Research Article - Addiction & Criminology (2021) Volume 4, Issue 4
Depression and Anxiety Among Syrians - A National Survey
F Mohsen1*, B Bakkar1, S Melhem1, S Aldakkak1, D Mchantaf1, M Marrawi3, Y Latifeh2
1Faculty of Medicine, Syrian Private University, Damascus, Syria
2Departement of Psychiatry, Faculty of Medicine, Syrian Private University, Damascus, Syria
3Department of Statistics, Syrian Private University, Syria
- Corresponding Author:
- Fatema Mohsen
Faculty of Medicine
Syrian Private University
Syria
E-mail: fatemamohsena@gmail.com
Accepted date: September 01, 2021
Citation: Mohsen F, Bakkar B, Melhem S, et al. Depression and anxiety among Syrians:A national survey assessment. Addict Criminol. 2021;4(4):1-8.
Abstract
Introduction: War and COVID-19 has inevitably triggered mental health disorders among Syrians. This virus has overwhelmed public healthcare systems worldwide and forced governments to impose draconian lockdowns of entire countries. This study aims to assess the prevalence of depression and anxiety during the COVID-19 outbreak embedded within the war.
Methods: This web-based cross-sectional screening study was distributed randomly in May 2020, during the Syrian war and COVID-19 pandemic. The survey contained several questions related to socio-demographic characteristics, and the Patient Health Questionnaire 9-item and Generalized Anxiety Disorder 7-item scale were used. Multivariable logistic regression analysis was performed to identify factors associated with depression, and anxiety. Statistical Package for Social Sciences version 25.0 (SPSS Inc., United States) was used to analyze data.
Results: Of the 3989 participants, 73.5% were female, 77.6% were single, 13.9% have chronic disease(s), and 10.4% have a poor economic status. The study revealed a high level of depressive 3326 (83.4%) and anxiety symptoms 2777 (69.6%) among participants. Multivariable logistic regression analysis revealed that females were a risk factor for depressive and anxiety symptoms.
Conclusion: This study showed an alarmingly high prevalence of depressive and anxiety symptoms among Syrians who have limited access to mental healthcare services. A change in the health care system must be addressed to provide urgent resources to alleviate acute mental health disturbances and improve their physical health perceptions.
Keywords
Mental health, Psychology, Depression, Anxiety, Syria population, War crisis.
Introduction
The significant association between war exposure or pandemic spread and elevated mental health disorders prevalence have been shown repeatedly in previous studies [1,2]. The Syrian conflict, now reaching a decade, paralleled with the domestically spreading Coronavirus Disease 2019 (COVID-19), is threatening civilians across Syria. The mental health of Syrians has been immensely challenged during the viral pandemic that emerged in this ongoing crisis.
Healthcare systems have been pushed to breaking point to deal with this pandemic. The ever-increasing number of deaths confirmed cases, and affected provinces and countries have led to public trepidation. This sudden outbreak and virus virulence will inevitably trigger anxiety, depression, and other mental disorders among the population. The latest numbers have shown significantly higher confirmed cases and deaths in neighbouring countries such as Turkey (160,979 and 4,461), Jordan (728 and 9), Lebanon (1,168 and 26) in contrast with Syria (122 and 4) [3]. Most borders within Syria remain closed, however, Turkey, Jordan and Lebanon have had some exemptions where the movement of people into the country have initiated the COVID-19 outbreak [4,5]. Lack of effective treatment, fears of death and contagion, losing family members or friends, social isolation, media misinformation overload, depletion of personal protection equipment, supplies, panic buying, and inadequate psychosocial support may all adversely affect individuals mental health. Levels of anxiety symptoms ranged from 6.3% to 50.9%, and depressive symptoms from 17.2% to 53.5% during the COVID-19 pandemic [6]. Depression constitutes major suicide deaths numbers (800,00 per year), ranked by WHO (World Health Organization) as the largest contributor to disability, and the third leading cause of disease burden globally; anxiety disorders are ranked the 6th contributor to disability [7]. Many people with depression are unaware they are suffering from a treatable illness, which can be screened, treated, and managed, and seeking help may not cross their minds. Therefore, their persisting involuntary symptoms can become unbearable, who may resolve suicide to end their pain.
