX-2), prostaglandin E2 (PGE2) and kappa B (NF-kB) had an important role in the inflammatory process. Similar results were also demonstrated in the different types of gynaecologic cancers [17,20,21]. Moreover it has been reported that an increased neutrophil count could be a strong and independent prognostic factor to predict the recurrence and cancer-specific overall survival in head and neck, and kidney tumours [22-24].
It has been established that in muscle-invasive bladder cancer, preoperatively measured neutrophil-lymphocyte ratio and platelet count have predictive value [19]. In another study stated muscle-invasive bladder cancer demonstrated that age, female gender, preoperative NLR in the peripheral blood and platelet count have predictive value on disease-free survival and rapid progression of the disease [25]. In our study, preoperative NLR, MPV and accompanying carcinoma in situ (CIS) detected in the initial cystoscopic evaluation were found to have a statistical meaningfulness to predict the relapse after BCG therapy. On the other hand, there was no significant relationship between preoperative PLR and RDW values and tumour recurrence after BCG therapy in the present study.
The significance of relationship between increased number of neutrophils and poor prognosis of cancer has not been widely accepted. In the contrary, in some studies, it was reported high neutrophil levels were found to be associated with improved out comes in gastric and low-grade prostate cancers [26]. Short follow-up period and limited number of the patients are the disadvantages of this study.
PLR bladder cancer patients before treatment of the prognostic value so far rarely been investigated. High PLR There are studies showing that the value associated with distant metastasis and poor prognosis in certain cancer patients next [27,28]. This pre-treatment studies showing otherwise have a relationship between PL and pathological features and prognosis of bladder cancer [9,29]. However, we did not find an association between bladder cancers with preoperative PLR. PLR pre-treatment prognostic value in bladder cancer studies that prove scarce, there may not be right for such a prediction PLR. The exact relationship between bladder cancer and elucidated with PLR with a greater number of patients it must be questioned in more detail by searching accuracy.
MPV when it comes to eating is an indicator of platelet volume. MPV increasing role in the homeostasis process indicate the presence of the following young populations are more active metabolic and enzymatic plate. Tumour patients that inflammation may be a reflection of the growing MPV continued and increased levels of cytokines, particularly IL-6 may be associated with. In addition, MPV values measured in a study with cancer surgical resection of tumour burden not only effective, they also show that after the operation decreased suggesting that alleviate inflammatory processes related to cancer. Thus, regardless of the MPV TNM staging may be used after surgical resection of the recurrent tumour is thought to be monitored [27]. We have found the MPV values lower in patients with BCG recurrent.
In this study we concluded that preoperative NLR, MPV or presence of CIS in the initial evaluation could be used as an independent marker to predict tumour recurrence after BCG therapy. For more precise consequences, the comprehensive studies with larger patient groups and longer follow-up periods are needed.
References
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010; 127: 2893-2917
- Burger M, Catto JW, Dalbagni G, Grossman HB, Herr H, Karakiewicz P. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013; 63: 234-241.
- Heney NM, Ahmed S, Flanagan MJ, Frable W, Corder MP, Hafermann MD, Hawkins IR. Superficial bladder cancer: progression and recurrence. J Urol. 1983; 130: 1083-1086.
- Babjuk M, Burger M, Zigeuner R, Shariat SF, van Rhijn BW, Compérat E. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2013. Eur Urol. 2013; 64: 639-653.
- Prescott S, James K, Hargreave TB, Chisholm GD, Smyth JF. Intravesical Evans strain BCG therapy: quantitative immune histochemical analysis of the immune response within the bladder wall. J Urol. 1992; 147: 1636-1642.
- Taniguchi K, Koga S, Nishikido M, Yamashita S, Sakuragi T, Kanetake H, Saito Y. Systemic immune response after intra vesical instillation of bacilleCalmette-Guérin (BCG) for superficial bladder cancer. ClinExpImmunol. 1999; 115: 131-135.
- Lin GN, Peng JW, Liu PP, Liu DY, Xiao JJ, Chen XQ. Elevated neutrophil-to-lymphocyte ratio predicts poor outcome in patients with advanced non-small-cell lung cancer receiving first-line gefitinib or erlotinib treatment. Asia Pac J ClinOncol. 2014.
- Millan-Rodriguez F, Chechile-Toniolo G, Salvador-Bayarri J, Palou J, Algaba F, Vicente-Rodríguez J. Primary superficial bladder cancer risk groups according to progression, mortality and recurrence. J Urol. 2000; 164: 680-684.
- Ohno Y, Nakashima J, Ohori M, Hatano T, Tachibana M. Pre-treatment neutrophil-to-lymphocyte ratio as an independent predictor of recurrence in patients with non-metastatic renal cell carcinoma. J Urol. 2010; 184: 873-878.
