Research Article - Journal of Clinical Ophthalmology (2023) Volume 7, Issue 1
Description of the age-related macular degeneration impact on quality of life from the patients' perspective: OBJETIVO DMAE study
José M Ruiz-Moreno1,2, Luis Arias-Barquet3, Laia Gómez-Baldó4, Carles Blanch5*, José García-Arumí6
1 Department of Ophthalmology, Puerta de Hierro-Majadahonda, University Hospital, Madrid, Spain
2 Department of Ophthalmology, Castilla La Mancha University, Miranza Corporation, Madrid, Spain
3 Department of Ophthalmology, Hospital Universitario de Bellvitge, Universidad de Barcelona, Barcelona, Spain
4 Department of Medical, Novartis Farmacéutica SA, Barcelona, Spain
5 Department of Health Economics, Novartis Farmacéutica SA, Barcelona, Spain
6 Department of Ophthalmology, Hospital Universitari Vall d'Hebron, Barcelona, Spain
- Corresponding Author:
- Dr. Carles Blanch
Department of Health Economics,Novartis Farmacéutica SA, Barcelona, Spain
E-mail: carles.blanch@novartis.com
Tel: +34620033112
Received: 30-Nov-2022, Manuscript No. AACOVS-22-81940; Editor assigned: 02-Dec-2022, PreQC No. AACOVS-22-81940 (PQ); Reviewed: 16-Dec-2022, QC No. AACOVS-22-81940; Revised: 23-Dec-2022, Manuscript No. AACOVS-22-81940 (R); Accepted: 27-Dec-2022; Published: 30-Dec-2022, DOI: 10.35841/aacovs.7.1.614-623
Citation: Ruiz-Moreno JM, Arias-Barquet L, Gómez-Baldó L et al, Description of the age-related macular degeneration impact on quality of life from the patients’ perspective: OBJETIVO DMAE study. J Clin Ophthalmol. 2023; 7(1): 614-623
Abstract
Background: Age-Related Macular Degeneration (AMD) is a leading cause of severe and irreversible central vision loss and legal blindness in populations >50 years old in developed countries. To obtain a complete approach to the disease, it is important to consider the reduction in Health Related QoL (HRQoL) of patients. The purpose of the study is to evaluate the impact of AMD on HRQoL and daily activities from the patients' perspective.
Methods: This was an observational, non-interventional study conducted in Spain to assess the impact of AMD in HRQoL. The final data collection took place over a 6-month period and included telephonic interviews with patient’s ≥ 50 years with diagnosed AMD. HRQoL was measured by the Visual Function Questionnaire (VFQ-25).
Results: A total of 181 patients were included. The greatest limitations were observed in daily living activities in environments unknown to the patient with a total of 48.8% of the patients needing support from a caregiver to perform domestic/housekeeping tasks. AMD showed a great impact on a patient's self-confidence (44.2%), in their mood (39.7%) and anxiety/nervousness (36.5%), with greater psychological impact in neovascular AMD patients.
Conclusion: The loss of vision in AMD patients is important, having a relevant impact on HRQoL. Furthermore, the level of dependence of these patients generates significant indirect costs. Preservation of vision is critical to limit the impact of AMD on the patient’s life.
Trial registration: Ethical Committee of the University Hospital of Bellvitge (ref. EPA041/19), July 11, 2019.
Keywords
Age-related macular degeneration, Dry, Neovascular, Quality of life, Visual function questionnaire.
Introduction
Age-Related Macular Degeneration (AMD) is a leading cause of severe and irreversible central vision loss in populations >50 years old in developed countries and is the main cause of legal blindness (visual acuity<20/200) [1].
In Spain, the estimated AMD prevalence in the population aged 65 years or older is 3.4% (men: 3.6%; women: 3.3%), reaching 8.5% in ≥ 80 years [1]. Given the quickly aging population, these numbers are expected to increase [2]. Recent studies estimate that the AMD prevalence in Europe will increase from 2.7 million people in 2016 to 3.9 million in 2040 [3].
AMD is classified into two subtypes: neovascular AMD (nAMD) and dry AMD [4,5]. Dry AMD in its early stage is characterized by drusen and pigment changes, with minor effects on vision and a slower progression than nAMD [6,5]. nAMD is the most common type (54% of AMD cases), and it is associated with exudative macular neovascularization, causing fluid leaks or hemorrhages, which can result in a rapid and severe loss of central vision, but it can also lead to visual distortion and a loss of contrast sensitivity and color intensity, leading to legal blindness [1,5,7-12] in its spontaneous evolution. Currently, nAMD is the only type of AMD with pharmacological treatment. The introduction of anti-Vascular Endothelial Growth Factor therapies (anti-VEGF) had a significant positive impact on the prevalence of legal blindness due to nAMD [13].
The severity of vision loss is assessed using a combination of objective measures, but the impact of visual impairment is better reflected from the patients' perspective. Patients with similar clinical features may function very differently, experience different levels of impairment, and report disparate values of perceived Quality of Life (QoL) across the physical, mental, emotional, and social domains of functioning [4]. To obtain a complete approach to the disease, it is important to consider the reduction in Health-Related QoL (HRQoL) in terms of mobility, personal independence, driving and reading ability [2,14-16].
Visual impairment could also affect performance at work and social activities, as well as being the cause of premature retirement and further impairment of daily activities [15,16]. Usually, AMD patients are likely to suffer from depression due to isolating themselves and disconnecting from activities they previously enjoyed and due to an increased need for care [5]. Furthermore, AMD has negative effects due to its impact on the social and economic participation of patients in society (ability to work and manage in society) [5]. This burden extends to social welfare systems, community services, caregivers, and patients’ families [5]. Thus, the burden on the caregiver can also be substantial, and AMD has been shown to have emotional, physical, and occupational effects on caregivers [13,17].