The prolonged conflict has exposed civilians to grave human violations including, killing, maiming, sexual assault, torture, explosive remnants, and displacement. Families are being forced to endure abominable conditions where 89% of the population are living in extreme poverty circumstances [8]. Infrastructures including hospitals and schools and public services are being systematically decimated. The Syrian ministry of health provides 3 hospitals for mental illness and substance abuse: Ibn Sina Hospital in Rural Damascus, Ibn Rushd Hospital in Damascus, and Ibn Khaldoun Hospital in Aleppo. Ibn Khaldoun Hospital was bombarded on 25 December 2012, leaving only 2 hospitals standing [9]. 1 million Syrians are estimated to suffer from severe psychiatric disorders, with only 80 psychiatrists working in Syrian territories (1 per 100 000 population) in 2018 [10,11]. Assuming that psychiatrists work 5 days/week for 52 weeks/year, and that each doctor can follow up on 15 cases/day and that they do not follow up on each patient more than 3 times a year, the total number of cases that the 80 psychiatrists can follow up on annually is 104,000, leaving 90% of severe cases unattended, untreated, and unmanaged. Destruction of mental health services, an increase in the prevalence of mental health problems as a result of conflict, and an inadequate number of psychiatrists are set to overwhelm health services [9].
Currently, there are no published studies on the impact of conflict on the mental health within Syria, nor are there any studies on the simultaneous impact of war and pandemic, however a systematic review on the mental health of Syrian refugees showed alarming numbers where levels of depression ranged from 11% to 49%, anxiety disorders from 49% to 55%, and post-traumatic stress disorder from 16% to 84% [10]. Since Syrians have been persistently exposed to panic and distress we aim to provide an estimated prevalence of depressive and anxiety symptoms during this tumultuous time. The objectives of this screening study are to identify potential factors associated with depressive, and anxiety symptoms.
Methods
Study design, setting, and participants
This web-based cross-sectional study was conducted using an Arabic questionnaire over 12 days between May 2 and May 14 of 2020. All participants aged 18 and above, residing in Syria with no known history of COVID-19 infection were included in the study. The questionnaire was distributed randomly through various social media platforms. All the participants provided online consent to participate in the study by answering a yes/no question, informed of the option to opt-out of the survey at any time, and the anonymity and confidentiality of their responses were assured. After confirmation, participants were directed to the first part of the survey to complete questions about sociodemographic information including gender, age, residence, education level, occupation, and economic status, participants were also asked about the history of chronic diseases. The Patient Health Questionnaire 9-item (PHQ-9), and the Generalized Anxiety Disorder 7-item (GAD-7) scale were used to evaluate the symptoms of depression and anxiety respectively. For this study, we used the Arabic version of PHQ-9 and GAD-7, which were validated in previous studies [11,12]. Score criteria of both PHQ-9 and GAD-7 were recorded as a 4-point scale, “0” (not at all), “1” (several days), “2” (more than half the days), and “3” (nearly every day), providing a 0-27, and 0-21 severity score range respectively. The PHQ-9 is a self-rated scale used to assess depression severity, with the scores categorized as none (0-4), mild (5-9), moderate (10-14), moderately severe (15- 19), and severe (20-27) [13]. The Gad-7 is a self-rated scale used to evaluate the severity of the 4 most common anxiety disorders (Generalized Anxiety Disorder, Panic Disorder, Social Phobia and Post Traumatic Stress Disorder). The scores were categorized as: none (0-4), mild (5-9), moderate (10-14), and severe (15-21) [14]. The study was ethically approved by the Institutional Review Board (IRB) of the Faculty of Medicine, Syrian Private University. The survey is available in appendix 1.
Statistical Analysis
Data analysis was executed using Statistical Package for Social Sciences version 25.0 (SPSS Inc., Chicago, IL, United States). Descriptive analysis, including frequencies, percentages, means and Standard Deviations (SD) were applied. Chi-square test was applied to describe the relationship between socio-demographic variables and the severity of anxiety, and depression. Binary logistic regression analysis was conducted to determine the significant predictors of depressive and anxiety symptoms using the socio-demographic variables as the independent variables. P-values <0.05 was considered statistically significant.
Results
Socio-demographic characteristics
Out of the 5000 total participants invited to take part in the study, 4,430 gave informed consent. 441 participants residing outside Syria were excluded, giving a final sample size of 3989 participants (response rate=79.8%). Most participants were female 2935 (73.5%), single 3096 (77.6%), students 2397 (60.1%), and residing in Damascus 1412 (35.4%). Participant ages ranged from 18 to 70 years, with the age group 18-25 years representing a majority of 2870 (71.9%). 416 (10.4%) participants stated they had poor economic status, and 1522 (38.1%) with moderate economic status. 556 (15.9%) mentioned a history of chronic diseases (Table 1).