- Xylinas E, Kluth LA, Lotan Y, Daneshmand S, Rieken M, Karakiewicz PI, Shariat SF. Blood and tissue-based biomarkers for prediction of outcomes in urothelial carcinoma of the bladder. Urol Oncol. 2014; 32: 230-242.
- Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008; 454: 436-444.
- Ardies CM . Inflammation as cause for scar cancers of the lung. Integr Cancer Ther. 2003; 2: 238-246.
- Wislez M, Rabbe N, Marchal J, Milleron B, Crestani B, Mayaud C. Hepatocyte growth factor production by neutrophils infiltrating bronchioloalveolar subtype pulmonary adenocarcinoma: role in tumour progression and death. Cancer Res. 2003; 63: 1405-1412.
- Margolis KL, Rodabough RJ, Thomson CA, Lopez AM, McTiernan A; Women's Health Initiative Research Group. Prospective study of leukocyte count as a predictor of incident breast, colorectal, endometrial, and lung cancer and mortality in post-menopausal women. Arch Intern Med. 2007; 167: 1837-1844.
- Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002; 420: 860-867.
- Nathan C. Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol. 2006; 6: 173-182.
- Fridlender ZG, Albelda SM. Tumour-associated neutrophils: friend or foe? Carcinogenesis. 2012; 33: 949-955.
- Tasoglu I, Sert D, Colak N, Uzun A, Songur M, Ecevit A. Neutrophil-Lymphocyte Ratioand the Platelet-Lymphocyte Ratio Predict the Limb Survival in Critical Limb Is chemia. ClinApplThrombHemost. 2013; 20: 645-650.
- Kaynar M, Yıldırım ME, Badem H, Caviş M, Tekinarslan E, Istanbulluoğlu MO. Bladder cancer invasion predictability based on preoperative neutrophil-lymphocyte ratio. Tumour Biol. 2014; 35: 6601-6605.
- Cho H, Kim JH. Multiplication of neutrophil and monocyte counts (MNM) as an easily obtain able tumour marker for cervical cancer. Biomarkers. 2009; 14: 161-170.
- Cho H, Hur HW, Kim SW, Kim SH, Kim JH, Kim YT, Lee K. Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer ImmunolImmun other. 2009; 58: 15-23.
- Jensen HK, Donskov F, Marcussen N, Nordsmark M, Lundbeck F, von der Maase H. Presence of intra tumoral neutrophils is an independent prognostic factor in localized renal cell carcinoma. J ClinOncol. 2009; 27: 4709-4717.
- Ceylan C, Camtosun A, Doluoglu OG, Tasdemir S, Keles I, Aglamis E, Tatar CA. Emphasis of neutrophil-to-lymphocyte ratio in non-metastatic renal cell carcinoma. Urologia. 2014; 81:51-56.
- Trellakis S, Farjah H, Bruderek K, Dumitru CA, Hoffmann TK, Lang S, Brandau S. Peripheral blood neutrophil granulocytes from patients with head and neck squamous cell carcinoma functionally differ from their counter parts in healthy donors. Int J ImmunopatholPharmacol. 2011; 24: 683-693.
- Can C, Baseskioglu B, Yılmaz M, Colak E, Ozen A, Yenilmez A. Pre-treatment Parameters Obtained from Peripheral Blood Sample Predicts Invasiveness of Bladder Carcinoma. Urol Int. 2012; 89: 468-472.
- Caruso RA, Bellocco R, Pagano M, Bertoli G, Rigoli L, Inferrera C. Prognostic value of intratumoral neutrophils in advanced gastric carcinoma in a high-risk area in northern Italy. Mod Pathol. 2002; 15: 831-837.
- Kilincalp S, Coban S, Akinci H, Hamamc M, Karaahmet F, Coskun Y. Neutrophil/lymphocyteratio, platelet/lymphocyteratio, and mean platelet volume as potential biomarkers for early detection and monitoring of colorectal adenocarcinoma. Eur J Cancer Prev. 2015;24:328–333.
- Cannon NA, Meyer J, Iyengar P, Ahn C, Westover KD, Choy H. Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors following stereotactic radiation therapy for early-stage non-small cell lung cancer. J ThoracOncol. 2015; 10: 280–285
- Zhang GM, Zhu Y, Luo L, Wan FN, Zhu YP, Sun LJ, Ye DW. Preoperative lymphocyte-monocyte and platelet-lymphocyte ratios as predictors of overall survival in patients with bladder cancer undergoing radical cystectomy. Tumour Biol. 2015.