Research Article - Journal of Gastroenterology and Digestive Diseases (2017) Volume 2, Issue 1
Democratic republic of Congo minister of public health congregation of the sisters of the poor of Bergamo.
- *Corresponding Author:
- Mukwela J
Clinician Researcher Manager in Public Health Congo
Tel: +243815359629
E-mail: j.mukwela.saco@gmail.com
Accepted date: March 14, 2017
Citation: Mukwela J, Kitambala G, Baba I, et al. Democratic republic of Congo minister of public health congregation of the sisters of the poor of Bergamo. J Gastroenterol Dig Dis. 2017;2(1):13-17.
Abstract
Monitoring sentinel of diarrhoea a rotavirus in the site of hospital complex pediatrique of Kingasani II 2009-2014 by the team of Jean Mukwela, Kitambala, Cleidia, Masungi, Kibaka, Emonmey, Baba, Katembo, Lubi, Lupwenge, Belerheine.
Keywords
Monitoring, Diarrhea, Rotavirus, Meningitis, Malaria, Respiratory, Infections, Gastroenteritis, Elisa, Pediatrics, Saddles, Samples.
Introduction
After malaria, respiratory infections, and meningitis, severe diarrhea is also one of the major causes of public health problems worldwide. According to current WHO statistics, this disease causes at least 483,000 deaths of children from zero to 59 months a year in the world.
Given this dramatic statistic, we raise the alarm bell at all levels and advocate for the rapid introduction of the new vaccine in Rotavirus throughout the world and particularly in the DRC. In 2009, the DRC's Ministry of Public Health, with the support of its partners, set up a study on the incidence of this disease with the adoption of three sentinel sites: the pediatric hospital of Kingasani II, and the pediatric hospital of Kalembe-Lembe for the Kinshasa pool, and the Sendwe hospital of Lubumbashi. This choice was made on the basis of expertise and specialty of care for sick children [1-3].
General Objective
The objective defined in our study is to monitor the circulating strains of rotavirus diarrhea at the Kingasani II pediatric hospital in Kinshasa in order to ensure adequate prevention and care.
Methodology
This is a retrospective exploratory study. The technique used is that of a direct interview with the parents of sick children. That is to say, we searched for them with the additional information before referring to the nursing staff for the cases recorded. The targets of our surveillance are the children from 0 to 59 months taken care of during our investigation period within this hospital center [3-6].
The population of this health area is 236,584 inhabitants whose children who suffered from diarrhea in Rotavirus account for 55%.
Sample
Given that the target population is the set of individuals concerned by the objective of scientific research, our sample is composed of 1204 children aged 0 to 59 months and taken in care following this disease.
Inclusion criteria
Unit of study: Be a sick child aged 0 to 59 months, hospitalized in the pediatric department for gastroenteritis in our structure. Be suffering from gastroenteritis of less than 7 days.
Exclusion criteria
Any child over 5 years of age; Child over 59 months hospitalized for gastroenteritis with diarrhea beyond 7 days.
Any child hospitalized for other pathologies than gastroenteritis.
Any child at the age of inclusion whose stool sample was not taken during hospitalization.
Gastroenteritis in malnourished children. Malnourished children were excluded from our study by the fact that they have a problem of malabsorption which modifies the structure of the intestinal mucosa preventing Rotavirus which is an enterocytes, hence the difficulty of finding these germs in the saddle a malnourished child.
Results
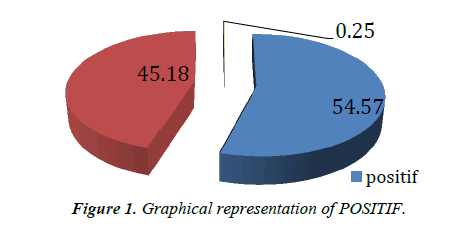
During the last five years, monitoring of Rotavirus has progressed in our Kingasani II Pediatric Hospital by simply collecting stool specimens and the ELISA assay, as well as motivated and trained staff Site can explain this success. Since August 2009 until December 2014, we have recorded 1204 cases of severe acute diarrhea. All of these stool samples were collected and analyzed by an immunoassay for Rotavirus, and 656 samples were positive (55%). Of 1204 cases of Rotavirus diarrhea analyzed in our department, we found that 656 cases were confirmed positive, 54.8%, 544 negative cases or 45.1%; And 3 cases had an indeterminate result of 0.25%.