Although the literature about AMD is extensive, most of the information focuses on physical aspects (treatment options, incidence, and progression of the disease) [18]. Data on nAMD patient perceptions and preferences are therefore important, and little research has so far been done into general patient attitudes towards nAMD, treatment expectations and fears [18,19].
Understanding patients’ experiences could help physicians, other health professionals and social and health institutions’ structure and prioritize the needs and management of patients. In this context, the present study aims to provide knowledge not only about the experience of Spanish patients with AMD treatment, their health care and HRQoL, but also about the impact of AMD on their lives through the difficulties that patients encounter in their daily life and their expectations and fears.
Materials and Methods
Study design and population
This was an observational, non-interventional and cross-sectional study based on a telephone interview with AMD patients conducted in Spain.
Patients learned that the study was being conducted through patients’ associations, pensioners' organizations, online and radio advertisements and/or informative leaflets available at the retina units of 10 hospitals of different regions, representing regional variability. The information included the study objective, the promoter’s name, how the responses would be used, and the details related to the patients’ participation (voluntary participation through a telephone interview, anonymity, ensuring confidentiality, the approximate duration, and the way to contact the interviewers).
The study was carried out in patients diagnosed with AMD (dry or neovascular) who voluntarily decided to contact. Before starting the interview, the interviewers ensured that the patient had agreed to participate in the study by giving oral consent and verified that the patient met all the selection criteria. Researchers did not directly participate in the inclusion of the patients in the study. Patients who contacted the interviewers and were interested in participating in the study were consecutively included.
Although the interviews were scheduled to take place over a 4-month period, the final data collection period was 6 months.
The inclusion criteria comprised adult patients ≥ 50 years with a confirmed diagnosis of AMD (dry or neovascular) who provided oral informed consent to participate. Patients participating in any other clinical study and/or other telephone interview on AMD were excluded.
The study variables were collected during the telephone interview. The responses to the interview, excluding personal data such as name or telephone number, were recorded and included in an ad hoc electronic Case Report Form (eCRF) specifically designed for this study. The blocks included in the interview were as follows:
Block 1: Sociodemographic profile.
Block 2: clinical data, patient journey and use of resources.
Block 3: psychological impact, satisfaction, and expectations.
Block 4: HRQoL.
Block 5: social impact/information received.
Study endpoints
The main endpoint was obtained by a qualitative description of the responses to the different sections of the interview to assess the impact of AMD on HRQoL and daily activities from the patients' perspective, including the following:
• Visual Function Questionnaire (VFQ-25) [20], (adapted and validated to the Spanish population) [21], analyzing: VFQ-25 total score; the score for each VFQ-25 subscale (general vision, eye damage, activities with near and far vision, social functioning, mental health, difficulties in performing the patient’s role and dependence) and the percentage of patients for each response to each item in VFQ-25. Their scores range from 0-100 points, with higher scores indicating better visual function.
• The impact of AMD on daily activities was analyzed using the percentage of patients with different degrees of limitation and the frequency with which they needed help due to AMD to perform the following daily activities: personal care, moving around the house, housework, attending a medical appointment, moving outside the house (to both familiar or unknown places/routes), shopping (choose and/or pay for products), using public transport (familiar/new routes), remember to follow the treatment and/or go to clinical visits.
Secondary endpoints described the patients’ characteristics, their healthcare and the psychological and impact of AMD on daily life. Secondary variables were as follows:
• AMD patient profile- sociodemographic and clinical characteristics, including concomitant diseases and eye diseases other than AMD.
• AMD symptoms, treatment, patient journey and use of resources (direct healthcare and non-healthcare and indirect resources).
• Psychological impact, patient satisfaction with treatment and assistance received, and expectations about the prognosis of the disease.
• Opinion of the patients on the information received about their disease (at the time of diagnosis, if more information is required, etc.), the AMD impact on social and family environment and loss of autonomy (limitations in daily living activities and how often they needed help due to AMD).
Statistical analysis
As it was a descriptive and exploratory analysis, the sample size was calculated according to statistical criteria. Using the maximum indeterminacy criteria, the estimated percentage was expected to be approximately 50% in a category of a categorical variable.
A sample of 385 evaluable patients would be enough to estimate a population percentage of 50%, with a 95% confidence interval (95% CI) of ± 5 percentage units. In this way, continuous variables could be estimated with a precision of 0.1 standard deviations (SD). Considering that approximately 10% of the patients would not have evaluable data, it was estimated that 428 AMD patients should be included in the study, considering as evaluable those patients who completed at least one section of the interview. However, despite the extension of the recruitment period (from 4 to 6 months), the expected number of AMD patients were not reached, with a final evaluable sample of 181 patients diagnosed with AMD (dry or neovascular). Although this sample size implies a lower precision, it allows the estimation of categorical variables with a 95% CI of ± 7.3 percentage points and 0.15 SD for the estimation of continuous variables.
Only private financing costs were included, and no costs were allocated according to public bases. Furthermore, private costs were only imputed in those patients who provided the data and were available.
Continuous variables were described by the mean, SD, median, minimum, and maximum, and depending on the distribution of the analyzed variable, quartiles were also presented. The number and percentage of patients by response category were used to describe categorical variables. No imputation of missing values was made for any variable. Counts (i.e., number of visits, number of medical tests and VFQ-25 scores) were treated as continuous variables. Data were analyzed with Statistical Analysis System (SAS) Enterprise Guide 7.15, considering a significance level of 0.05 (p<0.05).
Ethical considerations
The study was conducted according to guidelines on observational post-authorization studies for medicinal products for human use specified in Order SAS/3470/2009 of The Spanish Agency of Medicines and Medical Devices (AEMPS) and following the ethical principles of the Declaration of Helsinki and the local regulation, including privacy laws at the time of the study initiation. The protocol, an informed consent form, informative leaflets and other information for patients were approved by the Ethical Committee of the University Hospital of Bellvitge (ref. EPA041/19). All patients gave an oral informed consent before being included in the study.
