- Biomedical Research (2015) Volume 26, Issue 4
Determination of the normative values of the masseter muscle by singlefiber electromyography in myasthenia gravis patients
Lei Shi1, Hengfang Liu1, Min Zhang1, Yapei Guo1, Bo Song2, Changdong Song1, Dandan Song1,Yuming Xu2*
1Department of Neurology, the Fifth Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan, China
2Department of Neurology, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan, China
- *Corresponding Author:
- Yuming Xu
Department of Neurology
The First Affiliated Hospital of Zhengzhou University
No. 19 People Road
Zhengzhou 450000, Henan
China
Accepted August 13 2015
Abstract
The purpose of this study is to obtain normative values of the masseter muscle of myasthenia gravis (MG) patients and healthy volunteers by single-fiber electromyography (SFEMG). Stimulation of SFEMG in the masseter muscle was studied in 15 healthy volunteers (men 8, women 7; mean age 40.2, range 21-77) and 30 patients affected by MG (men 16, women 14; mean age 42.8, range 12-75). The mean consecutive difference (MCD) of the individual fiber and the mean MCD per study were determined in the normal group. We recommend the upper normal limit for the individual fibers of jitter and the mean MCD per study in the healthy Chinese adults of 33 μs and 22 μs respectively. Furthermore, in the MG group, the percentage of jitter > upper normal limit jitter and the impulse blocking percentage were detected, which were all significantly different compared to the normal control group (P < 0.01). The overall sensitivity was 90%, with the abnormality in 6 of the 9 ocular MG patients and 100% abnormality in the generalized MG patients. The masseter muscle SFEMG has a high degree of sensitivity. The masseter should be considered for SFEMG in the diagnosis of MG, and added routinely to the tested muscles.
Keywords
Single-fiber electromyography, masseter muscle, myasthenia gravis.
Introduction
Myasthenia gravis (MG) is a neuromuscular junction dysfunction caused by autoimmune disease [1]. And more than half of the patients were associated with thymic hyperplasia [2], and surgery may be the first choice [3]. And most of the cases would recover and got a good prognosis with timely treatment [4]. Recently, there is an increased prevalence of MG among rural male adults, which may has a possible association with agricultural pesticides exposure [5]. Among all the diagnose methods, single-fiber electromyography (SFEMG) is known to be the most sensitive diagnostic tool for MG [6,7]. In some series, the sensitivity of SFEMG was up to 100% [8,9]. However, the extremely high sensitivity of it has now recently challenged, particularly in seronegative cases [10,11]. Meanwhile, in some neuropathies and radiculopathies patients with the abnormalities of nerve which was caused by other diseases rather than MG, the specificity of SFEMG was still need to be confirmed [12]. So how to define the neuromuscular transmission function of all the cases above promoted more researchers to get the normal value by the useage of SFEMG.
In previous studies, the masseter muscle is considered to be suitable to take as a test standard for SFEMG since it is easy to attach and safe to examine, and the most important reason is that it is often involved in disorders of neuromuscular transmission [13,14], even from the very early stages, which meant that the masseter muscles should be the best choice for the research of this kind. Although no Chinese data was given about the normal value of masseter muscle based on SFEMG, which caused there was no possibility of clinical research that could be done to gain any return or diagnosis criteria that could be define, our study, were to collect normative values for jitter in the masseter of Chinese healthy adults and perform stimulated SFEMG (SSFEMG) of the masticatory muscles in patients referred with MG to assess the normal value as well as to know the significance of this methodology.
Materials and Methods
Clinical information
Fifteen healthy volunteers (men 8, women 7; mean age 40.2, range 21-77) without neurological and any other health problem from the physical examination department in the Fifth Affiliated Hospital of Zhengzhou University were recruited in this study to form the control group. Thirty patients diagnosed as MG (men 16, women 14; mean age 42.8, range 12-75) from the neurological department in the Fifth Affiliated Hospital of Zhengzhou University were included as the MG group, the diagnosis criteria as follows: 1) major criteria: any manifestation of fatigability or weakness; 2) minor criteria: “amplitude decrement >10% on repetitive nerve stimulation (RNS) test” or “any abnormal SFEMG findings in a muscle other than masseter” or “positive anti-acetylcholine receptor (AChR) antibodies” or “positive edrophonium test”, all the cases should have the major manifestation and any but at least 2 of the minor criteria.
Meanwhile, the muscle-specific tyrosine kinase (MuSK) antibody testing was not a necessary standard which should be got routinely available, and the clinical presentation of severity of MG was classified according to the published Ossermann standards [15]. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Zhengzhou University. Written informed consent was obtained from all participants.
