Research Article - Current Pediatric Research (2022) Volume 26, Issue 8
Detection of serum vitamin a levels in neonates with bronchopulmonary dysplasia.
Mohamed Shawky Elfarargy1*, Sally El-Sayed Abu-Risha2, Reham Lotfy Younis3
1Department of Pediatrics, College of Medicine, Tanta University, Egypt
2Department of Pharmacology and Toxicology, College of Pharmacy, Tanta University, Egypt
3Department of Physiology, College of Medicine, Tanta University, Egypt
- *Corresponding Author:
- Mohamed Shawky Elfarargy
Department of Pediatrics
College of Medicine
Tanta University
Egypt
E-mail: farargy2009@hotmail.com
Received: 04 August, 2022, Manuscript No. AAJCP-22-68267; Editor assigned: 05 August, 2022, PreQC No. AAJCP-22-68267(PQ); Reviewed: 08 August, 2022, QC No. AAJCP-22-68267; Revised: 15 August, 2022, Manuscript No. AAJCP-22-68267(R); Published: 22 August, 2022, DOI:10.35841/0971-9032.26.8.1609-1613.
Abstract
Background: Bronchopulmonary Dysplasia (BPD) is a serious Chronic Lung Disease (CLD) occurring in neonates mainly in premature infants treated with oxygen and mechanical ventilation. Aim: Detection of the serum vitamin A levels in neonates with BPD. Patient and Methods: A prospective case-control study was done on 40 neonates incubated in NICU of Tanta university hospital suffering from respiratory distress which was diagnosed as BPD (patient group) and 40 healthy neonates with matched gestational age and sex (control group). The study was done from June 2016 to March 2018. A sample of venous blood was taken from infants within the first 3 hours. Serum retinol (RT) levels were resolved utilizing high-performance liquid chromatography. Results: Serum RT levels were significantly lower in cases that developed BPD (patient group) if compared with healthy neonates (control group). The cutoff value of serum RT in neonates with BPD was 0.68 μmol/L with sensitivity and specificity was 96%, 92% respectively. Conclusion: Neonates with BPD are accompanied by a decreased in serum levels of vitamin A and could be used as an early predictor for developing BPD in neonates. Recommendation: vitamin A supplementation to the neonates who are susceptible to develop BPD.
Keywords
Neonate, Vitamin A, Bronchopulmonary dysplasia.
Introduction
BPD is the most common Chronic Lung Disease (CLD) occurring in premature infants treated with oxygen and mechanical ventilation. In BPD, there are many factors can lead to damage of lung tissues either the bronchial tree or the alveolar tissues as a result of the hazardous effect of prolonged O2 exposure and ventilator trauma to the lung tissues which lead to chronic destruction and reduction of the alveoli which result in decrease of the alveolar gas exchange [1].
BPD is a common morbidity affecting newborn especially premature, low birth weight infants. Infants with BPD have high rates of postnatal growth failure with high incidence of mortality either in the neonatal period or later in infancy or childhood [2]. RT deficiency and other nutrients, is a main cause of BPD in neonates especially in preterm. The serum retinol levels in preterm is shown to be less than that present in full term neonates, and the risk for BPD and other CLD is elevated in preterm neonates with decreased retinol serum levels [3,4].
The clinical finding of RT deficiency and BPD are collapse of the alveoli with loss of the cellular lining of these alveoli with necrosis of some respiratory tissues and destruction of the thin alveolar wall with resulting in fibrosis of the lung tissues and loss of the alveolar gas exchange functions [5].
Serum retinol levels are used as an excellent indicator and reflect efficiently the vitamin A status. The liver is the main storage site for retinol, and RT stores are lower in preterm than in full-term neonates [6]. In addition to decreased serum RT levels which reflect the vitamin A status, the carrier protein of the retinol is also lowered in preterm than in full term neonates.