Results
Study population
A total of 181 patients were included in the study, all of whom (100%) were evaluable patients: 34.3% (n=62) patients reported dry AMD, 42.0% (n=76) nAMD and 23.7% (n=43) patients did not know the type of their AMD. Excluding patients who did not know their type of AMD, the distribution was 44.9% dry AMD and 55.1% nAMD.
All patients (100.0%) answered at least one question from each block of the interview. The mean time to complete the 5 blocks of the interview was 33 minutes, with a minimum of 15 minutes and a maximum of one hour.
AMD patients’ profile
The mean (SD) age of patients was 72.5 (8.9) years, 50% of them being between 68 and 79 years old; mainly females (59.1%) and living in company (81.2%), mostly with their partner and/or descendants.
Bilateral involvement was indicated in 59.7% (n=37) and 46.1% (n=35) patients with dry AMD and nAMD, respectively. At the time of the interview, AMD evolution was approximately 5.5-6 years (minimum of 2 months and maximum of 20 years) 11.6% (n=21) of patients having poor or very poor vision at diagnosis (no cases of complete blindness at diagnosis were reported).
Due to the advanced age of the AMD patients interviewed, only 8.3% (n=15) patients were currently employed (Table 1). The overall mean (SD) percentage of disability was 67.4% (20.0). Concomitant diseases were reported by 79.0% (n=143) patients, being osteoarthritis (37.8%), diabetes (30.1%) and hypertension (26.6%) the most common. 13.3% (n=24) of the AMD patients belonged to some support group or patient association related to AMD (Table 1).
| Dry AMD (N=62) | nAMD (N=76) | Unknown AMD (N=43) | Total AMD (N=181) | ||
|---|---|---|---|---|---|
| Sociodemographic data | |||||
| Age (years), mean (SD) | 72.2 (8.6) | 72.9 (8.8) | 72.3 (9.7) | 72.5 (8.9) | |
| Sex (female), n (%) | 39 (62.9%) | 44 (57.9%) | 24 (55.8%) | 107 (59.1%) | |
| Living in company, n (%) | 48 (77.4%) | 60 (78.9%) | 39 (90.7%) | 147 (81.2%) | |
| Partner | 41 (85.4%) | 56 (93.3%) | 35 (89.7%) | 132 (89.8%) | |
| Children | 15 (31.3%) | 15 (25.0%) | 10 (25.6%) | 40 (27.2%) | |
| Caregiver | - | 2 (3.3%) | 2 (5.1%) | 4 (2.7%) | |
| Others (brothers) | 2 (4.2%) | 1 (1.7%) | 1 (2.6%) | 4 (2.7%) | |
| Employment situation, n (%) | |||||
| Active | 4 (6.5%) | 7 (9.2%) | 4 (9.3%) | 15 (8.3%) | |
| Non-active | 57 (91.9%) | 69 (90.8%) | 39 (90.7%) | 165 (91.2%) | |
| Reason for non-work activity | Unemployed | 1 (1.8%) | 3 (4.3%) | 3 (7.7%) | 7 (4.2%) |
| Due to AMD | - | - | 1 (33.3%) | 1 (14.3%) | |
| Retired | 45 (78.9%) | 56 (81.2%) | 31 (79.5%) | 132 (80.0%) | |
| Due to AMD | 1 (2.2%) | 6 (10.7%) | 3 (9.7%) | 10 (7.6%) | |
| Not known | 11 (19.3%) | 10 (14.5%) | 5 (12.8%) | 26 (15,8%) | |
| Incapacity for work | Incapacity for work | 3 (5.3%) | 7 (10.1%) | 3 (7.7%) | 13 (7,9%) |
| Due to AMD | - | 5 (71.4%) | 3 (100%) | 8 (61,5%) | |
| Not known | 1 (1.8%) | - | - | 1 (0,6%) | |
| Not known | 1 (1.6%) | - | - | 1 (0.6%) | |
| Belongs to a support group related to AMD, n (%) | 11 (17.7%) | 10 (13.2%) | 3 (7.0%) | 24 (13.3%) | |
Note: AMD: Age-related macular degeneration; nAMD: neovascular age-related macular degeneration; SD: Standard deviation.
Table 1. Sociodemographic characteristics of the study population.
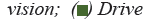
Overall, 46.4% (n=84) patients reported moderate vision, 37.0% (n=67) reported poor vision (n=22 of them with very poor vision), and only the remaining 16.6% (n=29) patients reported having excellent/good vision. Patients with dry AMD considered their vision as fair (53.2%) or poor/very poor (33.9%). In nAMD patients, the percentage of patients with poor/very poor vision was greater (42.1%), while a lower percentage of patients reported moderate vision (36.8%).
Impact on HRQL and daily activities from the patients’ perspective
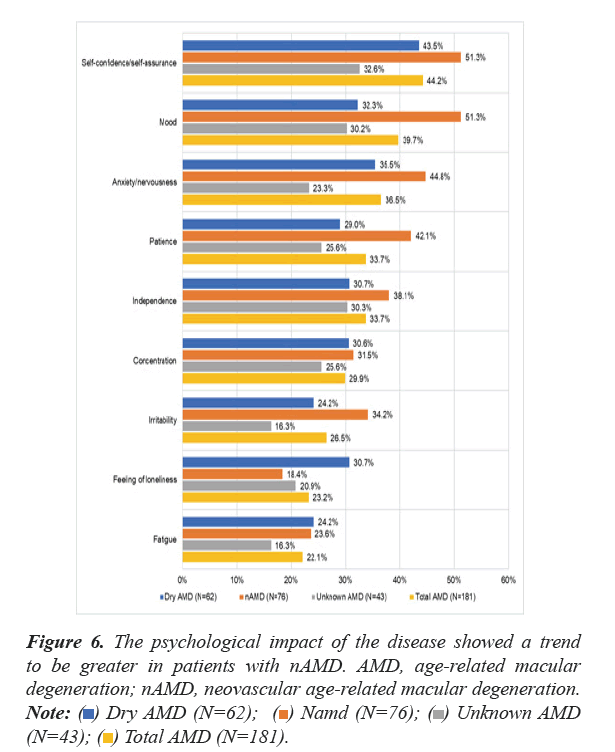
Overall, the mean (SD) VFQ-25 score was 66.8 (18.8) over 100 points, apparently indicating a low impact of AMD in their daily life. However, other dimensions of the questionnaire showed lower mean scores, for example, activities that require near vision (57.1 points), overall vision (53.5 points) and driving (44.2 points) (Figure 1).