SFEMG measurements and the abnormal standard of SFEMG
Stimulated jitter was investigated in the masseter according to the previously reported technique [16]. The recording SFEMG needle was introduced into the area of the muscle twitching, anterior to the cathode to avoid blood vessels passing behind the masseter. Stimulation was performed at a frequency of 10 Hz when the electrode positions were achieved. Stable single-fiber potentials were analyzed with amplitudes over 0.2 mV and with a rise time shorter than 0.3 ms and with a wellformed negative peak at a bandpass of 1-10 kHz. Jitter was obtained as the mean consecutive difference (MCD) for each fiber for a series of 50 responses.
.The judgment of abnormal SFEMG was made if any of the following criteria was met: abnormal values or blocking in more than 10% of the fibers studied or a mean MCD per study exceeding the upper limits of the normal value [17].
Statistical analysis
Statistical analysis of all data was performed using SPSS software. The differences between the mean values of the groups were compared by the ANOVA test or Chi-square test according to the measurable or enumerable properties of the data.
Results
Clinical information
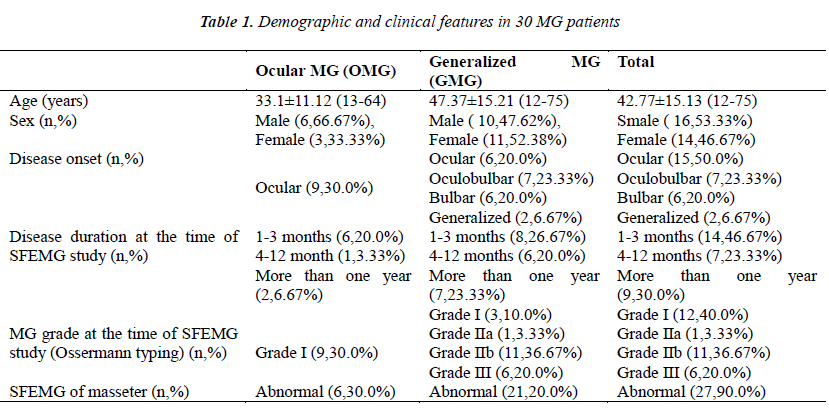
Demographic features and the basic clinical findings of the MG patients are summarized in Table 1, which showed the differences between different types of MG.
SFEMG findings of the normal control group
In total, 30 MG patients but we found it difficult for 3 patients to tolerate the examinations for some reasons, which limited us to study fewer than the ideal 20 fibers.
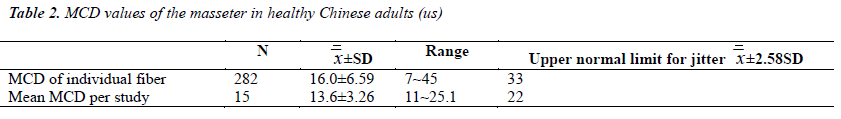
We have obtained a total of 282 single-fiber potentials between 12 and 28 per muscle. The examinations of three MG patients were stopped after recording 12 fibers because the patients were not feeling well. From the remaining patients at least 20 potentials were collected. The mean MCD of the individual fibers ranged between 7 and 45 μs, with a mean value of 16.00 μs and a SD 6.59 μs. Furthermore, the mean MCD per study ranged from 11.0 to 25.1 μs, with a mean of 13.6 μs and a SD 3.26 μs. The upper normal limit for jitter of individual fibers and for the mean MCD per study is defined as the 99th percentile. In our study, the two indexes each were 33 and 22 μs. We recommend these two values as the bounds of normality of the masseter of healthy Chinese adults (Table 2).
Comparison of the SFEMG findings
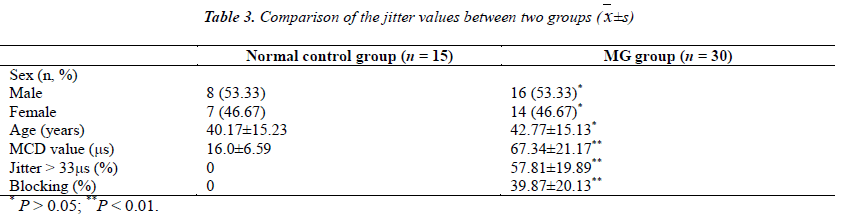
The results of the SFEMG findings of the MG group are presented in Table 1, and the results of the healthy Chinese adults are presented in Table 2. In Table 3 we show the comparison of these two groups. Twenty-seven patients had abnormalities in the masseter muscle and the overall sensitivity was 90.0%. The positive detection rate of ocular MG (OMG) and generalized MG (GMG) were 7% (6/9) and 100% (21/21) respectively, and there was no statistical difference between the detection rate of these two MG types (P > 0.05). The three normal results were found among patients with ocular MG, where the sensitivity was 67%.