Vitamin A is essential for healthy lung and normally functioning respiratory system and therefore it could protect the lung tissue from hazardous effect of prolonged high levels of O2 and unavoidable traumatic effect of ventilation on some alveoli thus reducing the risk of BPD. Vitamin A is vital for normal respiratory system growth and the healthy integrity of respiratory system. Preterm neonates are liable to reduced vitamin A levels at delivery and this has been accompanied by high risk of BPD. The early administration of vitamin A to preterm is accompanied by decrease in oxygen requirement among those preterm [7]. The aim of this study was detection of the serum vitamin A levels in neonates with BPD.
Patient and Methods
Study population
A prospective case-control study was done on 40 neonates incubated in NICU of Tanta University hospital suffering from respiratory distress which was diagnosed as BPD (patient group)(we started the study with 95 neonates where 1 neonates was died, 2 neonates transferred to another hospital and 52 neonates were not progress to be diagnosed as BPD and excluded from the study), and 40 healthy neonates (who did not develop BPD) with matched gestational age, weight and sex who represented the (control group). The study was carried out from June 2016 to March 2018. The patients group consisting of 40 neonates with BPD, mild, moderate or severe.
Mild BPD is a neonatal treatment with >21% O2 for at least 28 days and the ability to keep in room air without RD at thirty six weeks GA or discharge (in <32 weeks), or and the ability to respire room air without RD at age of >28 d or at discharge (in ≥ 32 weeks). Moderate BPD is a neonatal treatment with >21% O2 for at least 28 days and the ability to keep with <30% O2 without RD at thirty six weeks GA or discharge (in < 32 weeks) or O2 requirement (<30%) at age of >28 d or at discharge (in ≥ 32 weeks). Finally, severe BPD is a neonatal treatment with >21% O2 for at least 28 days and the need for ≥ 30% O2 for normal breathing without RD at thirty six weeks GA or discharge (in <32 weeks) or O2 requirement(≥ 30% ) at age of >28 d or at discharge (in ≥ 32 weeks) [8].
Inclusion criteria: Neonates suffering from BPD whatever its grade, estimation of serum RT was prepared for all newborn in this study within the first 3 hours after delivery and proceeding to any nutrition or therapies.
Exclusion criteria: neonatal sepsis, diseases of the respiratory diseases other than BPD, cardiovascular diseases, or central nervous system diseases, mothers who had vitamin A deficiency, mothers who had taken vitamin A supplementation. This study was approved by the ethics committee of the faculty of medicine, Tanta University. Written informed consent was signed from the parents of all neonates.
Data Collections
History taking, chest and systemic examination. Chest X-ray was done for all studied neonates.
Laboratory Workup
1.0 mL sample of venous blood was obtained from infants within the first 3 hours. Samples were collected in amber micro containers, separated, and stored in the dark at-80 C until analysis. Serum retinol levels were resolved utilizing high-performance liquid chromatography [9].
Statistical analysis
The computer program which had been done for every statistical calculation was SPSS version 21, IBM, Armonk, NY, USA. Data are expressed as mean ± SD, range. The t test was done for group comparisons of normally distributed variables. Chi-square (X2) test for comparison between two groups as regards qualitative data. P < 0.05 was considered as a significant
Results
| Patient group (n=40) | Control group (n=40) | Test | p-value | |
|---|---|---|---|---|
| Gestational age: (weeks) Mean ± SD | 33.99 ± 4.45 | 36.0 ± 4.62 | T: 1.976 | 0.051 |
| Weight:(kg) Mean ± SD | 1.99 ± 0.91 | 2.40 ± 0.96 | T: 1.957 | 0.054 |
| Sex: No. (%) | 24 Male (60%), | 22 Male (55%) | X2: 0.084 | 0.774 |
| 16 Female (40%) | 18 Female (45%) | |||
| Apgar score at 5 minutes Mean ± SD | 4.4 ± 1.2 | 8 ± 0.16 | T: 18.809 | 0.001* |
| Down score Mean ± SD | 6.32 ± 1.10 | 1.98 ± 0.89 | T: 15.339 | 0.001* |
Table 1. Comparative demographic and clinical data of the studied groups. *P: Value is significant if <0.05.