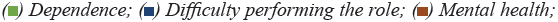
When questions related to patient’s actual quality of vision where analyzed, more nAMD patients reported worse vision quality (14.5% {n=11}). Moreover, nAMD patients reported having a greater concern for their eyesight (14.9% all the time/ most of the time) than dry AMD patients (8.2% all the time/ most of the time) (Figures 2a and 2b).
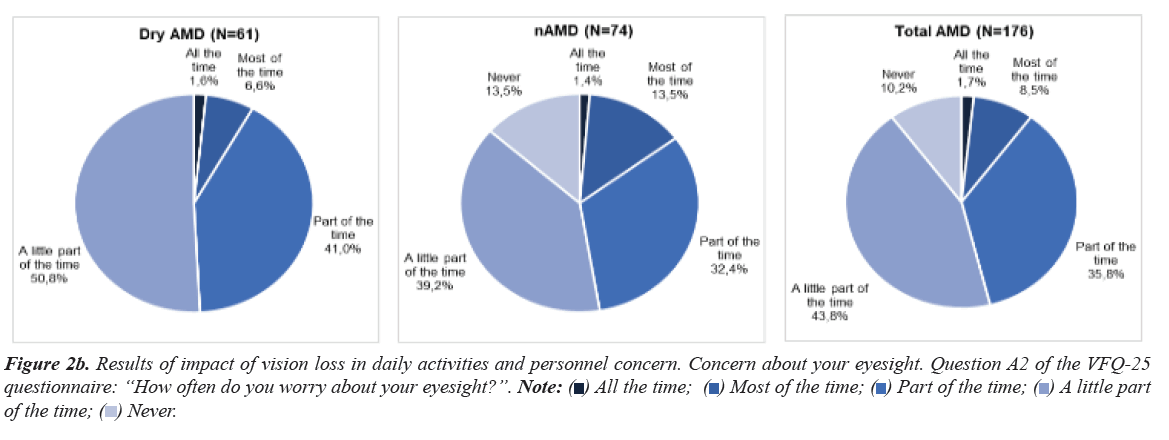
When patients were asked about carrying out daily living activities, overall, 24.9% (n=45) patients had difficulty reading the regular print of newspapers, more specifically, 8.1% (n=5) dry AMD patients and 17.1% (n=13) nAMD patients stopped doing it due to their vision. More patients with nAMD (30.3% ={n=23}) than patients with dry AMD (22.6% {n=14}) had extreme difficulty in doing jobs, practicing hobbies that required near vision or even stopped doing it due to vision problems (Figure 3).
The worst valued dimension in the VFQ-25 questionnaire was driving, with 34.3% (n=62) AMD patients currently driving, of whom 3.9% (n=7) had moderate/extreme difficulty. Moreover, of the 65.7% (n=119) patients who answered not to drive, 63.2% (n=36) said they had stopped doing it, mainly due to visual impairment. Difficulty driving at night was moderate/extreme in 15.5% (n=28) drivers, and 2.8% (n=5) stopped driving at night due to vision problems.
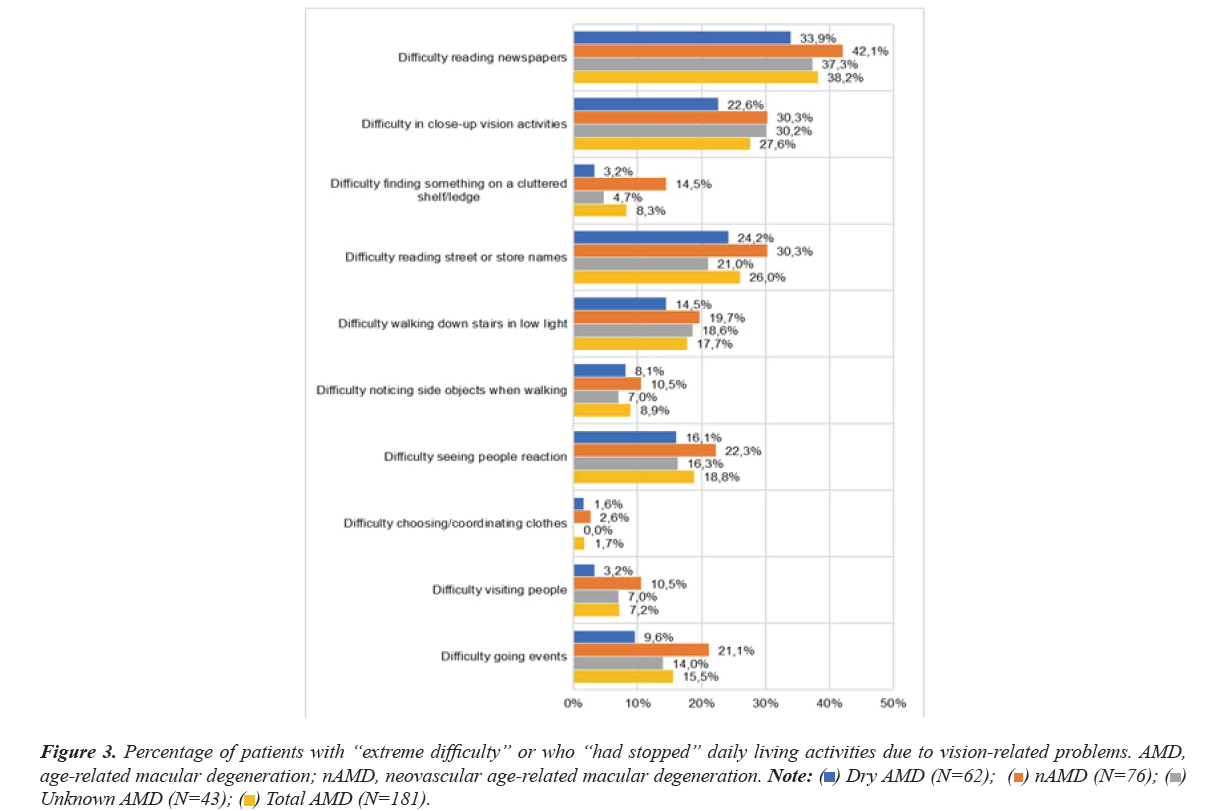
Overall, 33.7% (n=61) patients reported less control over their daily routine due to their vision, 17.7% (n=11) patients with dry AMD stayed at home most of the time, and 25.8% (n=16) felt frustrated, while in the nAMD group, these percentages were lower, being 7.9% and 14.4%, respectively (Figure 4).