| Gender (%) | Male | 1054 (26.4%) | Education (%) | Primary school | 21 (0.5%) |
| Female | 2935 (73.5%) | Intermediate school | 115 (2.9%) | ||
| Age (%) | 18-25 years | 2870 (71.9%) | Secondary school | 370 (9.3%) | |
| 26-34 years | 685 (17.2%) | College/University | 3271 (82%) | ||
| 35-44 years | 261 (6.5%) | Master’s degree | 185 (4.6%) | ||
| 45-54 years | 121 (3%) | PhD | 27 (0.7%) | ||
| 55 < | 52 (1.4%) | Occupation (%) | Health care worker | 259 (6.5%) | |
| Social status (%) | Single | 3096 (77.6%) | Government institution | 239 (6%) | |
| Married | 714 (17.9%) | Private institution | 202 (5.1%) | ||
| Other | 179 (4.5%) | Business | 202 (5.1%) | ||
| Economic status (%) | Excellent | 251 (6.3%) | Military | 35 (0.9%) | |
| Good | 1800 (45.1%) | Student | 2397 (60.1%) | ||
| Moderate | 1522 (38.1%) | Other | 655 (16.4%) | ||
| Poor | 416 (10.4%) | Household members (%) | Alone | 54 (1.4%) | |
| Chronic disease(s) (%) | Yes | 556 (13.9%) | 1-5 | 2474 (62%) | |
| No | 3433 (86%) | >5 | 1461 (36.6%) |
Table 1. Socio-demographic characteristics: (n=3989).
Depression and anxiety status
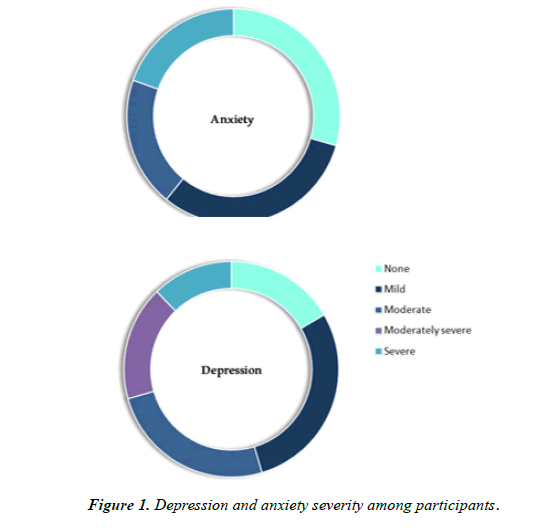
According to the PHQ-9 and GAD-7 scoring criteria, the prevalence of depressive and anxiety symptoms among participants was 3326 (83.4%) and 2777 (69.6%) respectively. Depression severity: none 663 (16.6%), mild 1150 (28.8%), moderate 1006 (25.2%), moderately severe 684 (17.2%), and severe 486 (12.2%). Anxiety severity: none 1212 (30.4%), mild 1293 (32.4%), moderate 805 (20.2%), and severe 679 (17.0%) (Figure 1).
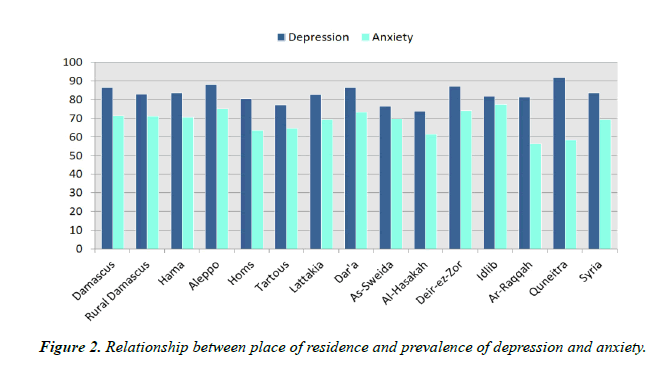
Comparison study
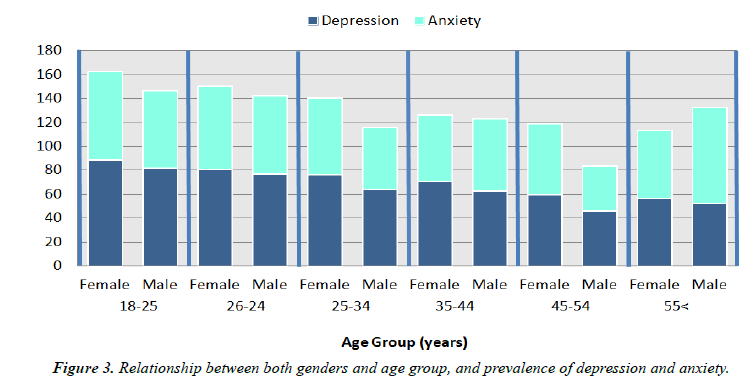
Depression scores were significantly higher among the social status of the single, education level of college/university, occupation of students, household members of 1-5, history of chronic disease(s) 2818 (70.6%), and good economic status (p<.0001) (Table 2). Anxiety scores were significantly higher among, education level of university/college (p<.0001), occupation of the student (p<.0001), household members of 1-5 (p=0.014), history of chronic disease(s) 2317 (58.1%) (p<.0001), and a good economic status (p<.0001) (Table 3). Depression was more prevalent among the residents of Ar- Raqqah (81.3%), while the lowest was among the residents of Al-Hasakah (73.7%). Anxiety was more prevalent among the residents of Idlib (77.3%), while the lowest was among the residents of Ar-Raqqah (56.3%) (Figure 2). Depression and Anxiety were significantly higher among females: 2506 (62.8%) and 2109 (52.9%); compared with males 820 (20.6%) and 668 (16.7%). Depression and anxiety were significantly higher in the age group 18-25 years compared with older ages (p<.0001) (Figure 3).