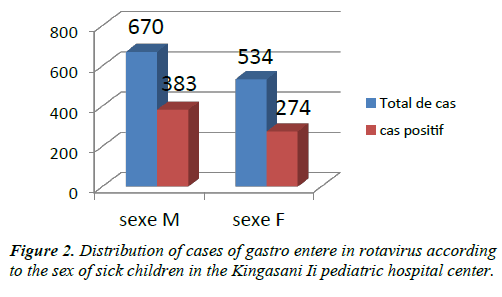
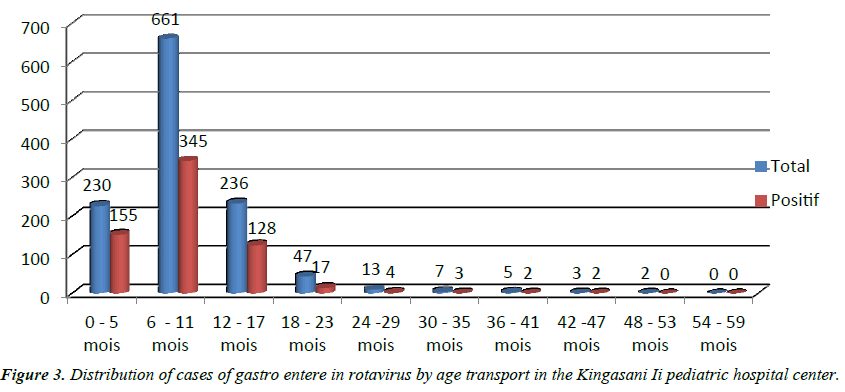
There was a distribution of cases of Rotavirus gastroenteritis according to sex in the Kingasani II pediatric hospital. Age distribution showed that positive cases of severe acute gastroenteritis were more common in children aged 0 to 17 months, with 155 cases positive for 0 to 5 months, 345 for 6 to 11 months and 128 for the age range of 12 to 17 months. The predominance of sick children is male [6-9].
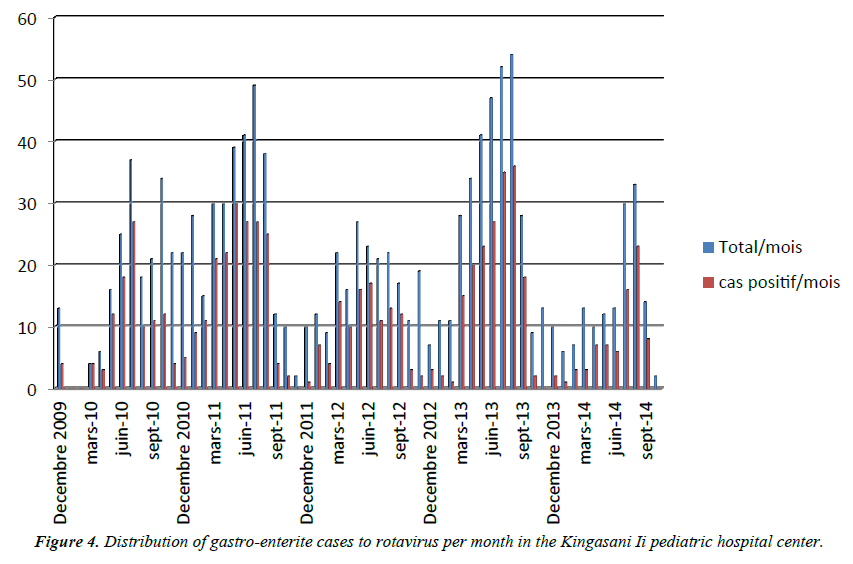
Determination of seasonality and experience showed that during the dry season (May, June, July) many cases of Rotavirus diarrhea were recorded, as during the dry season the climate is cold at Kinshasa especially at Kingasani and the wind blows from 6 am to 3 pm causing a strong viral permutation on both sides.