Statistical analysis of the sex and age values indicated that there was no significant difference between the two groups (P > 0.05). The mean MCD of the MG group was 67.34 μs (SD 21.17 μs), which was significantly different compared with the normal control group (P < 0.01). The mean percentage of jitter is >33 μs and the mean impulse blocking percentage were 57.81% and 39.87% respectively, while in the normal control group these two values are all 0. The mean jitter and the impulse blocking percentage were significantly different between the two groups (P < 0.01).
Discussion
SFEMG has been known to be the most sensitive diagnostic procedure for the diagnosis of MG for many years [6,7]. Using this detection method, the abnormal neuromuscular transmission can be easily found in an early stage, before impulse blocking or clinical weakness appearce. However, in the recent studies, people found that it is not specific, for example, in the radiculopathies and neuropathies, the specificity of SFEMG has been questioned [6,7]. Therefore, it is advisable to search for a kind of muscle that is easily and safely accessible and is highly sensitive.
To our knowledge, the masseter muscle seems to fulfill these requirements, and seems to be suitable for the SFEMG detection. Overall, the masseter muscle was receiving much greater attention in the SFEMG studies because of its characteristics, but we never found correlative studies about the masseter muscle in China. In this study we collected the normative values for jitter in the masseter of healthy Chinese adults and performed stimulated SFEMG (SSFEMG) of the masticatory muscles in patients referred with myasthenia gravis to assess the significance of this methodology.
In 6% of the myasthenic patients an early fatigue on the masseter muscle occurs, and this muscle is usually involved in most patients in the later period of the disease, with frank weakness and atrophy developing in 15% [18]. Furthermore, the masseter muscle presented the highest degree of abnormality compared to the facial, trapezius, or limb muscles [19-21]. Overall, we decided to obtain the control values of the masseter muscle in the SFEMG detection which can be used for further clinical researches. The stimulated jitter values that were obtained in the masseter are similar with the facial muscles, because the masseter resembles most closely in size and length of the fiber, and is similar to the a broad studies results [14]. In our study, we recommend the upper normal limit for jitter of individual fibers and the mean MCD per study of healthy Chinese adults as 33 μs and 22 μs respectively, which is comparable with other studies, 30 μs and 21 μs.
Our results confirm the high specificity of SFEMG when performed on the masseter muscle in the MG patients, and we found a high frequency of stimulated SFEMG abnormalities in the masseter muscle in a series of MG patients. From our results, the high sensitivity of masseter in MG is consistent with the findings in other craniofacial muscles by stimulation SFEMG method, for example in frontalis and orbicularis oculi [22]. Due to sharing the common origin and contiguous with the other craniofacial muscles in the anatomically, the sensitivity usually is expected over 90.0% of these muscles in MG patients. The positive detection rate in OMG is only 66.67% in the nine patients with ocular MG, which was a little low sensitivity. This result maybe has relationship with the small detection number, and the early investigation timing, which make it difficult to make definite conclusion about the value of masseter SFEMG in the diagnosis of ocular MG. Statistical analysis of the mean MCD, mean percentage of jitter >33 μs and the mean impulse blocking percentage values were all significantly different between normal control group and the MG group (P < 0.01), which indicated the high sensitivity of masseter SFEMG in MG.
In addition, from a technical viewpoint, stimulated SFEMG investigation method of the masseter is easy and accessible, because the location of masseter is superficial and clearly locate. Furthermore, most patients could tolerate this technique, which is much better than sampling of the orbicularis oculi or frontalis muscles.
In conclusion, the masseter muscle is suitable for SFEMG in MG patients, this method is not only easily investigated, but it also has a high degree of sensitivity. We suggest that the masseter muscle could be studied routinely in patients which are suspected to have a neuromuscular transmission disorders, and the masseter SFEMG may be of value in the diagnosis of these diseases.
Conflict of Interest
All authors have no conflict of interest regarding this paper.
References
- Turakhia P, Barrick B, Berman J. Patients withneuromuscular disorder. Med Clin North Am 2013; 97:1015-1032.
- Weiss JM, Cufi P, Le Panse R, Berrih-Aknin S. The thymus in autoimmune Myasthenia Gravis: Paradigm for a tertiary lymphoid organ. Rev Neurol (Paris) 2013; 169: 640-649.