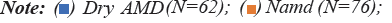
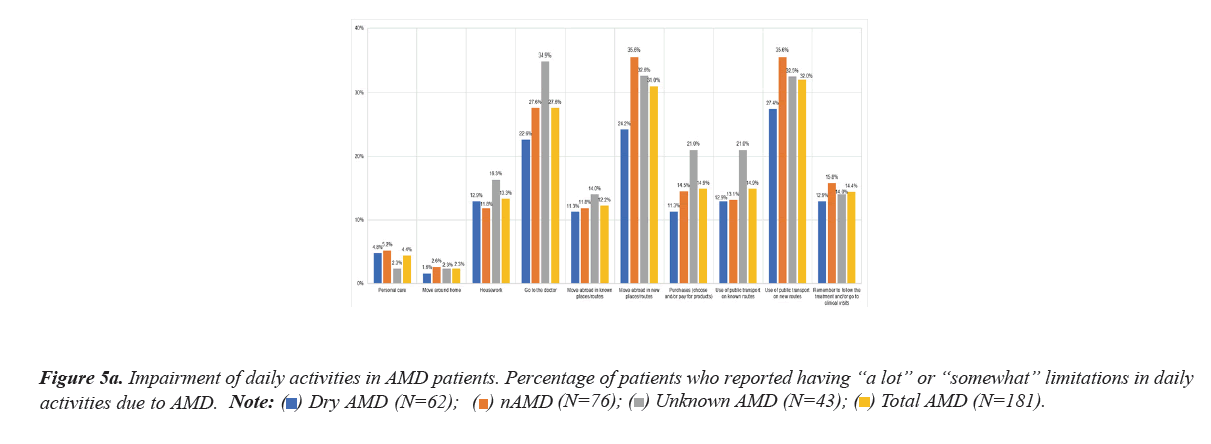
Daily living activities in new environments forthe patients showed the greatest limitation, such as the use of public transport in new routes (32.0%), mobility in unknown places or routes (31.0%) and attending a medical appointment (27.6%). Consequently, these activities required support from another person (Figures 5a and 5b).
The aspects of daily life most affected by AMD were the patient's working life or main occupation (22.6%), followed by home care (16.1%) and exercise (12.1%).
Patient journey
The mean (SD) time elapsed from the first complaints until AMD diagnosis by a doctor was 6.4 (14.5) months, with a minimum of 1 week and a maximum of 10 years; the median time was 1 month. The mean (SD) time elapsed from diagnosis to the start of treatment was 2.9 (6.8) months; the median time was 0.5 months.
Initially, 48.6% (n=88) patients went to the public health ophthalmologist, while 25.4% (n=46) went to a private ophthalmologist. After this first appointment, the doctor who diagnosed their AMD was the public health ophthalmologist, and once diagnosed, most patients were treated in the public hospital (79.0%).
Of all patients with AMD (n=181), 142 had received treatment and 43.1% of all patients (n=78) had received intravitreal injections in the last 12 months. Particularly, in the case of nAMD patients, 74.6% (n=53) were treated with intravitreal injections in the last 12 months, with a mean (SD) of 5.6 (3.5) injections reported by patients. Only 13.2% (n=7) patients were treated in private centers.
The mean (SD) number of visits due to AMD (treatment and/or examination) in the last 12 months was 2.7 (2.0) in dry AMD patients and 6.2 (3.9) in nAMD patients.
Use of resources
In the last 12 months, 81.2% (n=147) patients attended an appointment with the public ophthalmologist, and 22.7% (n=41) attended an appointment with a private ophthalmologist, with a median cost of €120.00 per private visit. Almost no appointments were made to other professionals, except for 8.8% (n=16) patients who went to the public primary care doctor. The mean (SD) number of total visits per patient reported in the last 12 months was 4.9 (6.1) (0.9 to private and 4.0 to public centers).
A total of 6.4% (n=84) patients used their private car, 35.4% (n=64) used public transport and 11.0% (n=20) used taxis to attend their AMD follow-up visits, with a mean (SD) of 5.2 (5.1) trips in the last 12 months.
Normal prescription glasses were required by 90.1% (n=163) patients, and sunglasses or dark glasses were required by 80.7% (n=146). In addition, 37.0% (n=67) patients stated that they used other reading aids, such as a magnifying glass, a special lamp, or a computer application, among others.
Domestic employees to carry out housekeeping or daily tasks and to accompany patients were required by 13.9% (n=25) patients, mostly paid by patients or their families (96.0% of them). A close person (family member, neighbor, or volunteer) who did not receive economic remuneration in return helped 47.0% (n=85) patients, with a median of 12 hours/week. Of these caregivers, 28.2% (n=24) were not working at the time of the interview, and of those who were working, 56.0% (n=14) had to take time off from work in the last 6 months due to diverse care responsibilities.