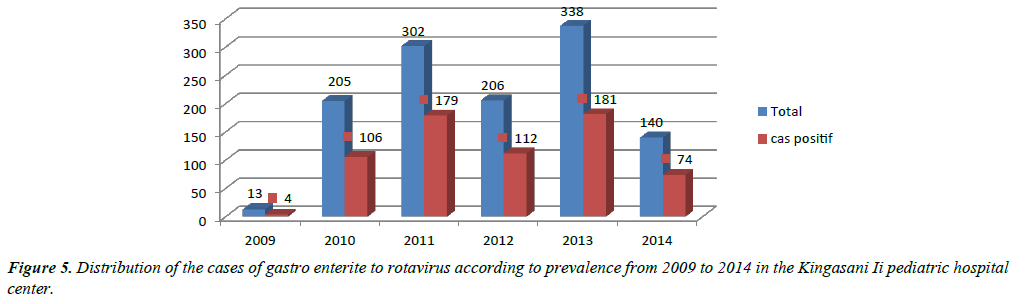
We note that in 2009 the center had recorded 30.8% of cases of diarrhea in Rotavirus, in 2010 the score achieved was 51.7%, while in 2011 the figure increased to 59.3% Lower in 2012 to 54.4% then a slight reduction in reduction in 2013 with 53.4% of cases and in the end 52.9% in 2014 (Figures 1-5).
The country's policy requires that children be properly rehydrated according to the dehydration plan and the citizens [9-12].
His medical care was realized: zinc 10 mg/day for children under 6 months. 20 mg/day for children over 6 months. Recall that we are waiting for vaccine which is very important because Rotavirus often reaches people who have defective immunity yet at age <2 years, children have it and constitutes a group at risk.
Support strategies
Used following an evaluation conducted by the Ministry of Public Health through its Expanded Program on Immunization (EPI). The maintenance of the Pediatric Hospital of Kingasani II is justified by the very marked expertise because it receives many patients given the geographical position of which it occupies. This center is the only one of its kind in that it is located in the most populated commune of the city of Kinshasa with equipment set up, including a focal point composed of clinicians, medical biologists and databases.
The Expanded Program on Immunization supervises surveillance activities in collaboration with the national institute for biological research (INRB). WHO, CDC and the Bill and MELINDA GUET foundation within the SURVAC project [12-15].
Monitoring resources and data from this operational unit are managed by a coordinator at the sentinel site. The site laboratory works in close collaboration with the national laboratory (INRB), the regional reference laboratory, WHO of Mendusa University, Limpopo, and the CDC Atlanta World Laboratory, which support genotyping, sequencing and Quality control examinations [15-20].
This center has a laboratory with a virology department especially for monitoring Rotavirus because it records several cases per month. To confirm the diagnosis of Rotavirus infection, we used two tests and are always recommended for surveillance. The ELISA is carried out in our reference or regional site with a quality control carried out by INRB. The PCR for genotyping is conducted at the national reference laboratory (NRL) of INRB, Kinshasa/DRC, at the regional reference laboratory (RRL) of MENDUSA University, and at the CDC global reference laboratory (GRL) Atlanta, USA. Clinicians who are members of the site identify the patients and complete an investigation form for each case admitted with severe acute diarrhea. This form is completed at the site laboratory with all test results and then returned to the clinicians for patient follow-up until discharge, then sent to the manager for compilation and re-sent to the expanded immunization program managers (EPI), the national institute for biological research (INRB), and the WHO where the analysis is carried out at each level.
Discussion
We affirm that from 2009 to 2014 there was surveillance of Rotavirus infection of positive ELISA in our Kingasani II pediatric hospital, all cases of severe acute diarrhea in children aged 0 to 59 months hospitalized in We had more than 50% compared to the rest of the recorded cases.
In our Kingasani II pediatric hospital, this sentinel surveillance for Rotavirus had started in 2009 in August as the rest of the sentinel sites. However, from there until October 2014, we recorded 1204 cases of acute gastroenteritis and these cases were included in the data recorded in the national surveillance system.
In relation to the periodicity, the most frequently reported months of transmission to this very deadly infection at Kingasani, are determined from April, May, June, July and August of each year because these are the months that characterize the season dry to which the viral mutation is very growing and active contrary to the remainder of months. This led us to confirm once again that seasonality plays a very important role in reporting cases of gastroenteritis in Rotavirus in Kinshasa [21,22].