Table 1 showed comparative demographic and clinical data of the studied groups which revealed non-significant differences in gestational age, weight and sex between the patient and control group (P>0.05) while there was significant difference in Apgar score at 5 minutes and Down score between both groups (P=0.001).
| Degrees of BPD | n=40 | % |
|---|---|---|
| Mild | 32 | 80 |
| Moderate | 6 | 15 |
| Sever | 2 | 5 |
Table 2. Degree of BPD in patient group.
Table 2 showed degree of neonates in patient group where there were 32 cases (80%) had mild degree of BPD, 6 cases (15%) had moderate BPD and 2 cases (5%) had grade sever BPD.
| Patient group (n=40) | Control group (n=40) | T test | P-value | |
|---|---|---|---|---|
| Serum retinol (μmol/L) | ||||
| Range: | 0.4 –0.69 | 0.67–1.12 | 6.713 | 0.001* |
| Mean ± SD | 0.55 ± 0.14 | 0.90 ± 0.22 |
Table 3. Comparison between the serum retinol levels between the patient and control group. *P: value is significant if <0.05.
Table 3 showed the serum RT levels of the patient and control group where the mean serum RT levels in the patient group was 0.55 ± 0.14 while the mean levels serum RT in the control group was 0.90 ± 0.22 which showed significant difference between the serum RT levels in the patient and control group where the serum RT levels in the BPD neonates (patient group) were significantly lower than the neonates who did not suffered from BPD (control group) (P=0.001).
| Degrees of BPD | Serum retinol (μmol/L)(Mean ± SD) | F test | P-value |
|---|---|---|---|
| Mild BPD | 0.65 ± 0.04 | 10.524 | 0.001* |
| Moderate BPD | 0.55 ± 0.5 | ||
| Sever BPD | 0.44 ± 0.04 |
Table 4. Comparison between the serum retinol levels in different degrees of BPD in the patient group. *P: Value is significant if <0.05.
Table 4 showed the serum RT levels in different degrees of BPD in the patient group which showed that that mean levels of serum RT in the neonates with mild BPD was 0.65 ± 0.04 μmol/l, the mean serum RT levels in the neonates with moderate BPD was 0.55 ± 0.5 μmol/l and the mean levels of serum RT in the neonates with sever BPD was 0.44 ± 0.04 μmol/l which revealed significant differences between the serum levels of RT in different degrees of BPD where the more severity of the BPD the more decrease in the serum RT levels(P=0.001).
| Cutoff (μmol/L) | AUC | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | |
|---|---|---|---|---|---|---|---|
| Retinol (μmol/L) | 0.68 | 0.984 | 96 | 92 | 93 | 95 | 94 |
Table 5. Sensitivity, specificity, cut off value, +ve predictive value, -ve predictive value of serum retinol in BPD.
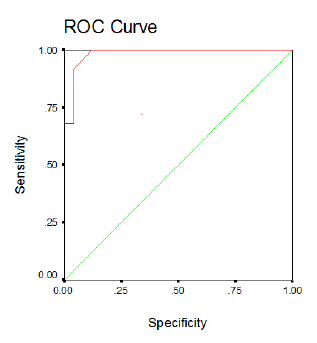
Table 5 and figure 1(ROC curve) Showed the cutoff value of the serum RT levels in cases of BPD was 0.68 μmol/l, the area under the curve was 0.984, the sensitivity was 96% ,the specificity was 92% ,the PPV was 93% ,the NPV was 95% the accuracy was 94%.
Discussion
BPD is a chronic chest disease that occurs in neonates especially in premature neonates due to assisted ventilation and prolonged oxygenation. Prolonged exposure of premature neonates and Very Low Birth Weight (VLBW) to elevated levels of oxygen is accompanied by BPD [10].
This study revealed that the serum retinol levels in the BPD neonates (patient group) were significantly lower than the neonates who did not suffered from BPD (control group) (P=0.001) and there were significant differences between the serum levels of RT in different degrees of BPD where the more severity of the BPD the more decrease in the serum RT levels (P=0.001)
In agreement with the results of this study, there were studies which concluded that retinol deficiency is accompanied by an increased incidence of developing RD, and also the decreased RT is also accompanied by various pulmonary hazards and increased the incidence of neonatal BPD especially in preterm. The results of our study were nearly similar to the results of some studies which stated that nutrient deficiency, particularly RT, is a main cause of BPD in preterm. The RT serum levels in the preterm was found to be less than that present in full term neonates and the risk for BPD is elevated in preterm with decreased RT serum levels which indicated that the importance of decreased RT levels in developing BPD in neonates.