| Characteristics |
Non-depression group (n=663) | Depression group (n=3326) | χ2 | P | |
|---|---|---|---|---|---|
| Gender |
Male | (22.2%) 234 | (77.8%) 820 | 32.190 |
<.0001 |
| Female | (14.6%) 429 | (85.4%) 2506 | |||
| Age group (years) |
18-25 | (13.5%) 387 | (86.5%) 2483 | 104.787 |
<.0001 |
| 26-34 | 141 (20.6%) | (79.4%) 544 | |||
| 35-44 | (27.6%) 72 | (72.4%) 189 | |||
| 45-54 | (32.2%) 39 | (67.8%) 82 | |||
| 55< | (46.2%) 24 | (53.8%) 28 | |||
| Social status |
Single | (15.0%) 464 | (85.0%) 2632 | 28.381 |
<.0001 |
| In a relationship | (23.1%) 165 | (76.9%) 549 | |||
| Other | (19.0%) 34 | (81.0%) 145 | |||
| Residence |
Rural | (17.9%) 236 | (82.1%) 1079 | 2.489 |
0.115 |
| Urban | (10.7%) 427 | (56.3%) 2247 | |||
| Education |
Primary school | (14.3%) 3 | (85.7%) 18 | 35.608 |
<.0001 |
| Intermediate school | (18.3%) 21 | (81.7%) 94 | |||
| High school | (13.0%) 48 | (87.0%) 322 | |||
| College/university | (16.1%) 526 | (83.9%) 2745 | |||
| Master’s degree | (29.7%) 55 | (70.3%) 130 | |||
| PhD | (37.0%) 10 | (63.0%) 17 | |||
| Occupation |
HCWs | (30.1%) 78 | (69.9%) 181 | 91.562 |
<.0001 |
| Government institution | (30.1%) 72 | (69.9%) 167 | |||
| Private institution | (20.3%) 41 | (79.7%) 161 | |||
| Business | (19.3%) 39 | (80.7%) 163 | |||
| Military | (20.0%) 7 | (80.0%) 28 | |||
| Student | (13.0%) 312 | (87.0%) 2085 | |||
| Other | (17.4%) 114 | (82.6%) 541 | |||
| Household members |
0 | (9.3%) 5 | (90.7%) 49 | 21.237 |
<.0001 |
| 1-5 | (18.7%) 463 | (81.3%) 2011 | |||
| >5 | (13.3%) 195 | (86.7%) 1266 | |||
| Chronic disease(s) |
Yes | (8.6%) 615 | (91.4%) 2818 | 29.743 |
<.0001 |
| No | (17.9%) 48 | (82.1%) 508 | |||
| Economic status |
Poor | (9.4%) 39 | (90.6%) 377 | 28.658 |
<.0001 |
| Moderate | (16.0%) 243 | (84.0%) 1279 | |||
| Good | (17.8%) 320 | (82.2%) 1480 | |||
| Excellent | (24.3%) 61 | (75.7%) 190 | |||
Table 2. Socio-demographic characteristics and association with depressive symptoms.