Psychological impact, HRQoL and personality
The emotional impact on patients upon being diagnosed with AMD was high or very high in 85.5% (n=53) dry AMD patients and 73.7% (n=56) nAMD patients. Overall, 69.6% (n=126) patients reported fear due to the risk of going blind. Regarding the disease evolution, only 2.8% (n=5) patients thought they would end up losing their sight, and 7.2% (n=13) thought it would become quite worse; however, the outlook for the evolution of symptoms was mostly a slight worsening (23.8%) or stability (28.7%).
On a range from 0 (the least possible psychological impact) to 10 (the greatest possible psychological impact), the mean (SD) score of the psychological impact of AMD reported by the patients was 5.2 (1.7), indicating medium impairment. Patients with good or moderate vision at diagnosis showed a mean (SD) score of 5.1 (1.8), while in patients with poor vision, the mean (SD) score increased by one point to 6.1 (1.4). There was a trend indicating that the worse the vision was at the time of diagnosis, the greater the psychological impact. Moreover, patients with poor or very poor vision at the time of the interview showed a trend of greater impairment in all dimensions of the VFQ-25 questionnaire versus patients with better vision.
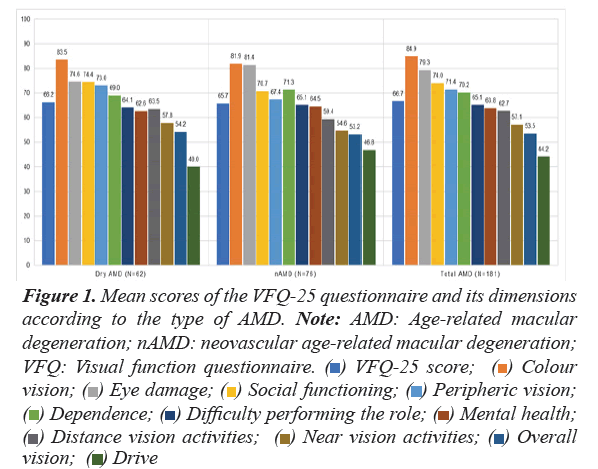
A greater affectation was observed in self-confidence and security of the patients in them (44.2%) and in the mood (39.7%), followed by anxiety/nervousness (36.5%). The psychological impact of the disease showed a trend to be greater in patients with nAMD (Figure 6).
Patient satisfaction with treatment and assistance and expectations with prognosis
Among the 144 patients who received or were receiving treatment for AMD, it entailed an effort or even a discomfort to follow treatment for 22.6% (n=41) of them, regardless of the type of treatment, which was higher for nAMD (4.8% in dry AMD versus 40.8% in nAMD). The satisfaction of these patients with treatment outcomes when they started was more or less as expected in 35.4% (n=64) of the overall patients (30.6% and 39.5% of the patients with dry AMD and nAMD, respectively), 20.4% (n=37) AMD patients considered it to be much better than expected (9.7% in dry AMD versus 26.3% in nAMD), 37.0% (n=67) were satisfied or very satisfied with the benefits provided by the AMD treatment (14.5% in dry AMD versus 51.3% in nAMD), and 8.8% (n=16) indicated that they were quite or very unsatisfied (6.5% and 10.9% of the patients with dry AMD and nAMD, respectively).
Of the surveyed patients, 89.5% (n=162) were satisfied with the assistance received by health professionals, mainly during the first months after diagnosis. Regarding unsatisfied patients, 75.0% (n=12) reported that the professionals had given few explanations about the disease and its consequences, indicated lack of empathy of these professionals and 18.8% (n=3) indicated lack of time during medical appointment as the main reason for unsatisfaction.
Of the patients who had received intravitreal treatment, 18.8% stated that they had abandoned it, 86.7% of the dropouts were motivated by the ophthalmologist and 66.7% were motivated due to lack of effectiveness.
Opinion of AMD patients on the information received about their disease
At diagnosis, 64.6% (n=117) patients received information from a social health professional about the symptoms and/or vision problems that could arise due to AMD, 63.0% (n=114) reported having received information on available treatments and its possible side effects, 53.0% (n=96) patients indicated that health professionals informed them about the disease evolution over time and 23.8% (n=43) received information about the limitations that they could have in their daily life. Only 7.2% (n=13) patients were informed about the benefits and social assistance available related to AMD and/or vision loss and its treatment.
Of the surveyed patients, 57.5% (n=104) considered that they had all the necessary information on AMD. Among the 38.7% (n=70) patients who did not consider it, 31.6% (n=55) of the surveyed patients would especially like to have information about AMD evolution and 28.2% (n=49) about the possible complications that may arise over time. It is important to highlight that 55.7% (n=39) patients would like to have more information about treatment benefits.
Discussion
The results of this study are part of a broader project [22], carried out in Spain involving several patient advocacy groups, main scientific societies, caregivers and professionals to identify the impact of AMD in the Spanish population and to design strategies for better patient care in the future. Together with the current survey used to evaluate vision related QoL in clinical trials (VFQ-25), an additional questionnaire was included to provide knowledge about the experience of Spanish patients with AMD treatment, their health care and HRQoL, and to determine the impact of AMD on their lives through the difficulties that they encountered in their daily life, their expectations, and fears. To meet the objectives of the study, a telephone survey was conducted across different regions in Spain with 181 AMD patients who voluntarily agreed to participate in an interview about their disease.
The socio-demographic characteristics of the surveyed population are consistent with those for the general elderly population obtained from the Spanish national health survey conducted in 2017 [23]. The percentage of patients who had increased difficulty in their daily activities or showed permanent disability due to AMD was also consistent with previous studies [5].