- El Hammoumi M, Arsalane A, El Oueriachi F, Kabiri el H. Surgery of myasthenia gravis associated or not with thymoma: a retrospective study of 43 cases. Heart Lung Circ 2013; 22: 738-741.
- Andersen JB, Owe JF, Engeland A, Gilhus NE. Total drug treatment and comorbidity in myasthenia gravis: a population-based cohort study. Eur J Neurol 2014; 21: 948-955.
- Nemet AY, Kaiserman I, Mimouni M, Segal O, VinkerS. High prevalence of myasthenia gravis among rural adult populations. JClinNeuromuscul Dis 2014; 16: 47-50.
- AAEM Quality Assurance Committee and American Association of Electrodiagnostic Medicine. Literature review of the usefulness of repetitive nerve stimulation and single fiber EMG in the electrodiagnosticevaluation of patients with suspected myasthenia gravis or Lambert–Eaton myasthenic syndrome. Muscle Nerve 2001; 24: 1239-1247.
- Sanders DB. Clinical impact of single-fiber electromyography. Muscle Nerve 2002; 11: S15-S20.
- Padua L, Caliandro P, Di Iasi G, Pazzaglia C, CiaraffaF, Evoli A. Reliability of SFEMG in diagnosing myasthenia gravis: sensitivity and specificity alculated on 100 prospective cases. ClinNeurophysiol 2014;125: 1270-1273.
- Katzberg HD, Bril V. A comparison of electrodiagnostic tests in ocular myasthenia gravis. J ClinNeuromuscul Dis 2005; 6: 109-113.
- Nemoto Y, Kuwabara S, Misawa S, Kawaguchi N, Hattori T, Takamori M, Vincent A. Patterns and severity of neuromuscular transmission failure in seronegativemyasthenia gravis. J NeurolNeurosurg Psychiatry 2005; 76: 714-718.
- Sanders DB, El-Salem K, Massey JM, McConville J, Vincent A. Clinical aspects of MuSK antibody positive seronegative MG. Neurology 2003; 60: 1978-1980.
- Katirji B, Kaminski HJ. Electrodiagnostic approach to the patient with suspected neuromuscular junction disorder.NeurolClin 2002; 20: 557-586.
- Orhan EK, Deymeer F,Oflazer P, Parman Y, Baslo MB. Jitter analysis with concentric needle electrode in the masseter muscle for the diagnosis of generalized myasthenia gravis. ClinNeurophysiol 2013; 124: 2277- 2282.
- Khuraibet AJ, Rousseff RT, Behbehani R, al-ShubailiAF, Khan RA. Single-fiber electromyography of masseter muscle in myasthenia gravis. Muscle Nerve 2008; 37: 522-525.
- Padua L, Galassi G, Ariatti A, Aprile I, Caliandro P, Evoli A, Pazzaglia C, Tonali P. Myasthenia gravis selfadministeredquestionnaire: development of regional domains. NeurolSci 2005; 25: 331-336.
- Rousseff RT, Khuraibet AJ, Al-Shubaili AF, TzvetanovP. Stimulated jitter in the masseter muscle: normative values. Muscle Nerve 2007; 35: 243-245.
- Gawe? M, Domitrz I, Domitrz W, Szmidt-Sa?kowska E, Kami?ska A. Impairment of neuromuscular transmission in transient global amnesia-Does it reallyexist? NeurolNeurochir Pol 2014; 48: 337-341.
- Keesey JC. Clinical evaluation and management of myasthenia gravis. Muscle Nerve 2004; 29: 484-505.
- Pavesi G, Cattaneo L, Tinchelli S, Mancia D. Masseteric repetitive nerve stimulation in the diagnosis of myasthenia gravis. ClinNeurophysiol 2001; 112: 1064-1069.
- Tsuda E, Imai T, Hozuki T, Yamauchi R, Saitoh M, Hisahara S, Yoshikawa H, Motomura M, Shimohama S. Correlation of bite force with excitation-contraction coupling time of the masseter in myasthenia gravis. ClinNeurophysiol 2010; 121: 1051-1058.
- Rubin DI, Harper CM, Auger RG. Trigeminal nerve repetitive stimulation in myasthenia gravis. Muscle Nerve 2004; 29: 591-596.
- Valls-Canals J, Povedano M, Montero J, Pradas J. Stimulated single-fiber EMG of the frontalis and orbicularis oculi muscles in ocular myasthenia gravis. Muscle Nerve 2003; 28: 501-503.