| Characteristics |
Non-anxiety group (n=1212) | Anxiety group (n=2777) | χ2 | P | |
|---|---|---|---|---|---|
| Gender |
Male | (36.6%) 386 | (63.4%) 668 | 26.360 |
<.0001 |
| Female | (28.1%) 826 | (71.9%) 2109 | |||
| Age group(years) |
18-25 | (28.4%) 814 | (71.6%) 2056 | 34.790 |
<.0001 |
| 26-34 | (31.7%) 217 | (68.3%) 468 | |||
| 35-44 | (39.5% )103 | (60.5%) 158 | |||
| 45-54 | (43.0%) 52 | (57.0%) 69 | |||
| 55< | (50.0%) 26 | (50.0%) 26 | |||
| Social status |
Single | (30.3%) 939 | (69.7%) 2157 | 1.989 |
0.370 |
| In a relationship | (31.7%) 226 | (68.3%) 488 | |||
| Other | (26.3%) 47 | (73.7%) 132 | |||
| Residence |
Rural | (30.3%) 398 | (69.7%) 917 | 0.013 |
0.910 |
| Urban | (30.4%) 814 | (69.6%) 1860 | |||
| Education |
Primary school | (28.6%) 6 | (71.4%) 15 | 32.019 |
<.0001 |
| Intermediate school | (22.6%) 26 | (77.4%) 89 | |||
| High school | (21.9%) 81 | (78.1%) 289 | |||
| College/university | (30.8%) 1008 | (69.2%) 2263 | |||
| Master’s degree | (42.7%) 79 | (57.3%) 106 | |||
| PhD | (44.4%) 12 | (55.6%) 15 | |||
| Occupation |
HCWs | (42.1%) 109 | (57.9%) 150 | 34.458 |
<.0001 |
| Government institution | (38.9%) 93 | (61.1%) 146 | |||
| Private institution | (35.1%) 71 | (64.9%) 131 | |||
| Business | (30.2%) 61 | (69.8%) 141 | |||
| Military | (25.7%) 9 | (74.3%)26 | |||
| Student | (29.0%) 696 | (71.0%) 1701 | |||
| Other | (26.4%) 173 | (73.6%) 482 | |||
| Household members |
0 | (33.3%)18 | (66.7%) 36 | 8.589 |
0.014 |
| 1-5 | (30.0%)791 | (68.0%) 1683 | |||
| >5 | (27.6%) 403 | (72.4%) 1058 | |||
| Chronic disease(s) | Yes | (17.3%) 1116 | (82.7%) 2317 | 52.554 |
<.0001 |
| No | (32.5%) 96 | (67.5%) 460 | |||
| Economic status |
Poor | (16.8%) 70 | (83.2%) 346 | 65.495 |
<.0001 |
| Moderate | (28.4%) 433 | (71.6%) 1089 | |||
| Good | (33.4%) 601 | (66.6%) 1199 | |||
| Excellent | (43.0%) 108 | (57.0%) 143 | |||
Table 3. Socio-demographic characteristics and association with anxiety symptoms.
Multiple logistic regression
Multiple logistic regression analysis showed the following factors: female gender vs. male, (OR:1.653, p<.0001); age group of 18-25 years vs. 26-34 years, (OR:0.713, p=0.05; 35- 44 years, OR:0.430, p<.0001; 45-34 years, OR:0.298, p<.0001; 55 years and above, OR:0.156, p<.0001); occupation in private (OR:1.825, p=0.010), business (OR:2.058, p=0.003), and other sectors (OR:1.809, p=0.001), as well as students (OR:2.315, p<.0001) (vs. HCWs); economic status of poor (OR:4.771, p<.0001), moderate (OR:2.075, p<.0001) and good (OR:1.531, p<.0001) (vs. excellent); and having a chronic disease(s) (vs. not, OR:2.990, p<.0001), were factors significantly associated with depressive symptoms (Table 4).
| Characteristics | p.value | OR | 95% C.I. for OR | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Gender | Female vs male | <.0001 | 1.653 | 1.355 | 2.017 |
| Age | 26-34 vs 18-25 | 0.015 | 0.713 | 0.544 | 0.936 |
| 35-44 vs 18-25 | <.0001 | 0.430 | 0.297 | 0.622 | |
| 45-54 vs 18-25 | <.0001 | 0.298 | 0.184 | 0.482 | |
| 55 and above vs 18-25 | <.0001 | 0.156 | 0.080 | 0.308 | |
| Occupation | Private vs HCWs | 0.010 | 1.825 | 1.152 | 2.891 |
| Business vs HCWs | 0.003 | 2.058 | 1.280 | 3.310 | |
| Student vs HCWs | <.0001 | 2.315 | 1.658 | 3.234 | |
| Other vs HCWs | 0.001 | 1.809 | 1.259 | 2.599 | |
| Economic status | Poor vs excellent | <.0001 | 4.771 | 2.956 | 7.698 |
| Moderate vs Excellent | <.0001 | 2.075 | 1.473 | 2.922 | |
| Good vs Excellent | 0.011 | 1.531 | 1.101 | 2.130 | |
| Chronic disease(s) | Yes vs no | <.0001 | 2.990 | 2.120 | 4.215 |
Table 4. Multiple logistic regression analysis of depressive symptoms.