Considering that almost half of patients reported moderate vision (46.4%), the impact of the vision assessed by the specific VFQ-25 on HRQoL was reasonably accurate (mean score of 66.8 (sd18.8) points), because even if this impact on QoL is slightly higher than that observed in the literature, it is consistent with the highest impact reported by Spanish patients (56.5 versus other Western countries (48.0 Canada, 44.4 France, 51.3 Germany and 52.7 United Kingdom)) [24]. In our study, the dimensions of the questionnaire with the greatest impact on patients’ daily life were driving, overall vision and activities involving near vision. These are slightly different from those with worse scores in the Australian study [5] (overall health, driving and overall vision) and from those of the United States study [25] (color vision, eye pain, social functioning and peripheral vision). In this sense, our study reflected the extreme difficulty that AMD patients have on basic daily living activities related to near vision as reading the regular print of newspapers (24.9% of the total patients) or doing jobs or hobbies that require near vision (27.6%), and how the impact is greater when suffering nAMD. The higher impact on activities that depend on near vision has already been reported by Taylor et al [2], in a systematic review of the scientific literature, although not differentiating for type of AMD (dry and neovascular), as provided here. These data is especially relevant, taking into account that the limitation on these types of activities has a significant impact on the quality of leisure time and, therefore, on the social inclusion and interpersonal relationships of the elderly, which must be guaranteed in a holistic quality of life model [26].
Patients in our study reported need for external help to carry out different daily activities (13.9% required a domestic employee to carry out housekeeping or daily tasks) and presented even greater limitations when carrying out activities in new and unknown environments. The need for external help means that caregivers must spend a significant time accompanying the patient, contributing to an increase in the overall burden of the disease, as pointed out by previous studies [5,15,24].
Furthermore, 48.8% of the patients required the help to carry out these tasks without any financial retribution, a higher percentage than the 28.9% of a study carried out in other Western countries [24]. In general, unpaid persons are direct relatives who must take time off work. This impact has already been noted in previous studies [5,15,24].
For AMD patients, it took a mean of 6.4 (14.5) months to be diagnosed from first visual discomfort. Once diagnosed, patients were mostly treated in a public hospital (79.0%), meaning that the Spanish National Health System must be ready to treat a large number of patients, entailing consequently a high economic and clinical burden.
Regarding psychological impact, patients with good or moderate vision at diagnosis showed a lower mean score (5.1) than patients with poor vision (6.1). Indeed, more than two-thirds of the respondents (69.6%) reported fear due to the perceived risk of going blind. The psychological and HRQoL impact of nAMD could be reduced significantly if earlier diagnoses had been made, since existing treatments are more effective if the disease is detected in its early stages, allowing maintenance of visual acuity over time [27].
Moreover, an impact in self-confidence and security of the patients in themselves (44.2%) and in their mood (39.7%) was observed due to AMD, followed by anxiety/nervousness (36.5%), higher than results presented in previous studies [24,28].
The present study entails some limitations inherent to the studies conducted through direct interviews with patients, all of whom are subjected to a certain degree of subjectivity and memory bias, voluntary participation bias, among others. Also, as some of the patients came from patient advocacy groups, they perhaps showed a peculiarity in their character that implied being much more involved in the monitoring of their disease and, therefore, being much more critical at certain levels of the management of their disease. Regarding data collection, telephone interviews have shown very similar results to face-to-face interviews in comparative studies of both methods; therefore, telephone interviews are a valid survey method to access a large sample of a dispersed population [29], as was the case in the present work. Thus, it is not easy to compare the characteristics of the sample of the present study with other studies, published elsewhere. Unfortunately, the Spanish version of the IVI [30], questionnaire was not available at the time the study was conducted, thus was not available for Spanish population. Despite limitations, the design of the study, based on a direct interview with patients, was the most appropriate to collect the direct point of view of the patients about the implications of AMD in their life and HRQoL.
Conclusion
In conclusion, the study showed that from the perspective of AMD patients, loss of vision is important and has an impact on patient HRQoL in aspects directly associated with sight as well as with psychological aspects of their life. Early diagnosis and preservation of vision seems critical to limit the impact that AMD has on their lives. The dependence of patients to perform common tasks is remarkable, since it generates a significant impact on indirect costs associated with the need for a formal or informal caregiver and should be considered in economic evaluations of the different health interventions or therapies to stop or slow down AMD progression. Patients with nAMD suffer from greater visual impairment and have a greater impact on the degree of autonomy and the patient's HRQoL. In this group of patients, the care process needs to be optimized by shortening the time to diagnosis and start of treatment.
Ethics Approval and Consent to Participate
The study was conducted according to guidelines on observational post authorization studies for medicinal products for human use specified in Order SAS/3470/2009 of The Spanish Agency of Medicines and Medical Devices (AEMPS) and following the ethical principles of the Declaration of Helsinki and the local regulation, including privacy laws, at the time of the initiation of the study.
The protocol, informed consent form, informative leaflets and other information for patients were approved by the Ethical Committee of the University Hospital of Bellvitge (ref. EPA041/19).
Availability of Data and Materials
Upon confidentiality agreement, data might be shared. Our manuscript has associated data in a data repository.
Competing Interests
JM Ruiz-Moreno has been a consultant for Allergan, Bayer, Novartis, Roche and Topcon. L Arias Barquet has been a consultant for Allergan, Bayer, Novartis, Roche, and Topcon. J García-Arumí has been a consultant for Novartis, Bayer, and Alcon. L Gómez-Baldó and C Blanch work for Novartis Farmacéutica SA. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by Novartis Farmacéutica SA. The sponsor or funding organization participated in the design of the study; management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript.