Stankler said, explains that the higher intake of Rotavirus diarrhea infection causes more mortality in children 0 to 59 months. The results obtained in our study showed that in the Democratic Republic of Congo. There is a wide variety of circulating strains of Rotavirus, which changes over time.
The analysis done by Tsuboi, proves that genotyping done in the MENDUSA regional laboratory in South Africa detected the higher strains of P [8], G2P6 and from 2009 to 2014. Wasmuth studied Rotavirus around the world estimating that about half of the hospitalizations for diarrhea in pediatric wards is attributable to this virus. This corresponds practically to our results of this study of which all the children have an episode of gastroenteritis in Rotavirus and the majority of the children have about 5 Rotavirus infections before the age of 5 years and that with the number, the severity of the episodes of diarrhea is less.
Thus, at the age of 5, each child will have had an episode of diarrhea due to Rotavirus, 1 in 5 children will need a visit to a medical center, 1 in 65 will have Hospitalized and 1 in 293 will die due to Rotavirus, our surveys have found it in the prevalence results .
Rotavirus gastroenteritis is a disease that also affects children in developing countries, this assertion to share similar opinion to our study by the fact that the Kingasani neighborhood being very concentrated with a population more than the remains of the neighborhoods In the capital of Kinshasa, there is a very remarkable rural exodus, each of which brings with its culture and the notion on the management of waste is questioned. On the one hand we see that people having nothing to do are no longer doing small businesses to guarantee their survival selling mainly open-air food, on the other hand we notice the lack of supervision of children because remember Here that the mother daughters are numerous in this corner of the capital and whose notion on the planning of the births is problematic. The incidence of gastroenteritis in Rotavirus by age group is similar among children in developing countries and those in industrialized countries. On the other hand, inequality in access to care increases the severity of infections and its consequences in developing countries, where Rotavirus gastroenteritis is an important cause of infant mortality and this is verifiable in our results.
Conclusion
In our study, 55% of children hospitalized for severe rotavirus diarrhea are those whose age ranged from 0 to 59 months, this is attributed to a Rotavirus infection. The results demonstrate the need to introduce the Rotavirus gastroenteritis vaccine in our country to help reduce the high prevalence and mortality rate of children aged 0-59 months without ignoring deaths due to this disease.
Given that seasonality constitutes the high period of Rotavirus diarrhea cases, it is necessary to introduce the vaccine in order to have a synchronization with total coverage throughout the country. This could lead to mastery in record time and to eradicate the disease nationwide, see the Kingasani II Pediatric Hospital. Although biases are often reported, such as better family attention for the breast-fed child or more frequent or prolonged nursing stays of bottle-fed infants, this preventive effect is not discussed. There was also a strong correlation between the duration of breastfeeding and the lowest incidence of infectious diarrhea. Exclusive breastfeeding for a period of 6 months significantly reduces the risk of acute diarrhea during the first year of life compared to 3 months of breastfeeding.
The prolongation of breastfeeding beyond the age of 6 months does not seem to increase the preventive effect. This effect may be only transitory; The infectious risk being delayed at a later age. It would then be less. The preventive effect for acute diarrhea of partial breastfeeding is difficult to analyze in the absence of significant data available; It probably depends on the amount of milk intake.
The natural infection does not protect against reinfection, but protects the infant from severe disease during reinfection. It is legitimate to wait until the efficacy of RV vaccines in terms of protection is comparable to that of natural infection. The aim of this vaccination is therefore to prevent the occurrence of severe acute gastroenteritis due to RV in infants under two years of age. This vaccination must be effective not only against the three most frequent serotypes of RV in the world.
Acknowledgement
Our most sincere thanks go to the congregation of the sisters of the poor in Bergamo for the superior sister CLELIA SUDIRO RENATA for her personal involvement in the supervision activities of our institution.
We would like to thank the WHO team in the person of: Dr Adolph Kongolo, Vital Mondonge and Mr Albert Mbule who despite their multiple occupations are concerned to frame the best result of this study.