Multiple logistic regression analysis showed: female gender vs. male, (OR:1.476, p<.0001); age group of 18-25 years vs. 26-34 years, (OR: 0.708, p=.0001; 35-44 years, OR: 0.328, p<.0001; 45-54 years, OR: 0.243, p<.0001; 55 years and above, OR:0.189, p<.0001); education of school vs. college/ university and above, OR:0.624, p<.0001); careers in private, business, and other sectors, as well as students vs. HCWs, (OR: 0.725, p<.0001); economic status of poor (OR:6.339, p<.0001), moderate (OR:3.140, p<.0001) and good (OR:1.451, p=0.008) (vs. excellent); and having a chronic disease(s) (vs. not, OR:2.492, p<.0001) were factors significantly associated with anxiety symptoms (Table 5).
| Characteristics | p.value | OR | 95% C.I.for OR | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Gender | Female vs male | <.0001 | 1.476 | 1.263 | 1.725 |
| Age | 26-34 vs 18-25 | 0.001 | 0.708 | 0.577 | 0.869 |
| 35-44 vs 18-25 | <.0001 | 0.328 | 0.234 | 0.459 | |
| 45-54 vs 18-25 | <.0001 | 0.243 | 0.154 | 0.384 | |
| 55 and above vs 18-25 | <.0001 | 0.189 | 0.100 | 0.357 | |
| Education | University/College, Master, PHD vs Primary, Intermediate, Secondary | <.0001 | 0.624 | 0.488 | 0.798 |
| Occupation | HCWs vs Government, Private, Business, Military, Student , Other | 0.021 | 0.725 | 0.552 | 0.953 |
| Economic status | Poor vs excellent | <.0001 | 6.339 | 4.390 | 9.153 |
| Moderate vs Excellent | <.0001 | 3.140 | 2.371 | 4.160 | |
| Good vs Excellent | 0.008 | 1.451 | 1.101 | 1.911 | |
| Chronic disease(s) | Yes vs no | <.0001 | 2.492 | 1.941 | 3.198 |
Table 5. Multiple logistic regression analysis of anxiety symptoms.
Discussion
This is the first national survey conducted to evaluate the prevalence of depression and anxiety during the war and the COVID-19 pandemic among Syrian residents. Unprecedented measures have been adopted during the pandemic to mitigate the spread of disease including, lockdowns, social distancing, and self-isolation. This survey was conducted at a time where the number of confirmed COVID-19 cases started to rise, leaving an ominous atmosphere towards the country’s future [15].
The prevalence of depressive and anxiety symptoms among Syrians was 3326 (83.4%) and 2777 (69.6%) respectively. These numbers are significantly higher compared with studies conducted during the COVID-19 pandemic [6]. The high prevalence of depression and anxiety in war-ridden regions among individuals has been reported in a previous study (49%, 55%) respectively [10]. The high prevalence of depressive and anxiety symptoms found in our study have surpassed 2015 WHO prevalence estimations, of 3.9% and 4.3% respectively [7]. Multiple stressors, war-pandemic psychological effects, have triggered mental health disorders among Syrians.
Literature has revealed a lack of mental healthcare services provided by psychologists and psychiatrists that limits psychological care access for the many distressed individuals, including scarcity of online and social media support in the form of publications, resources, posts, guidelines, videos, and online group chats [8,9]. These latter methods can alleviate mental health problems caused by risk factors such as exposure to COVID-19. This study showed that 663 (16.6%) and 1212 (30.4%) have no depressive or anxiety symptoms. This is lower than studies conducted in Turkey (76.4% and 54.9%) and China (83.5% and 71.2%) [16,17]. The United Nations provided policies to mitigate the mental health consequences of the pandemic: a societal approach to care for mental health, ensure widespread psychosocial support, and long term management of affected individuals [18]. Good mental health is crucial for the functioning of a society, as the severe impact of war and COVID-19 must be addressed urgently.
All participants presenting with mild 1150 (28.8%) and moderate 1006 (25.2%) depression, and mild 1293 (32.4%) and moderate 805 (20.2%) anxiety require clinical assessment for symptom duration and functional disability to determine the necessity of treatment. As over half the population requires a scheduled clinical assessment, with a total population of 17,500,657, this concludes that over 9 million people require mental health services [19]. The lack of psychiatrists, hospitals, medical capacity, and clinics projects ominous outcomes of Syrian mental health.