The results of this study were similar to studies that revealed the efficacy of administration of vitamin A in decreasing the incidence of BPD or death in preterm and that supplementation with vitamin A to the neonates is considered as an important and vital preventive management for neonatal BPD. Our study showed that the cutoff value of the serum RT levels in cases of BPD was 0.68 μmol/l, the area under the curve was 0.984, the sensitivity was 96%, the specificity was 92 %, the PPV was 93%, the NPV was 95% the accuracy was 94%.
In agreement with our study, there was a study which found that supplying preterm and VLBW with vitamin A from the first hours of life in an amount that exceeding the routinely given in multivitamin preparation, is accompanied by decrease in BPD and the subsequent neonatal chest problems and decrease the incidence of death in such problems.
The results of this study recommended vitamin A supplementation to the neonates who are susceptible to develop BPD which were similar to some studies which stated that the supplementation of preterm and VLBW with vitamin A from the first hours of life had a very important function in promotion of the healing of the lung tissues after injury by elevated O2 or assisted ventilation and was accompanied by decreased the incidence of developing BPD in the future with better prognosis and decreased mortality in these neonates. Several researches had tried to overcome the decreased levels of vitamin A in neonates with BPD by giving vitamin A supplementation enteral, intramuscular or intravenous.
The recommendation of our study which revealed that the serum RT levels in the BPD neonates (patient group) were significantly lower than the neonates who did not suffered from BPD (control group) (P=0.001) was that supplementation the neonates who are susceptible to develop BPD with vitamin A and this recommendation was the same recommendation of various recent studies which was done in neonates either suffered or susceptible to develop BPD which were stated that vitamin A supplementation has been documented to reduce the incidence of BPD and certain neonatal societies had put it in the guidelines of prevention and treatment of neonatal BPD.
Conclusion
Neonates with BPD is accompanied by decreased in serum levels of vitamin A and could be used as early predictor for developing BPD in neonates.
Recommendation
Vitamin A supplementation to the neonates who are susceptible to develop BPD
Limitation of the Study
The limited number of neonates whatever cases or control in the study, so another studies should be done in the same topic using larger number of neonates to reach an evident conclusion and recommendation.
References
- Greenhill L, Kollins S, Abikoff H, et al. Efficacy and safety of immediate-release methylphenidate treatment for preschoolers with ADHD. J Ame Acad Child Adolesc Psychiatry 2006; 45: 1284-1293.
- https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/cer-203-adhd-final_0.pdf
- Searight HR, Robertson K, Smith T, et al. Complementary and alternative therapies for pediatric attention deficit hyperactivity disorder: A descriptive review. ISRN Psychiatry 2012.
- Catalá-López F, Hutton B, Núñez-Beltrán A, et al. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: A systematic review with network meta-analyses of randomised trials. PloS one. 2017; 12:
- Conners CK, Epstein JN, March JS, et al. Multimodal treatment of ADHD in the MTA: An alternative outcome analysis. J Am Acad Child Adolesc Psychiatry. 2001; 40: 159-167.
- Polanczyk GV, Willcutt EG, Salum GA, et al. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int J Epidemiol 2014; 43: 434-442.
- Faber Taylor A, Kuo FE. Children with attention deficits concentrate better after walk in the park. J attention disorders. 2009; 12: 402-409.
- Berto R. The role of nature in coping with psycho-physiological stress: A literature review on restorativeness. Behavioral sciences. 2014; 4: 394-409.
- Kaplan S. The restorative benefits of nature: Toward an integrative framework. J Environ Psychol 1995; 15: 169-182.
- Lumber R, Richardson M, Sheffield D, et al. Beyond knowing nature: Contact, emotion, compassion, meaning, and beauty are pathways to nature connection. PLoS one 2017; 12: e0177186.