It will be very ungrateful for us not to acknowledge the heavy contribution of our different actors in their respective titles and qualities, for having participated in full for this study to be born this is the team whose names mentioned above. Our gratitude is due to the various INRB authorities, notably Professor Muyembe, Mrs Berth Miwanda, Ms Elie Pukuta and Mr Jean Claude Tshanga Tshanga but for their wonderful supervision. Finally, we would like to pay homage to Mrs Diane Wanku, Mrs Lila Ralison, Mr Mathieu, whom we would not be ungrateful if we finish this exhibition without alluding to their very commendable expertise.
References
- http://www.mrcgene.com/tri.html.
- http://www.proteinatlas.org/.
- Amuli JP. Methodology in scientific research, ISTM / KINSHASA.Web Design. 2014.
- Stankler L, Pollitt RJ, Gray ES, et al. An unexplained diarrhoea and failure to thrive in 2 siblings with unusual facies and abnormal scalp hair shafts: A new syndrome. Arch Dis Child. 1982.
- Synowsky SA, Heck AJ. The yeast Ski complex is a hetero tetramer. ProteinSci. Saccharomyces cerevisiae. 2008.
- Tomecki, R, Kristiansen MS, Lykke-Andersen S, et al. Conserved functions of yeast genes support the duplication, degeneration and complementation model for gene duplication. 2010.
- Tsuboi T, Kuroha K, Kudo K, et al.Plays a general role in quality control by dissociation of a stalled ribosome at the 3rd end of aberrant mRNA. Mol Cell. 2012;46(4):518-29
- Verloes A, Lombet J, Lambert Y, et al. Gosseyef further delineation of a distinct syndrome with neonatal hemochromatosis phenotype, intractable diarrhoea, and hair anomalies. Am J Med Genet. 1997.
- Vodkin M, Katterman F, Fink GR. Yeast killer mutants with altered doublestranded ribonucleic acid. J Bacteriol. 1974; 117(2):681-6
- Wan J, Yourshaw M, Mamsa H, et al. Mutations in the RNA exosome component gene EXOSC3 cause neurodegeneration. Nat Genet. 2012; 44:704-708.
- Wang J, Cortina G, Wu SV, et al. Mutant neurogenin-3 in congenital malabsorptive diarrhoea. N Engl J Med. 2006;355(3):270-80.
- Wang L, Lewis MS, Johnson AW. Domain interactions within the Ski2/3/8 complex and between the Ski complex and Ski7p. 2005;11(8):1291-302.
- Wang X, Jia H, Jankowsky E, et al. Degradation of hypomodified.2008;14(1):107-16.
- Wasmuth EV, Lima CD. Exosomes are dependent on the noncatalytic core and central channel. Exotics and endoribonucleolytic activities of yeast cytoplasmic and nuclear RNA. 2012.
- Widner WR, Wickner RB. Evidence that the SKI antiviral system of Saccharomyces cerevisiae acts by blocking expression of viral. 1993;13(7):4331-41
- Witharana C, Roppelt V, Lochnit G, et al. Heterogeneous complexes of the RNA exosome in Sulfolobus soil fataricus.Bio chemistry. 2012.
- Wolfe JF, Adelstein E, Sharp GC. Antinuclear antibody with distinct specificity for polymyositis. J Clin Invest. 1977;59:176-8
- Wolski SC, Kuper J, Kisker C. The XPD helicase: XPanDing archaeal XPD structures to get a grip on human DNA repair. Biol Chem. 2010;391(7):761-5
- Xu C, Min J. Structure and function of WD40 domain proteins. 2011;2(3):202-14
- Yang CT, Hindes AE, Hultman KA, et al. Mutations in gfpt1 and skiv2l2 cause distinct stage-specific defects in larval melanocyte regeneration in zebrafish. 2007; 3(6):88
- Yang XF, Wu CJ, Chen L, et al. CML28 is a broadly immunogenic antigen, which is overexpressed in tumor cells. Cancer Res. 2002;62(19):5517-22.
- Zhao X, Yu YT. Incorporation of 5-fluorouracil into U2 snRNA blocks pseudouridylation and pre-mRNA splicing in vivo. Nucleic Acids Res. 2007;35(2): 550-8.