Participants with moderately severe 684 (17.2%) and severe 486 (12.2%) depression, and severe 679 (17.0%) anxiety warrant active treatment with psychotherapy and/or medications. In 2005 the health expenditure per capita was US$58. This is very low in comparison with the UK (where the health expenditure per capita was US$2900 in 2005) [20]. As the country is drowning in debts from the effects of the rampant war, the health expenditure per capita is likely to be significantly lower. In 2013, The World Federation for Mental Health (WFMH) declared a call for action on the mental health consequences of the manifold emergency in Syria. One of WFMH concerns is the neglect of trauma created by violence and disruption. The WHO, major humanitarian organizations, and the Syrian government that has not prioritized mental health have been urged by WFMH to consider the serious immediate and longterm mental health impacts of continuing armed conflict.
Extreme poverty, accounting for 89% of the population has drastic effects on mental health [8]. A recent study (April of 2020) conducted at the same institution reported the prevalence of poor and moderate economic status among participants as 6.9% and 34.8% respectively [21]. This study revealed 10.4% and 38.1% have a poor to moderate economic status showing an increase in poverty over the space of only a month. The Syrian government is suffering a prolonged economic recession where the Syrian Pound (SYP) volatile exchange rate reflects the destruction of the economic foundations [5]. Many Syrians have either lost or are at risk of losing their income due to job cuts during the draconian lockdown, leaving millions of families facing economic turmoil. Mental illness is significantly associated with chronic diseases where depression is found to occur in cancer (40%), diabetes (27%), cerebrovascular (23%), and cardiovascular (17%) patients [22-24]. This study revealed that 2818 (70.6%), and 2317 (58.1%) participants with chronic disease(s) reported depressive and anxiety symptoms. These findings are by a Turkish study [16].
Multivariable logistic regression analyses revealed that risk factors related to depression and anxiety, and found that: females, age of 18-25, students, and chronic diseases(s) were highly associated with depressive and anxiety symptoms. This is done by a Turkish and Chinese study [16,25]. Our study revealed that living in an urban area in comparison with a rural one was not significantly associated with depressive and anxiety symptoms and this is not by Turkish study [16]. The incidence of depression and anxiety is more common among chronically ill patients [26]. Individuals with chronic disease(s) are risk factors for depressive and anxiety symptoms as chronically ill patients are at increased risk of COVID-19 infection, which can be severe, lead to complication, and mortality [27]. Young adults (18-25 years), who were once children during this war, have grown up knowing but destruction and displacement. Grave violations of children’s rights-abductions, rape, killing and maiming continue unabated. Approximately 6 million Syrian children have been born since the crisis began, growing up knowing nothing but war, terror and displacement [28,29]. Prolonged lockdowns harmed society, many people were unemployed, schools and universities closed, and hyperinflations, constitute the spread of mental health disorders among younger generations. The Syrian government is trying to develop modern psychiatric care by encouraging the establishment of community-based services and cooperating with private sectors for the delivery of health care services. Syria is opening its market to some private insurance companies, which may have beneficial effects on the development of mental health services [20].
Limitation
Several limitations are present within this study. First, our findings can only be generalized about well-educated Syrians of good socio-economic status. Elderly and rural residents that have limited access to the internet are more likely to exhibit symptoms associated with depression and anxiety, as the elderly have a higher prevalence of chronic diseases and rural residents have endured severe impacts of war. Second, self-reporting has certain limitations compared with interviews. Third, the crosssectional state of study does not track the longitudinal follow up, management, and efficacy of psychological services. Fourth, further investigation is required to determine the correlation of depression and anxiety with causation. Fourth, a cross-sectional study is required to determine the prevalence of fear, insomnia, and distress during the COVID-19 pandemic among Syrians.
Conclusion
When the conflict and pandemic ends, what remains of the mental health services will be grossly insufficient to meet the predicted care needs of the Syrian population. Our study revealed a shockingly high prevalence of depression and anxiety during a time of war and pandemics. Syrians of female gender; age group of 18-25 years; occupation in private, business, and other sectors, as well as students; economic status of poor, moderate, and good; and having a chronic disease(s), were factors significantly associated with depressive and anxiety symptoms. It is therefore of the utmost importance to highlight the need to improve the deteriorating mental health services during these stressful events, increasing mental health awareness by providing campaigns, decrease stigma stigmatization towards mental health diseases and psychiatrists, encourage individuals to seek help and not feel ashamed, correct terminology within society, assess psychiatric management and protocols. The government must include mental health care in Syria's primary health care system, provide aid and support for mental health care workers, activate hotlines and online consultations, encourage individuals to seek counselling and reach out for help. We call on national and international organizations to address these needs to reconstruct mental health services and to assist in providing skilled health care workers for the suffering people of Syria.
Acknowledgements
We are thankful to the management of the Syrian Private University for its support in the field of medical training and research. We are thankful to everyone who participated in this study.