Authors' Contributions
J Ruiz-Moreno, L Arias Barquet and J García-Arumí are the study coordinators and contributed to the design and development of the study. L Gómez-Baldó and C Blanch contributed to the design and development of the study. J Ruiz-Moreno, L Arias Barquet and J García-Arumí contributed to the manuscript writing and the acquisition of data and information. J Ruiz-Moreno, L Gómez-Baldó and C Blanch contributed substantially to data interpretation and the review of the manuscript. All authors reviewed the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgements
We thank all the centers and investigators that have collaborated in the Objetivo DMAE study: Dr. Enrique Rodríguez de la Rua (Hospital Universitario Virgen de la Macarena), Dr. Isabel Pinilla Lozano (Hospital Clínico Universitario Lozano Blesa), Dr. Maribel López Gálvez (Hospital Clínico Universitario de Valladolid), Dr. Pere Romero Aroca (Hospital Universitario de Reus), Dr. Jose Antonio López Garrido (Hospital de Galdakao), Dr. Patricia Udaondo Mirete (Hospital Universitario La Fe), Dr. Jacobo González Guijarro (Hospital Universitario de La Princesa) and Dr. Marta Rodríguez Núñez (Hospital do Meixoeiro de Vigo).
We thank Andrés Mayor (President of Acción Visión España), Jacinto Zulueta (President of Mácula Retina) Paca Tricio (President of UDP) and Juan Manuel Martínez (President of CEOMA) for their contribution to the conception of the study. We also thank the patients for their participation in the study.
We thank IQVIA and Carmen Barrull and David Gasche for providing medical editorial assistance with this manuscript. We also thank Teresa Guix, Gabriela Susanna Mònica Pintaluba and Clara Amat (Novartis Farmacéutica SA) for their collaboration and assistance in writing and project management and Angels Costa and Carmen Navarro (Novartis Farmacéutica SA) for their contribution to the design and accomplishment of the study.
References
- Spanish Eyes Epidemiological (SEE) Study Group. Prevalence of age-related macular degeneration in Spain. Br J Ophthalmol. 2011;95(7):931-936.
- Taylor DJ, Hobby AE, Binns AM, et al. How does age-related macular degeneration affect real-world visual ability and quality of life? A systematic review. BMJ open. 2016;6(12):e011504.
- Colijn JM, Buitendijk GH, Prokofyeva E, et al. Prevalence of age-related macular degeneration in Europe: the past and the future. Ophthalmology. 2017;124(12):1753-1763.
- Ord LM, Wright J, DeAngelis MM, et al. Quality of life with macular degeneration is not as dark as it may seem: Patients’ perceptions of the MacDQoL questionnaire. J Clin Med. 2015;4(9):1841-18852.
- Spooner KL, Mhlanga CT, Hong TH, et al. The burden of neovascular age-related macular degeneration: a patient’s perspective. Clinical Ophthal. 2018;12:2483.
- Mitchell J, Bradley C. Quality of life in age-related macular degeneration: a review of the literature. Health Qual Life Outcomes. 2006;4:97.
- Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 1992;99(6):933-943.
- Mitchell P, Smith W, Attebo K, et al. Prevalence of age-related maculopathy in Australia: the Blue Mountains Eye Study. Ophthalmology. 1995;102(10):1450-1460.
- Vingerling JR, Dielemans I, Hofman A, et al. The prevalence of age-related maculopathy in the Rotterdam Study. Ophthalmology. 1995;102(2):205-210.
- Varma R, Fraser-Bell S, Tan S, et al. Prevalence of age-related macular degeneration in Latinos: the Los Angeles Latino eye study. Ophthalmology. 2004;111(7):1288-1297.
- Augood CA, Vingerling JR, de Jong PT, et al. Prevalence of age-related maculopathy in older Europeans: the European Eye Study (EUREYE). Arch Ophthalmol. 2006;124(4):529-535.
- Damián J, Pastor-Barriuso R, Armadá F, et al. Epidemiología de la degeneración macular asociada con la edad. Situación en España. 2006;38(1):51-57.
- Gohil R, Crosby-Nwaobi R, Forbes A, et al. Caregiver burden in patients receiving ranibizumab therapy for neovascular age related macular degeneration. PloS one. 2015;10(6):e0129361.
- Trillo AH, Dickinson CM. The impact of visual and nonvisual factors on quality of life and adaptation in adults with visual impairment. Invest Ophthalmol Vis Sci. 2012;53(7):4234-4241.
- Gopinath B, Liew G, Burlutsky G, et al. Age-related macular degeneration and 5-year incidence of impaired activities of daily living. Maturitas. 2014;77(3):263-266.
- Gao G, Ouyang C, Dai J, et al. Baseline traits of patients presenting at a low vision clinic in Shanghai, China. BMC ophthalmology. 2015;15(1):1-6.
- Dawson SsR, Mallen CD, Gouldstone MB, et al. The prevalence of anxiety and depression in people with age-related macular degeneration: a systematic review of observational study data. BMC ophthalmology. 2014;14(1):1-7.
- McCloud C, Lake S. Understanding the patient’s lived experience of neovascular age-related macular degeneration: a qualitative study. Eye. 2015;29(12):1561-1569.
- Müller S, Ehlken C, Bauer-Steinhusen U, et al. Treatment of age-related neovascular macular degeneration: the patient’s perspective. Graefe's Arch Clin Exp Ophthalmol. 2017;255(11):2237-2246.
- Coleman AL. Development of the 25-item national eye institute visual function questionnaire. Arch Ophthalmol. 2002;3(1):58-59.
- Alvarez-Peregrina C, Sánchez-Tena MA, Caballé-Fontanet D, et al. Crosscultural adaptation and validation into Spanish of the questionnaire National Eye Institute Visual Function Questionnaire 25. Arch Soc Esp Oftalmol. 2018;93(12):586-91.
[Google Scholar] [CrossRef] [PubMed]
- Arias Barquet L, Esteban Vega AI, García Arumí J, et al. Objetivo DMAE. Situación actual y propuestas de mejora para la atención sociosanitaria de la DMAE. 2021.
- Ministerio de Sanidad. Encuesta nacional de salud de españa 2017.2020.
- Soubrane G, Cruess A, Lotery A, et al. Burden and health care resource utilization







 Total AMD (N=181).
Total AMD (N=181).