Funding
Syrian Private University did not fund this study. No other funding sources.
Availability of Data and Materials
All data related to this paper’s conclusion are available and stored by the authors. All data are available from the corresponding author on a reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) at the Syrian Private University (SPU). All Participants confirmed their written consent by answering a yes-no question. Participation in the study was voluntary and participants were assured that anyone who was not inclined to participate or decided to withdraw after giving consent would not be victimized. All information collected from this study was kept strictly confidential.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
F Mohsen and B Bakkar conceptualized the study, participated in the design, wrote the study protocol, performed the statistical analysis, did a literature search and drafted the manuscript. SM participated in statistical analysis. DM, SA and YL did a literature search and revision of the draft. All authors read and approved the final draft.
References
- Frounfelker R, Evelyn. JB, Bruffaerts. R, et al. Civilians in World War II and DSM-IV mental disorders: results from the World Mental Health Survey initiative. Soc Psychiatry Psychiatr Epidemiol. 2018; 53(2):207-9.
- Du L, Chen YM, Li Y, et al. Prevalence of depression during the SARS, MERS, and COVID-19 pandemics: A protocol for overview of systematic reviews. Medi. 2020;99(38): e22235.
- WHO. Coronavirus Disease 2019 (COVID-19): situation report. 2020; 130
- McKernan B. Syria confirms first Covid-19 case amid fears of catastrophic spread. The Guardian. 2020; 23.
- Affairs, OCHA, WHO, Syrian Arab Republic: COVID-19 Humanitarian Update No.09.2020.
- Salari N, Jalali R, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57.
- WHO. Depression and other common mental disorders: global health estimates. World Health Organization. 2017
- Hedar M. Mental health during the Syrian crisis: How Syrians are dealing with the psychological effects. Int Rev Red Cross. 2017; 99:927.
- Abou Saleh M, Mobayed M. Mental health in Syria. Int Psych. 2013;10(3):58-60.
- Hendrickx M, Woodward A, Fuhr DC, et al. The burden of mental disorders and access to mental health and psychosocial support services in Syria and among Syrian refugees in neighboring countries: a systematic review. J Public Health (Oxf). 2020;42(3):e299-e310
- Sawaya H, Atoui M, Hamadeh A, et al. Adaptation and initial validation of the Patient Health Questionnaire-9 (PHQ-9) and the Generalized Anxiety Disorder-7 Questionnaire (GAD-7) in an Arabic speaking Lebanese psychiatric outpatient sample. Psych Res. 2016;239:245-52
- Al Hadi AN, Al Ateeq DA, Al Sharif E, et al. An arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psych. 2017;16:32.
- Kocalevent RD, Hinz A, Brähler E. Standardization of the depression screener Patient Health Questionnaire (PHQ-9) in the general population. Gen hospital psych. 2013; 35(5):551-55.
- Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266-74.
- World Health Organisation (WHO). Coronavirus disease (COVID-19): situation report.2020;103.
- Özdin S, Özdin SB. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psych. 2020;66(5):504-11
- Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40-48.
- Nations U. Policy brief: COVID‐19 and the need for action on mental health. 2020.
- World Health Organisation (WHO). Syrian Arab Republic-Global Cancer Obsetvatory. 2019.
- Assalman I, Alkhalil M, Curtice M. Mental health in the Syrian Arab Republic. Int Psychiatry. 2008; 5(3):64-66.
- Mohsen F, Bakkar B, Armashi H, et al. A crisis within a Crisis: COVID-19 knowledge and awareness among the syrian population-A National Survey Assessment. BMJ open. 2020
- Control CFD, and prevention, Mental health and chronic diseases CDC fact sheet. 2012;2.
- American Heart Association. Depression and Heart Health Web Site. 2018.
- Lasser K, Boyd JW, Woolhandler S, et al. Smoking and mental illness: A population-based prevalence study. Jama. 2000;284(20):2606-610.
- Wang Y, Junjie Y, Wei W, et al. Study on the public psychological states and its related factors during the outbreak of Coronavirus Disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2020:1-10.
- Gerontoukou EI, Michaelidoy S, Rekleiti M, et al. Investigation of anxiety and depression in patients with chronic diseases. Health Psychol Res. 2015;3(2):2123.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-62.
- Yayan EH, Düken ME, Özdemir AA, et al. Mental Health Problems of Syrian Refugee Children: Post-Traumatic Stress, Depression and Anxiety. J Pediatr Nurs. 2020;51:e27-e32.
- Unicef, Syrian crisis after nine years of conflict, children continue to pay the heaviest price. Unicef. 2020.